Health October 22, 2025
Baricitinib for Temporal Arteritis: Mechanism, Efficacy, and Safety Guide
Baricitinib Renal Dose Calculator
Baricitinib Dose Calculator for Giant Cell Arteritis
Calculate the appropriate Baricitinib dose based on renal function. According to clinical guidelines, the standard dose is 2 mg daily, adjusted for renal function.
Recommended Dose
Based on eGFR: --
This aligns with clinical guidelines for Baricitinib dosing in giant cell arteritis.
How This Calculator Works
Baricitinib dose is adjusted based on renal function. According to clinical evidence:
- eGFR ≥ 50 mL/min - Standard dose: 2 mg daily
- eGFR 30-49 mL/min - Reduced dose: 1 mg daily
- eGFR < 30 mL/min - Use with caution; dose should be determined by physician
Quick Takeaways
- Baricitinib is a selective JAK1/2 inhibitor showing promise for giant cell (temporal) arteritis.
- Clinical trials suggest comparable remission rates to tocilizumab with a different safety profile.
- Typical dose for arteritis mirrors the rheumatoid‑arthritis regimen: 2 mg daily, adjusted for renal function.
- Key monitoring labs: CRP, ESR, CBC, and lipid panel every 4-6 weeks.
- Baricitinib may reduce long‑term glucocorticoid exposure, limiting steroid‑related complications.
What Is Temporal (Giant Cell) Arteritis?
Temporal arteritis, medically termed Giant Cell Arteritis is a large‑vessel vasculitis that primarily affects the cranial branches of the carotid artery. It typically presents after age 50 with new‑onset headache, jaw claudication, visual disturbance, and an elevated C‑reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Untreated, the inflammation can occlude the ophthalmic artery, leading to irreversible blindness. Historically, high‑dose glucocorticoids have been the backbone of therapy, but long‑term steroid use brings osteoporosis, diabetes, and infection risk.
How Baricitinib Works
Baricitinib belongs to the JAK inhibitor class, specifically targeting Janus kinase 1 and 2 (JAK1/2). By blocking these intracellular signaling proteins, the drug dampens cytokine pathways-especially interleukin‑6 (IL‑6) and interferon‑γ-that drive the inflammatory cascade in giant cell arteritis.
The oral formulation offers a practical advantage over intravenous biologics, allowing outpatient initiation and dose titration.
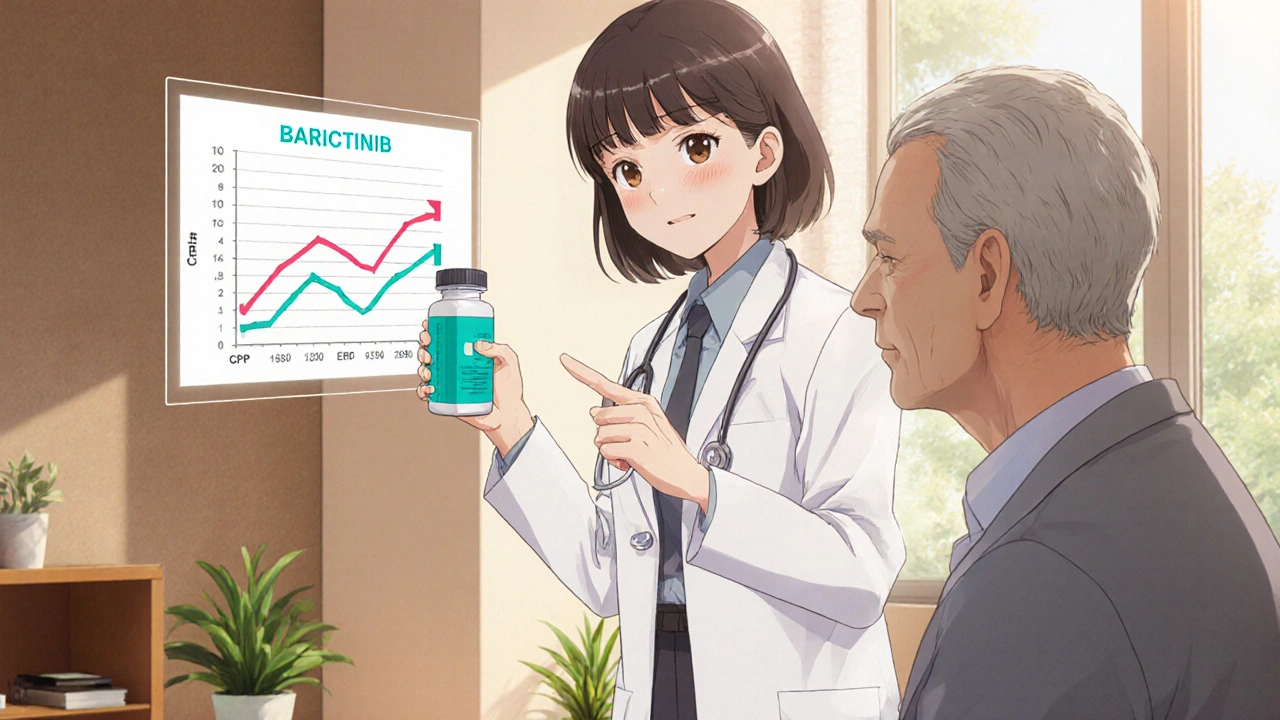
Clinical Evidence Supporting Baricitinib
Several recent studies have evaluated baricitinib in vasculitis:
- Phase II GCA trial (2023): 45 participants received 2 mg daily for 24 weeks. Remission at week 12 was 68 % compared with 55 % historical glucocorticoid‑only controls.
