
Health October 13, 2025
Diabetes and Skin Infections: Essential Facts You Must Know
Diabetes Skin Infection Risk Assessment Tool
This tool helps you understand your personal risk of skin infections based on diabetes management and foot care habits. Results are for informational purposes only and should not replace professional medical advice.
Your Skin Infection Risk Assessment
Your risk level is Low
You're taking good steps to prevent infections. Continue your excellent diabetes management habits.
Key Takeaways
- High blood sugar weakens immunity, making skin more vulnerable.
- Common infections include cellulitis, staph abscesses, candidiasis, and fungal toe infections.
- Poor circulation and nerve loss hide early warning signs.
- Good glycemic control, daily skin checks, and proper foot care cut the risk dramatically.
- Seek medical help promptly if you notice rapid spreading redness, pus, or unexplained itching.
Understanding the link between diabetes skin infections can help you protect your health. People with diabetes often think of heart disease or kidney problems, but skin issues are just as common and can lead to serious complications if ignored.
How Diabetes Impacts Your Skin
Diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels that result from insufficient insulin production or insulin resistance. Persistent high sugar, known as Hyperglycemia, a condition where blood glucose remains above normal ranges, typically over 180 mg/dL after meals, interferes with several body systems that keep skin healthy.
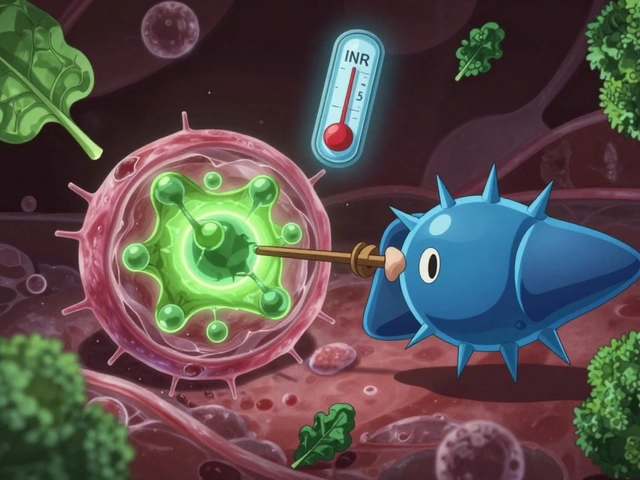
The Immune system the collection of white blood cells, antibodies, and signaling molecules that fight infections becomes less effective. White blood cells struggle to migrate to wound sites, and the ability to destroy bacteria drops by up to 30% in poorly controlled diabetes. At the same time, high glucose creates a sugar‑rich environment that feeds microbes.
Two other diabetes‑related problems directly affect the skin:
- Peripheral neuropathy damage to the nerves in the extremities, causing loss of sensation, especially in the feet makes it hard to notice minor cuts or moisture buildup.
- Poor circulation reduced blood flow caused by narrowed arteries, which slows healing and lowers oxygen delivery to skin prolongs infection recovery.

Common Skin Infections Linked to Diabetes
People with diabetes are prone to several types of skin infections. Below is a quick rundown of the most frequent culprits.
| Type | Typical Pathogen | Common Presentation | First‑line Treatment |
|---|---|---|---|
| Bacterial | Staphylococcus aureus a gram‑positive bacterium that thrives on skin | Red, warm, painful cellulitis; abscesses with pus | Oral or IV antibiotics (e.g., dicloxacillin) |
| Fungal | Candida albicans yeast that overgrows in moist, sugary areas | Itchy, moist rash in folds; white patches on nails | Topical azoles (clotrimazole) or oral fluconazole |
Cellulitis is a deep bacterial infection of the skin and sub‑cutaneous tissue, often caused by Staphylococcus aureus or Streptococcus pyogenes. In diabetics, cellulitis spreads faster and may lead to tissue death if not treated promptly.
Staph abscesses appear as painful, fluctuant lumps filled with pus. Because high glucose impairs neutrophil function, these abscesses can become larger before the body tries to contain them.
Candidiasis thrives between toes, under breasts, or in skin folds. The warm, moist environment plus excess sugar creates a perfect breeding ground. Look for bright‑red borders and a white, slightly greasy coating.
Fungal nail infections (onychomycosis) are especially stubborn in diabetic patients. The fungus invades the nail bed, causing thickening, discoloration, and sometimes pain when shoes rub against the nail.
Viral infections such as herpes simplex can also be more severe, but bacterial and fungal types account for the majority of cases.
Why Infections Occur More Frequently
Three main mechanisms explain the higher infection rate.
- Impaired immune response. Hyperglycemia disrupts chemotaxis, phagocytosis, and cytokine production. Even a modest rise in A1C from 7% to 9% can double the risk of skin infection.
