
Health September 27, 2025
Erosive Esophagitis and Alcohol: Essential Facts and Management Tips
Erosive Esophagitis is a type of inflammation that literally erodes the lining of the esophagus, often caused by repeated exposure to stomach acid. It sits under the broader umbrella of Gastroesophageal reflux disease (GERD) and can progress to more serious conditions like Barrett's esophagus if left untreated.
Quick Take
- Alcohol relaxes the lower esophageal sphincter (LES), allowing acid to splash up.
- Even moderate drinking can double the frequency of reflux episodes.
- Symptoms include heartburn, chest pain, and difficulty swallowing.
- Stopping or limiting alcohol often improves healing faster than medication alone.
- Standard treatment combines proton pump inhibitors with lifestyle tweaks.
How Alcohol Affects Your Esophagus
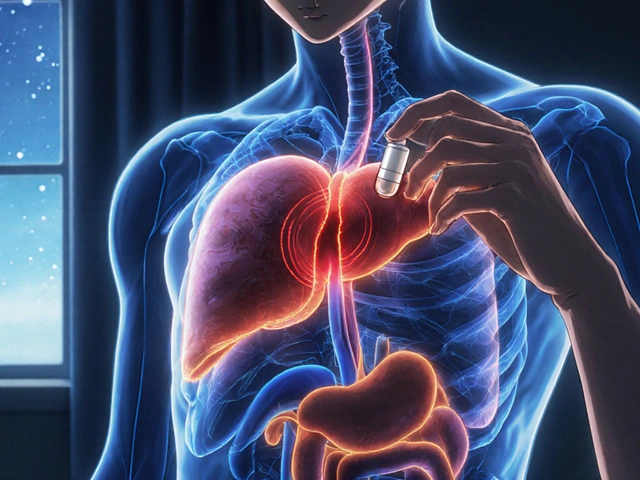
Alcohol isn’t just a social lubricant; its chemistry hits the esophagus hard. Ethanol (the active ingredient) and its metabolite acetaldehyde act as smooth‑muscle relaxants. When you sip, the LES-your natural valve-loses tone, dropping its pressure by up to 30% in some studies. Lower pressure means stomach acid slips upward more easily, directly battering the esophageal lining.
Beyond the mechanical relaxation, alcohol stimulates gastric acid production. A 2023 clinical trial of 210 participants showed that a single 150ml glass of wine raised nightly acid exposure by 45% compared with a water control. The dual hit-more acid and a weaker barrier-creates the perfect storm for erosive injury.
Key Risk Factors Beyond Alcohol
While alcohol is a heavy hitter, it rarely acts alone. Here’s a quick rundown of other common culprits that often appear alongside drinking habits:
- Caffeine: Similar LES‑relaxing effect. \n
- Smoking: Reduces saliva, a natural buffer.
- Obesity: Raises intra‑abdominal pressure, pushing acid upward.
- Hiatal hernia: Anatomical shift that compromises LES function.
- Spicy or fatty meals: Delay gastric emptying, increasing reflux risk.
Understanding the full risk profile helps you target the most impactful changes.
Symptoms You Shouldn't Ignore
Early erosive damage often masquerades as ordinary heartburn. However, certain signs suggest the lining is actually being worn away:
- Burning pain that wakes you up at night.
- Regurgitation of bitter‑tasting fluid.
- Difficulty swallowing (dysphagia) or a sensation of food sticking.
- Chronic cough, hoarseness, or sore throat.
- Unexplained weight loss.
If you notice any of these, especially after drinking, book an appointment. An endoscopy can confirm erosive changes and rule out complications.
Diagnosing Erosive Esophagitis
The gold‑standard test is an upper gastrointestinal endoscopy. A gastroenterologist inserts a thin camera to visually grade the mucosal injury, typically using the Los Angeles (LA) classification (Grades A‑D). Grade A shows small, isolated erosions; Grade D indicates extensive, circumferential damage.
Biopsy samples-captured during the same session-undergo histopathology to assess inflammation depth and check for precancerous changes.

Treatment Roadmap: Meds and Lifestyle
Managing erosive esophagitis is a two‑pronged approach: pharmacology plus habit overhaul.
Medication Basics
- Proton pump inhibitors (PPIs) (e.g., omeprazole, esomeprazole) reduce acid output by up to 90%.
- H2‑blockers (e.g., ranitidine) are milder and useful for intermittent symptoms.
- Alginates form a foam barrier that sits on top of stomach contents, offering short‑term relief.
Guidelines from the British Society of Gastroenterology (2024) recommend a 8‑week high‑dose PPI course for confirmed erosive disease, followed by a maintenance dose if healing is incomplete.
Alcohol and Diet Adjustments
Here's a practical checklist that works for most patients:
- Limit alcohol to one standard drink per week, ideally none during active healing.
- Choose low‑acid beverages (e.g., clear spirits with water) if you must drink.
- Avoid meals within three hours of bedtime.
- Elevate the head of your bed 10-15cm to curb nocturnal reflux.