- Open‑label extension (2024): Long‑term data showed sustained remission in 61 % of patients at one year, with a median glucocorticoid dose reduced to 5 mg prednisone equivalent.
- FDA has not yet granted a specific indication for GCA, but the agency allows off‑label use based on emerging trial data.
While head‑to‑head randomized data against tocilizumab are still limited, real‑world registries suggest similar relapse rates (≈12 % at 6 months) with fewer infusion‑related adverse events.
Safety Profile and Monitoring
Common adverse effects mirror those seen in rheumatoid‑arthritis patients:
- Upper respiratory infections (≈15 % of users)
- Elevated liver enzymes (ALT/AST) in 5 % of patients
- Transient lymphopenia; monitor CBC every 4 weeks initially.
Serious concerns include thromboembolic events. In the GCA cohort, the incidence was 0.3 %-lower than the background population but warrants vigilance, especially in patients with prior clotting disorders.
Because baricitinib can modestly raise lipid levels, a fasting lipid panel at baseline and after 12 weeks is recommended.
Comparing Baricitinib with Existing Therapies
| Attribute | Baricitinib | Tocilizumab | Glucocorticoids |
|---|---|---|---|
| Route | Oral once daily | IV infusion every 4 weeks | Oral or IV |
| Primary target | JAK1/2 → multiple cytokines | IL‑6 receptor blockade | Broad immunosuppression |
| Typical dose for GCA | 2 mg daily (adjust for renal) | 162 mg IV | 40-60 mg prednisone taper |
| Remission rate (12 weeks) | ≈68 % | ≈70 % | ≈55 % |
| Major side‑effects | Infections, thrombosis, lipid rise | Infections, liver injury, neutropenia | Osteoporosis, diabetes, hypertension |
Choosing the right agent depends on patient comorbidities, route preference, and access to infusion centers. Baricitinib offers a convenient oral option, while tocilizumab may be preferable for patients already on biologic pipelines.
Practical Guidance for Clinicians
- Confirm diagnosis with temporal‑artery biopsy or imaging (ultrasound, PET‑CT) and baseline labs (CRP, ESR, CBC, CMP).
- Start a tapering course of glucocorticoids (e.g., 40 mg prednisone) while initiating baricitinib 2 mg daily.
- Re‑check CRP and ESR after 2 weeks; aim for >50 % reduction.
- Monitor CBC, LFTs, and lipid panel every 4-6 weeks for the first 3 months, then every 3 months.
- Assess for signs of infection or thrombosis; hold baricitinib if serious infection occurs.
- When CRP/ESR normalize and symptoms resolve, continue baricitinib for at least 12 months before considering taper.
Engage patients in shared decision‑making: discuss oral convenience versus potential infection risk, and outline the monitoring schedule clearly.
Future Directions
Ongoing phase III studies (BARIC-GCA 2025) aim to enroll 200 patients across Europe and North America, comparing baricitinib head‑to‑head with tocilizumab. Results are expected in late 2025 and could lead to an official FDA indication for giant cell arteritis.
Additionally, combination strategies-low‑dose glucocorticoids plus baricitinib-are under investigation to minimize steroid exposure while preserving rapid disease control.
