
Health November 25, 2025
Eosinophilic Esophagitis: Food Triggers and Steroid Slurries Explained
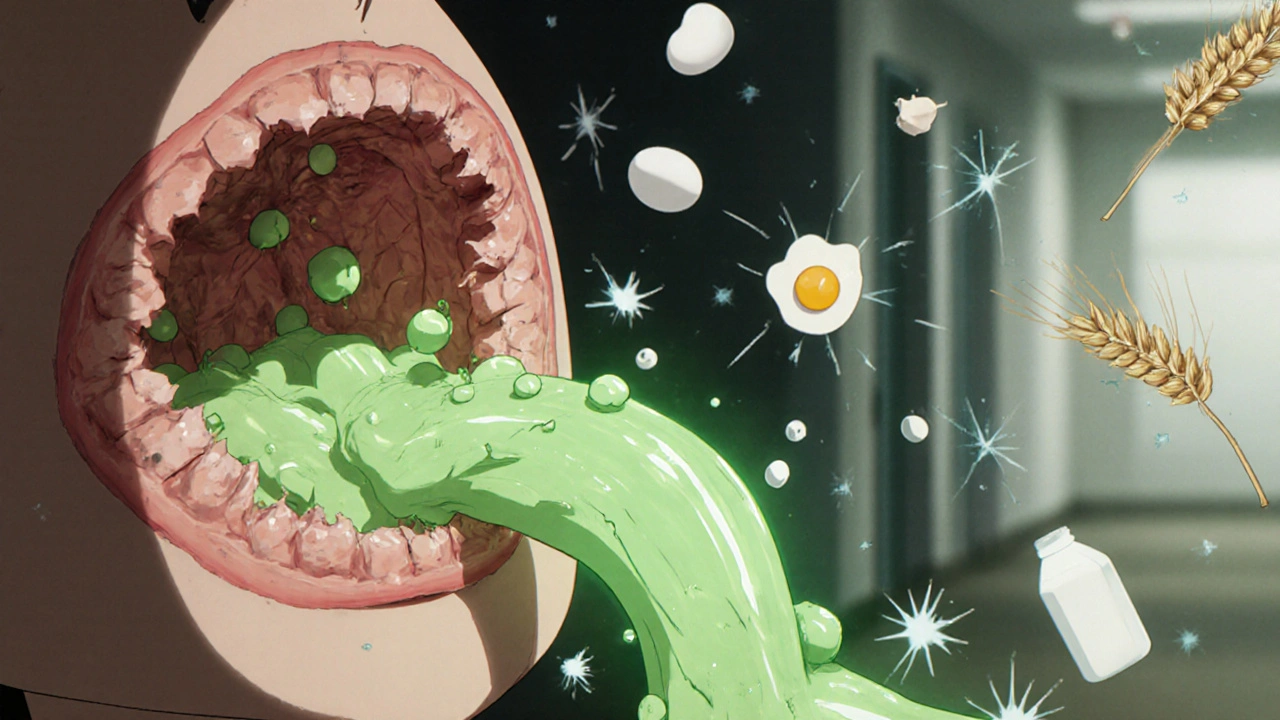
Eosinophilic esophagitis (EoE) isn’t just heartburn that won’t go away. It’s a chronic immune reaction where your body attacks food proteins, turning your esophagus into a swollen, inflamed tunnel that makes swallowing feel like choking on a piece of bread. Unlike acid reflux, EoE doesn’t respond to antacids. Instead, it demands a precise strategy: either remove the triggers from your diet or coat your esophagus with a special steroid slurry to calm the inflammation. Both approaches work - but they’re not easy.
What Exactly Is Happening in Your Esophagus?
EoE happens when eosinophils - white blood cells usually found in your gut or lungs - pile up in your esophagus like unwanted guests. These cells don’t belong there. When they do, they release chemicals that scar and narrow the tube, making it stiff and less flexible. A normal esophagus has fewer than 15 eosinophils per high-power field under the microscope. In EoE, that number jumps to 100 or more. This isn’t just irritation; it’s structural damage.