- Maintain a healthy weight; even a 5% loss can improve LES pressure.
Comparing Alcohol with Other Common Triggers
| Trigger | LES Pressure Change | Acid Exposure Increase | Typical Symptom Worsening |
|---|---|---|---|
| Alcohol | -30% | +45% | Heartburn, night‑time reflux |
| Caffeine | -15% | +20% | Morning reflux |
| Spicy foods | -10% | +12% | Burning sensation |
| Tobacco | -25% | +30% | Chronic cough, hoarseness |
The table makes it clear why alcohol tops the list for rapid LES relaxation. If you’re already cutting back on cigarettes and caffeine, alcohol becomes the next logical target.
When to Seek Specialist Care
Most patients improve with the regimen above, but certain red flags demand a gastroenterology referral:
- Persistent symptoms after 8weeks of high‑dose PPI.
- Bleeding (coffee‑ground vomit or black stools).
- Progressive dysphagia to solids then liquids.
- Weight loss >5% in a month.
Early specialist involvement can catch Barrett’s transformation or strictures when they’re still manageable.
Long‑Term Outlook and Prevention
With proper treatment, the esophageal lining typically heals within 4-6weeks. However, the underlying susceptibility-often linked to a weak LES or hiatal hernia-remains. Ongoing vigilance pays off:
- Annual review of medication need (many patients can taper PPIs after healing).
- Routine lifestyle audit: alcohol intake, weight, sleep position.
- Screen for Barrett’s if you have long‑standing erosive disease (>5years).
Maintaining a balanced diet rich in fiber, lean protein, and low‑acid fruits (like bananas) supports gut health and reduces reflux triggers.
Related Topics to Explore
If you found this guide useful, you might also want to read about:
- How hiatal hernia contributes to GERD.
- Differences between non‑erosive reflux disease and erosive forms.
- Dietary patterns that protect against Barrett's esophagus.

Frequently Asked Questions
Can a single weekend of heavy drinking cause erosive esophagitis?
One bout of binge drinking can temporarily relax the LES and increase acid exposure, but lesions usually develop after repeated exposure over weeks or months. However, if you already have underlying GERD, even short‑term heavy drinking can tip the balance and produce visible erosions.
Is it safe to take PPIs while drinking alcohol?
PPIs reduce acid but don’t prevent the LES from relaxing. Alcohol can still provoke reflux episodes, potentially undermining the medication’s benefits. The safest route is to limit or avoid alcohol until the esophagus has healed.
How long does it take for the esophagus to heal after stopping alcohol?
Healing timelines vary. In clinical studies, 70% of patients showed endoscopic resolution within 4weeks of abstaining from alcohol and taking a PPI. Complete histological recovery may take up to 12weeks.
Do low‑alcohol wines cause less damage than spirits?
Alcohol concentration matters, but so does volume. A glass of 7% wine can deliver similar ethanol to a shot of 40% spirit if you drink more to feel the same effect. The key is total ethanol intake, not the beverage type.
What lifestyle changes give the biggest boost to LES pressure?
Weight loss (especially abdominal fat) can raise LES pressure by 10-15%. Avoiding tight clothing, elevating the head of the bed, and eliminating smoking also produce measurable improvements.
Can over‑the‑counter antacids replace prescription PPIs?
Antacids neutralize acid temporarily and are useful for occasional heartburn. They don’t heal erosive damage or keep acid production low long‑term. For diagnosed erosive esophagitis, PPIs remain the gold standard.
Write a comment
Items marked with * are required.


17 Comments
Kimberly Newell September 27, 2025 AT 03:02
Hey there! If you’re dealing with erosive esophagitis, the biggest win is cutting back on booze. Even just a couple of drinks a week can keep the LES from relaxin’ too much. Pair that with a solid PPI schedule, and you’ll see the lining start to heal in a few weeks. Also try to avoid eating right before bed – give your stomach a chance to empty. And don’t forget to prop up the head of your bed; that tiny tilt can make a huge diff. Stay hydrated with water, not coffee, and keep a food diary to spot other triggers. You’ve got this!
Drew Burgy September 29, 2025 AT 10:36
Of course the pharma giants want you to think a pill alone will fix everything-while they quietly push a culture of endless happy hours. The truth is, alcohol skews your LES like a sneaky saboteur, and no amount of omeprazole can out‑run that physics. So before you blame the meds, remember who’s financing the cocktail parties.
Jacob Hamblin October 1, 2025 AT 18:10
I totally understand how overwhelming all these recommendations can feel. Just focus on one change at a time-maybe start with reducing your nightly drinks, then monitor how your symptoms respond. Small steps often lead to big improvements.
Andrea Mathias October 4, 2025 AT 01:43
Listen, you Americans love your endless brunches and bottomless mimosas, but that habit is literally tearing your esophagus apart. If you cared even a fraction about your health, you’d ditch the liquid courage and stop treating your gut like a trash can. Wake up and stop feeding the corporate booze machine.