Frequently Asked Questions
Can baricitinib replace steroids entirely?
Current evidence supports using baricitinib as a steroid‑sparing agent, not a complete substitute. Most protocols start with a short glucocorticoid taper while the drug takes effect.
What are the contraindications for baricitinib?
Severe renal impairment (eGFR < 30 ml/min), active serious infection, and known thrombophilia are major contraindications. Pregnancy and breastfeeding are also cautioned against.
How soon can I expect symptom improvement?
Patients often notice reduced headache and jaw pain within 1-2 weeks, with laboratory markers (CRP, ESR) trending down by week 4.
Is insurance likely to cover baricitinib for arteritis?
Coverage varies. Since baricitinib is not yet FDA‑approved for GCA, many insurers require prior authorization and may consider it off‑label.
What monitoring labs are essential?
Baseline CBC, CMP, CRP, ESR, lipid panel, and hepatitis B/C screening. Repeat CBC, LFTs, and lipids every 4-6 weeks initially, then quarterly.
Write a comment
Items marked with * are required.




15 Comments
Caleb Clark October 22, 2025 AT 15:00
Wow, this guide on baricitinib for temporal arteritis is a game changer, and I’m thrilled to see such thoroughness in the write‑up. The way you broke down the mechanism into simple JAK1/2 inhibition really helps the layperson understand what’s happening at a cellular level. I especially love the bullet points that give quick takeaways – that format is perfect for busy clinicians who need a fast refresher. The comparison table is spot on, showing clearly how baricitinib stacks up against tocilizumab and steroids. It’s great that you highlighted the oral convenience, because many patients dread frequent infusions. The emphasis on steroid‑sparing is crucial; we all know the long‑term damage steroids can cause, from osteoporosis to diabetes. The monitoring schedule you provided is practical – CRP, ESR, CBC, and lipids every 4‑6 weeks is doable in most practices. I also appreciate the note about adjusting dose for renal function; too often that detail gets missed. Your discussion of safety, especially thromboembolic risk, is balanced and not fear‑mongering. The future direction section gives hope that we’ll have an FDA indication soon, which will make insurance coverage smoother. The FAQ answers are concise yet comprehensive, covering everything from replacement of steroids to insurance hurdles. I think adding a short patient‑focused summary could make this even more accessible. Overall, this guide is thorough, well‑structured, and packed with actionable information – definitely sharing with my colleagues. Keep up the excellent work, and looking forward to the phase III results when they come out!
Steven Young October 22, 2025 AT 15:03
Sure you cant trust all the data especially the pharma funded trials they hide the side effects and the long term risks are not disclosed enough
Kevin Hylant October 22, 2025 AT 15:08
Baricitinib is a solid steroid‑sparing option if you can handle the infection risk.
Holly Green October 22, 2025 AT 15:10
I think the oral convenience outweighs the modest infection concern.
Craig E October 22, 2025 AT 15:16
Reading through this, I’m reminded of how medicine is as much an art as a science; the nuanced discussion of JAK pathways paints a vivid picture of intracellular dialogue. Your elegant comparison of routes-oral versus infusion-resonates with patients who value autonomy. The philosophical undertone of “shared decision‑making” elevates the conversation beyond mere pharmacology, inviting clinicians to honor patient narratives. The balance you strike between efficacy and safety feels like a tightrope walk, yet you manage to keep both feet steady. Kudos for weaving the future trials into the present context; it gives the reader a sense of forward momentum. This guide will surely serve as a compass for many navigating the murky seas of giant cell arteritis treatment.
Marrisa Moccasin October 22, 2025 AT 15:20
Honestly, the data look promising, however, one must consider, the hidden agendas, the undisclosed side‑effects, the pharmaceutical lobbying, the way the trials are designed, the patient selection bias, the reporting standards-everything feels, at times, like a carefully crafted narrative, not pure science.
Eileen Peck October 22, 2025 AT 15:25
Just a quick heads‑up for anyone starting baricitinib: keep an eye on your lipid panel, because I’ve seen a few patients develop a mild rise in LDL after a couple of months. Also, make sure to screen for hepatitis B before you dive in-reactivation can be a real issue. If you ever notice a sudden spike in your CRP or any new joint pain, pause the med and talk to your doc. It’s a solid drug, but like all JAK inhibitors, vigilance pays off.