The condition was first clearly defined in the 1990s, but it’s only in the last decade that doctors began recognizing how common it is. Today, about 57 out of every 100,000 people in North America have EoE. It affects both kids and adults, but men are diagnosed more often. Symptoms vary: kids might refuse food or vomit, while adults often report food getting stuck, chest pain, or needing to drink water to get meals down. Many people live for years thinking they have GERD - until an endoscopy reveals the truth.
The Six Biggest Food Triggers (And One Surprising Shortcut)
Not all foods cause EoE. Research shows that six foods trigger the immune response in most patients: milk, eggs, wheat, soy, fish/shellfish, and nuts. These are the classic culprits, and eliminating all six at once - known as the six-food elimination diet (6FED) - clears symptoms in 75% to 80% of children and about 65% of adults.
But here’s the twist: you might not need to cut out all six. A major NIH-funded study in 2022 found that removing just milk - the one-food elimination diet (1FED) - worked just as well. About 64% of adults went into remission after ditching dairy alone. That’s nearly the same as the 65% who cleared symptoms after eliminating all six. Why? Because milk proteins - especially casein - are the most consistent trigger across populations. For many, cutting out cheese, yogurt, butter, and milk-based ingredients is enough.
That doesn’t mean other foods don’t matter. In Spain, soy and legumes are common triggers, affecting 35% of patients. In the U.S., that number is closer to 15%. This geographic variation means there’s no one-size-fits-all list. The only way to know your triggers is through elimination and reintroduction. You remove the suspected foods for 6-8 weeks, then add them back one at a time, watching for symptoms. Endoscopy confirms whether inflammation has truly faded.
Some people try allergy tests - skin prick or patch tests - but those are unreliable for EoE. Studies show they only catch 20-30% of true triggers. That’s why doctors don’t rely on them. The gold standard is still what you eat - and what you don’t.
Steroid Slurries: How a Breathing Inhaler Became a Swallowing Solution
If diet changes feel overwhelming, steroid slurries offer a medical alternative. These aren’t pills you swallow. They’re topical steroids - usually fluticasone (Flovent) or budesonide (Pulmicort) - mixed with a thick liquid like honey, applesauce, or water and then swallowed, not inhaled.
The trick? You don’t want the medication to go to your lungs. You want it to stick to your esophagus. So you take a small amount - say, 220 mcg of fluticasone mixed with 2-3 mL of water - hold it in your mouth for 30 seconds, then slowly swallow. Repeat twice daily for 8-12 weeks. This coats the inflamed tissue directly, reducing eosinophils without flooding your whole body with steroids.
Since January 2023, there’s been a new option: Jorveza. It’s budesonide specifically formulated as an oral suspension for EoE. Approved by the FDA, it’s dosed at 1.0 mg twice daily for 12 weeks. In clinical trials, 64% of patients reached histological remission - meaning their esophagus looked normal under the microscope - compared to just 2% on placebo.
Fluticasone slurry works in about 50-60% of cases. Budesonide slurry is slightly more effective, with 60-70% success rates. But neither is perfect. About 15% of users get oral thrush - a yeast infection in the mouth - because the steroid suppresses local immunity. That’s why you’re told to rinse your mouth after each dose. Some patients hate the taste. One Reddit user called it "swallowing chalk mixed with regret." Others prefer fluticasone because it’s easier to mix with water. Budesonide tastes like sweet, gritty medicine - but it works faster for many.
What Works Better: Diet or Drugs?
There’s no single winner. It depends on your life, your goals, and your tolerance for change.
- Dietary elimination has no side effects beyond hunger and social stress. It’s the only way to potentially cure EoE long-term - if you can stick to it. But 40% of people see symptoms return within six months of reintroducing foods. Nutritional gaps are also common. Cutting out dairy means you need to replace calcium and vitamin D. Eliminating wheat and soy can leave you short on fiber and protein.