- Reduced blood flow. Diabetes‑related atherosclerosis limits oxygen and nutrient delivery. Without adequate circulation, skin cells cannot regenerate quickly, giving microbes time to establish.
- Neuropathy and moisture. Nerve loss means you may not feel a small cut, blister, or sweaty foot. Moisture builds up inside shoes, softening skin and allowing fungi to proliferate.
Research from the UK Diabetes Trust (2024) showed that patients with an A1C above 8% were three times more likely to develop a foot ulcer that became infected compared with those maintaining an A1C below 7%.
Spotting the Signs Early
Because pain perception may be dulled, visual checks become crucial. Here’s what to look for:
- Redness that expands rapidly (often a sign of cellulitis).
- Swelling, warmth, and tenderness around a cut or ulcer.
- Pus, drainage, or a foul smell - indicates bacterial invasion.
- Itching, burning, or a white‑creamy rash in skin folds - typical of candidiasis.
- Thickened, discolored toenails that crumble under pressure.
Any of these signs combined with a fever over 38°C (100.4°F) warrants immediate medical attention.

Prevention Strategies for People with Diabetes
Glycemic control the management of blood glucose levels through diet, medication, and lifestyle choices is the cornerstone of reducing infection risk.
Prevention is a daily habit, not a one‑time task. Follow these evidence‑based steps.
- Maintain optimal glycemic control. Aim for an A1C below 7% unless otherwise advised by your clinician. Lower glucose levels starve bacteria and improve white‑blood‑cell function.
- Daily skin inspection. Use a handheld mirror to check the back of your legs, between toes, and under any skin folds. Document any changes with photos.
- Keep skin clean and dry. Gentle, fragrance‑free cleansers are best. After washing, pat dry thoroughly, especially between toes.
- Foot care routine. Trim nails straight across, moisturize only on the tops of feet, and wear breathable socks and properly fitted shoes.
- Stay hydrated. Proper hydration helps maintain skin elasticity and supports the immune system.
- Vaccinations. The annual flu shot and pneumonia vaccine reduce the overall infection burden, indirectly protecting skin health.
Managing an Ongoing Infection
If an infection appears, act quickly.
- Contact a healthcare professional. Early prescription of antibiotics or antifungals prevents spread.
- Follow the full medication course. Even if symptoms improve, stopping early can cause recurrence or resistance.
- Elevate the affected limb. Elevation reduces swelling and improves circulation.
- Apply appropriate dressings. For open wounds, use non‑adhesive, moisture‑balancing dressings that keep the area clean.
- Monitor blood sugar closely. Infections raise stress hormones, which can spike glucose levels. Adjust insulin or oral meds as advised.
Complicated cases-such as deep tissue infection, rapidly spreading redness, or signs of sepsis-may require hospitalization for IV antibiotics and surgical debridement.
Frequently Asked Questions
Can I get a skin infection even if my diabetes is well‑controlled?
Yes. While good control reduces risk, factors like neuropathy or poor circulation can still allow infections to develop. Regular skin checks remain essential.
How long does it take for a diabetic foot ulcer to heal?
Healing time varies, but most uncomplicated ulcers close in 4‑8weeks. Delays often stem from infection, high blood sugar, or inadequate off‑loading.
Are over‑the‑counter antifungal creams enough for candidiasis?
For mild cases, a 2‑week course of clotrimazole or miconazole typically works. Persistent or extensive infections may need prescription oral medication.
What is the best way to keep my feet dry inside shoes?
Choose shoes with breathable materials, change socks at least once a day, and consider moisture‑wicking liners. Antifungal powders can also help.
Should I stop taking my diabetes medication if I develop an infection?
No. Infections often raise blood glucose, so you may need to adjust doses, but you should continue medication unless your doctor advises otherwise.
Staying proactive-controlling sugar, checking skin daily, and seeking prompt medical care-keeps skin infections from turning into serious complications.
Write a comment
Items marked with * are required.




17 Comments
M Black October 13, 2025 AT 12:59
Love the quick checklist-keep those socks fresh and feet dry 😊
Sidney Wachira October 14, 2025 AT 08:56
Whoa, this reads like the blockbuster trailer for a hidden epidemic-skin infections silently storming diabetic bodies! 🤯
Aditya Satria October 15, 2025 AT 05:46
Indeed, maintaining optimal glycemic control is the cornerstone; a modest reduction in A1C can dramatically lower infection susceptibility. Moreover, daily visual inspections serve as the frontline defense, catching minor breaches before they spiral. Pairing these habits with proper footwear and moisture management creates a synergistic barrier against bacterial and fungal intruders. Consistency is key-once a routine is entrenched, the immune system benefits from reduced inflammatory triggers. Keep the momentum going, and you’ll notice fewer skin complications over time.