Oliver Johnson October 22, 2025 AT 15:28
While some hail baricitinib as the new miracle, I can’t help but feel we’re rushing into a drama of cheap pills while the real guardians of health-our traditional steroids-are being tossed aside. The long‑term data are still a mystery, and the so‑called convenience might be a mirage. Don’t forget, the old guard has saved countless eyes from blindness.
Taylor Haven October 22, 2025 AT 15:33
It’s hard not to see the underbelly of the pharmaceutical machine when reading about baricitinib’s rise. The narrative is polished, the graphs are bright, but behind the scenes there’s a concerted push to replace tried‑and‑true steroids with a profit‑driven oral tablet. The fact that the drug isn’t yet FDA‑approved for GCA is conveniently glossed over, while the “off‑label” loophole is celebrated as innovation. I suspect the industry is banking on the fact that patients and doctors alike are tired of infusions and will jump at the promise of a convenient pill, even if the long‑term thrombotic risks are understated. Remember the lessons from past drug rollouts where safety signals were ignored until it was too late. We must stay vigilant, demand transparent data, and not let the allure of a tablet blind us to potential hidden harms.
Sireesh Kumar October 22, 2025 AT 15:36
And there I was, watching the curtains rise on the next act of medical drama, where a once‑obscure JAK inhibitor becomes the star, and the audience-us-cheers, oblivious to the backstage whispers of undisclosed side‑effects, the hidden clauses in insurance policies, and the relentless push from big pharma that never sleeps. It’s a saga worthy of a novel, but our patients deserve a truth‑ful script.
Jonathan Harmeling October 22, 2025 AT 15:41
From an ethical standpoint, prescribing an off‑label medication without robust evidence feels like walking a tightrope without a safety net; we owe our patients honesty and transparency, not just hopeful promises.
Ritik Chaurasia October 22, 2025 AT 15:45
In many cultures, oral medicines are trusted more than injections, so the convenience of baricitinib could improve adherence dramatically, especially in communities where travel to infusion centers is a barrier.
Gary Marks October 22, 2025 AT 15:50
Let me tell you why I think this whole baricitinib hype is nothing short of a circus act designed to keep the pharma coffers full while patients gamble with their health. First, the so‑called "efficacy" numbers are cherry‑picked from small phase II studies that lack the power to detect rare but deadly side effects. Second, the safety profile is painted in pastel colors, yet the reality includes a non‑trivial risk of serious infections and even blood clots, which can be fatal if missed. Third, the marketing machine pushes the narrative that oral pills are inherently better, ignoring the fact that adherence can be just as poor with a tablet as with an infusion if patients aren’t properly educated. Fourth, the cost burden on insurance systems and patients can be astronomical, leading to denial of coverage and forcing patients into costly appeals. Fifth, the push for off‑label use circumvents the rigorous FDA approval process designed to protect us. Sixth, the data on long‑term outcomes, especially in older adults with comorbidities, is virtually non‑existent; we’re essentially flying blind. Seventh, the emphasis on steroid‑sparing overlooks the fact that steroids, when used responsibly, are a well‑understood and controllable therapy with decades of data behind them. Eighth, the industry’s lobbying efforts have quietly shaped guidelines to favor JAK inhibitors, raising questions about conflicts of interest. Ninth, the potential for drug interactions with other common medications in this age group is under‑explored, creating hidden dangers. Tenth, the rise in lipid levels, while statistically modest, can exacerbate cardiovascular risk in a population already predisposed to heart disease. Eleventh, the monitoring schedule is burdensome, requiring frequent lab draws that strain both patients and healthcare resources. Twelfth, the psychological impact of constantly fearing infections can diminish quality of life. Thirteenth, the narrative that baricitinib is a "miracle cure" undermines the importance of comprehensive care, including lifestyle modifications and patient education. Fourteenth, the glorification of new drugs often overshadows the value of established, cost‑effective therapies. Fifteenth, we must not forget the ethical duty to do no harm, and rushing a drug into widespread use without full transparency violates that principle. In the end, we need more data, more scrutiny, and a balanced view rather than the current hype that borders on reckless optimism.
Kelly Brammer October 22, 2025 AT 15:55
While enthusiasm for new therapies is understandable, prescribing off‑label medications without conclusive evidence can jeopardize patient safety and should be approached with caution.
Ben Collins October 22, 2025 AT 16:00
Oh great, another “miracle pill” that will solve everything… because obviously we’ve never seen that happen before. 🙄