- Steroid slurries bring faster relief - often within 2-4 weeks. They’re easier than tracking every ingredient in every meal. But they’re not a cure. If you stop taking them, inflammation comes back. And thrush, bad taste, and daily routines can make them hard to maintain.
For kids, dietary elimination still leads. Pediatricians prefer it because it avoids long-term steroid use. For adults, especially those with busy lives, steroid slurries are often the first choice. But many patients combine both: use steroids to get quick relief, then try a 1FED to find their trigger and reduce medication dependence.
And then there’s the elemental diet - a liquid formula made of broken-down amino acids, free of all proteins. It works in over 90% of cases. But it’s expensive ($1,200-$1,800 a month), tastes awful, and requires a feeding tube for some. It’s reserved for severe cases or when other treatments fail.

Real People, Real Struggles
Reddit’s r/EoE community has over 8,400 members sharing daily battles. One user, SwallowWithCare, eliminated dairy and went 14 months without needing a dilation procedure - something they’d needed every three months before. Another, FoodFight2023, spent eight weeks tracking every bite, only to find soy was their trigger. "I lost my social life," they wrote. "I didn’t go out to dinner once. Was it worth it? Maybe. But I almost quit."
On HealthUnlocked, a survey of 327 patients showed 68% improved with steroid slurries within four weeks. But 42% quit because of thrush. Meanwhile, 73% of those using budesonide slurry noticed relief within two weeks - faster than fluticasone. But 31% still preferred fluticasone because it was easier to prepare.
The emotional toll is real. EoE doesn’t just affect your throat - it affects your identity. Can you go to a birthday party? Eat at a restaurant? Travel? The constant vigilance wears people down. That’s why support groups and dietitians matter. The American Partnership for Eosinophilic Disorders (APFED) offers free consultations. The Cincinnati Center’s Food Pantry gives away hypoallergenic meals to qualifying patients.
What’s Next? The Future of EoE Treatment
The treatment landscape is changing fast. In May 2023, the FDA approved dupilumab (Dupixent), a biologic injection originally for eczema and asthma, for EoE. It targets the immune pathway driving eosinophil buildup. In trials, it helped 60% of adults achieve remission. Now, it’s being studied for kids too.
Researchers are also looking for biomarkers - blood or stool tests - that could predict your triggers without elimination diets. If that works, it could turn a years-long guessing game into a simple lab test. Component-resolved diagnostics are already being tested to identify specific proteins in milk or soy that trigger reactions, so you might only avoid the bad part of the food, not the whole thing.
Market projections show the EoE treatment market will hit $1.2 billion by 2030. But drugs like dupilumab will cost thousands per month. Insurance coverage is spotty. For now, diet and steroid slurries remain the most accessible options.
The key takeaway? You’re not alone. And you don’t have to choose between a perfect diet and perfect health. Start small. Try cutting out milk for six weeks. See if your swallowing improves. Talk to your doctor about budesonide slurry. Track your symptoms. Get an endoscopy to confirm. Then decide what’s sustainable - because living with EoE isn’t about perfection. It’s about finding a way to eat, swallow, and live without fear.
Can you outgrow eosinophilic esophagitis?
Some children do outgrow EoE, especially if their triggers are identified early and removed. But for adults, it’s usually a lifelong condition. Even if symptoms disappear after dietary changes or steroid treatment, stopping the regimen often leads to a return of inflammation. Regular monitoring is essential.
Is EoE the same as GERD?
No. GERD is caused by stomach acid backing up into the esophagus. EoE is an allergic immune reaction to food proteins. Both can cause trouble swallowing and chest pain, but GERD responds to acid blockers like omeprazole. EoE does not. Endoscopy with biopsy is the only way to tell them apart.
Do I need to avoid all dairy if milk is my trigger?