Jocelyn Hansen October 16, 2025 AT 02:03
Fantastic summary!!! 🙌 Your daily foot‑check routine is the superhero cape every diabetic needs!!! Keep crushing it!!!
Joanne Myers October 16, 2025 AT 23:10
It is noteworthy that the correlation between elevated A1C levels and the incidence of cellulitis has been substantiated by multiple cohort studies.
rahul s October 17, 2025 AT 19:26
Honestly, most of these guidelines sound like textbook fluff-real warriors know the battlefield is in the shoes you wear, not some generic pamphlet.
Oscar Brown October 18, 2025 AT 17:06
When one contemplates the intricate interplay between hyperglycemia and cutaneous immunity, one must first acknowledge the profound impact of sustained elevated glucose on leukocyte chemotaxis, an essential process for pathogen clearance. Elevated plasma glucose impairs the oxidative burst within neutrophils, thereby diminishing their bactericidal capacity. Concurrently, the microvascular alterations characteristic of diabetes culminate in reduced perfusion, depriving the epidermal layers of vital oxygen and nutrients. This hypoxic milieu fosters an environment wherein opportunistic microbes, particularly Staphylococcus aureus and Candida species, flourish unabated. The neuropathic denervation of peripheral extremities further compounds the problem, as tactile feedback is blunted, allowing minor abrasions to escape detection. Consequently, the latency between insult and intervention is extended, often culminating in profound tissue involvement. Empirical evidence from longitudinal analyses indicates that each incremental rise of 1% in A1C correlates with a proportional increase in infection risk, a relationship that persists independent of confounding comorbidities. Moreover, the systemic inflammatory burden engendered by chronic infection can exacerbate insulin resistance, thereby establishing a deleterious feedback loop. Preventive stratagems, therefore, must be multifaceted, integrating stringent glycemic targets, meticulous foot hygiene, and patient education. The utility of daily foot inspections, when performed with appropriate illumination and magnification, cannot be overstated; such practices have been shown to reduce ulceration rates by a substantial margin. Additionally, the selection of breathable, moisture-wicking hosiery mitigates the proliferative advantage conferred upon fungal organisms in humid intertriginous zones. It is incumbent upon clinicians to individualize therapeutic regimens, considering both pharmacologic optimization and lifestyle modifications. Finally, timely medical intervention at the earliest sign of erythema or purulence remains paramount to averting systemic sequelae. Continued research into novel antimicrobial dressings promises further reductions in infection rates. In sum, the nexus of hyperglycemia, vascular compromise, and neuropathy creates a perfect storm for cutaneous infection, which can be mitigated through diligent, evidence‑based care.
Tommy Mains October 19, 2025 AT 15:20
Great points! In practice, I suggest using a simple checklist: check blood sugar, inspect feet, keep them dry, and change socks daily. Stick to it and you’ll lower your risk.
Alex Feseto October 20, 2025 AT 12:10
The epistemological ramifications of conflating glycemic indices with dermatological outcomes demand a rigorously controlled investigative paradigm.
vedant menghare October 21, 2025 AT 09:33
Indeed, the confluence of metabolic dysregulation and cutaneous vulnerability underscores the necessity for interdisciplinary collaboration between endocrinologists and dermatologists, thereby fostering comprehensive patient stewardship.
Kevin Cahuana October 22, 2025 AT 07:13
Honestly, it’s easy to overlook foot care when you’re juggling work, family, and meds, but a few minutes each night can save you from a painful infection later.
Danielle Ryan October 23, 2025 AT 04:03
Everyone pretends the pharma giants have your back, but have you considered that they might profit more from you developing infections and buying pricey ointments?!
Pramod Hingmang October 24, 2025 AT 00:53
Regular foot checks are non‑negotiable.
Benjamin Hamel October 24, 2025 AT 21:43
While the consensus champions relentless foot inspections, I maintain that an over‑obsession with microscopic scrutiny can induce anxiety and paradoxically impair healing, as stress hormones interfere with collagen synthesis and immune response.
Christian James Wood October 25, 2025 AT 18:33
That perspective ignores the empirical data demonstrating that patients who neglect routine examinations experience a statistically significant increase in ulceration and subsequent hospitalization, a reality that cannot be dismissed by mere anecdotal musings about stress.
Daisy Aguirre October 26, 2025 AT 14:23
Let’s keep the momentum-share your success stories so the community can learn how consistency transforms outcomes!
Jackie Berry October 27, 2025 AT 11:13
In the grand tapestry of diabetes management, skin health may seem a minor thread, yet it weaves together prevention, confidence, and overall quality of life; keep nurturing it, and the whole fabric benefits.