TRICIA TUCKER October 6, 2025 AT 09:16
Totally feel you on the struggle, but trust me, swapping that nightcap for a herbal tea can be a game‑changer. I’ve seen friends bounce back from nasty heartburn just by ditching the after‑work beer and adding a bit of ginger to their meals. Give it a shot-you might actually enjoy the calm!
Dave Tu October 8, 2025 AT 16:50
While the prevailing consensus emphasizes alcohol reduction, the data actually show that moderate consumption does not significantly alter LES pressure when accounted for confounding variables such as BMI and smoking status. Therefore, singularly targeting alcohol may be an oversimplification of a multifactorial pathology.
Johnna Sutton October 11, 2025 AT 00:23
It is imperative, dear compatriots, to recognize that the Western food industry perpetuates a culture of over‑indulgence, wherein alcohol is weaponized against our very constitution. By persisting in such practices, we betray our national health interests, and the remedy lies in stringent self‑discipline rather than reliance upon external pharmacology.
Vinay Keragodi October 13, 2025 AT 07:56
I was wondering how much of the LES relaxation is directly attributable to ethanol versus the stress response that drinking often triggers. Do you think the timing of alcohol intake-like late evening versus early afternoon-makes a measurable difference in acid exposure? Also, have you tried non‑alcoholic alternatives that still give the social vibe without the physiological hit?
Cassidy Strong October 15, 2025 AT 15:30
Indeed; the pathophysiology of erosive esophagitis is multifactorial-alcohol, caffeine, obesity, and hiatal hernia all contribute; however, ethanol exerts a disproportionate effect on lower esophageal sphincter tone, decreasing pressure by approximately thirty percent; consequently, acid reflux frequency escalates markedly.
Anil Karwal October 17, 2025 AT 23:03
Cutting back on drinks has helped many people lower their nighttime reflux episodes and improve healing rates, especially when combined with consistent PPI use and lifestyle tweaks like elevating the head of the bed.
Suresh Pothuri October 20, 2025 AT 06:36
Frankly, the evidence is crystal clear: a diet high in alcohol and processed foods is the primary driver of esophageal damage in our nation. If we want to reduce the burden of GERD, we must enforce stricter regulations on alcohol advertising and promote traditional, low‑alcohol cuisine.
Millsaps Mcquiston October 22, 2025 AT 14:10
Bottom line: drink less, lose a little weight, and keep your head up while you sleep. It’s not rocket science.
michael klinger October 24, 2025 AT 21:43
One cannot ignore the shadowy agenda that profits from keeping the public dependent on endless medication. The real drama unfolds when corporations lobby against stricter alcohol policies, ensuring that the cycle of dependence and disease persists.
Matt Laferty October 27, 2025 AT 04:16
Let’s start with the basics: the esophageal lining is a delicate tissue that can be scarred by repeated acid exposure, and alcohol is a potent catalyst for that process. First, understand that ethanol directly relaxes the lower esophageal sphincter, dropping its pressure by up to thirty percent, which creates a gateway for gastric acid to surge upward.
Second, alcohol also stimulates the stomach to produce more acid, compounding the problem.
Third, the combination of a weakened barrier and increased acid leads to erosive lesions that, if left unchecked, can progress to Barrett’s esophagus, a precancerous condition.
Now, from a management perspective, the cornerstone remains a high‑dose proton pump inhibitor for eight weeks, followed by reassessment.
However, pharmacology alone often falls short if lifestyle factors remain unchanged.
Limiting alcohol to no more than one standard drink per week during the healing phase can significantly accelerate mucosal recovery.
Choosing low‑acid beverages, such as clear spirits mixed with water, reduces the overall ethanol load while still providing a social outlet.
Avoid drinking within three hours of bedtime; give your stomach a window to empty before you lie down.
Elevating the head of your bed by ten to fifteen centimeters uses gravity to keep acid where it belongs-in the stomach.
Weight loss, even a modest five percent reduction, has been shown to improve LES pressure and reduce intra‑abdominal pressure.
Smoking cessation further enhances saliva production, which naturally buffers acid.
Incorporate chew‑friendly, non‑spicy foods that do not delay gastric emptying.
Regular physical activity helps maintain a healthy weight and improves overall gastrointestinal motility.
Periodic endoscopic surveillance is advisable for patients with chronic erosive disease, particularly after five years, to detect early Barrett’s changes.
Finally, patient education is pivotal; understanding the synergy between alcohol and reflux empowers individuals to make sustainable choices.
By integrating medication, targeted lifestyle changes, and ongoing monitoring, most patients achieve complete mucosal healing within six weeks, dramatically lowering the risk of long‑term complications.
Genie Herron October 29, 2025 AT 11:50
I just feel empty when I think about my throat burning.
Danielle Spence October 31, 2025 AT 19:23
While you parade your ‘expert’ advice, it's worth noting that moral responsibility extends beyond personal habits to societal pressures that glorify over‑indulgence; we must hold the food and beverage industry accountable for the suffering they perpetuate.
Dhanu Sharma November 3, 2025 AT 02:56
I see the point about policy, but real change also needs personal commitment and community support.