Yes - but only for the elimination phase. Milk includes cow’s milk, cheese, yogurt, butter, cream, whey, casein, and any ingredient derived from cow’s milk. Even trace amounts can trigger inflammation. After 6-8 weeks, you can reintroduce dairy one form at a time to see what, if anything, causes a reaction.
Can steroid slurries cause weight gain or bone loss?
Not usually. Because steroid slurries are swallowed and not inhaled, very little enters your bloodstream. Systemic side effects like weight gain, mood changes, or bone thinning are rare at the standard doses used for EoE. The main local side effect is oral thrush, which can be prevented by rinsing your mouth after each dose.
How often do I need an endoscopy for EoE?
You’ll need one at diagnosis to confirm EoE. After starting treatment - whether diet or steroids - you’ll need another endoscopy in 8-12 weeks to check for remission (fewer than 15 eosinophils per high-power field). After that, most doctors recommend a follow-up every 1-2 years if you’re stable, or sooner if symptoms return.
Write a comment
Items marked with * are required.



12 Comments
mohit passi November 25, 2025 AT 23:11
This post hit different 😌 I’ve been on budesonide slurry for 3 months and honestly? My throat feels like it’s been freed from a vice. No more choking on pizza. No more water chasers. Just... breathing. 🙏
Rachel Whip November 26, 2025 AT 20:27
Just a heads-up for anyone trying the 1FED: don’t forget hidden dairy in bread, deli meats, and even some vitamin D supplements. I thought I was clean until I checked the ingredient list on my granola. Total game-changer.
Joe bailey November 27, 2025 AT 10:23
I’ve been in this community for 2 years. Started with the 6FED, ended up just cutting milk. Now I eat out without panic. It’s not perfect but it’s mine. And yeah, I still rinse after my slurry. No thrush for me. 🎯
james thomas November 29, 2025 AT 05:18
Dupilumab costs $18k a year. You think they care if you can swallow? Nah. Big Pharma’s just selling hope wrapped in a syringe. Meanwhile, your grandma’s apple sauce + Flovent still works. Keep it simple.
JAY OKE November 30, 2025 AT 01:00
The part about soy being a bigger trigger in Spain? That makes sense. My cousin’s from Madrid and she’s allergic to everything with legumes. Meanwhile, here in Ohio? It’s all about cheese. Geography matters.
Ezequiel adrian December 1, 2025 AT 19:26
I tried the slurry. Tasted like regret and chalk. But I did it. 3 weeks in and I can finally eat a sandwich without feeling like I’m swallowing a sponge. Worth the grossness.
Micaela Yarman December 2, 2025 AT 19:10
I’ve been teaching EoE awareness in my university’s health program. Students are shocked that this isn’t just "bad acid." We need more public education. This isn’t a diet trend-it’s a medical reality. I’ve shared this post with my class.
Stephen Adeyanju December 3, 2025 AT 17:58
I hate that I have to carry a tiny bottle of budesonide everywhere I go. My coworkers think I’m on some kind of vape. I just want to eat a burger without a medical procedure
Asia Roveda December 4, 2025 AT 23:41
Why is it always the rich who get the new drugs? I can’t afford dupilumab. My insurance says "diet first" like I’m just being picky. Meanwhile, people with money get biologics and I get labeled "non-compliant."
Brittany Medley December 6, 2025 AT 02:35
Please remember: endoscopies are not optional. I skipped mine for a year because I "felt fine." Then I had a food impaction and spent 4 hours in the ER. Your esophagus doesn’t lie. If you’re not getting scoped, you’re gambling.
Cynthia Springer December 7, 2025 AT 05:03
Is there any data on whether long-term steroid slurry use affects dental health? I’ve noticed my teeth feel more sensitive since I started rinsing with water only. Should I be using a fluoride rinse?
Ali Miller December 8, 2025 AT 07:13
This is why America’s healthcare system is broken. You need a $2000 endoscopy to prove you’re not just being lazy. Meanwhile, in Germany, they just prescribe the slurry and move on. We’re stuck in the Stone Age.