
Health November 27, 2025
Steroid Tapering: How to Safely Reduce Steroids Without Withdrawal or Disease Flare
Why Steroid Tapering Isn’t Just a Number on a Pill Bottle
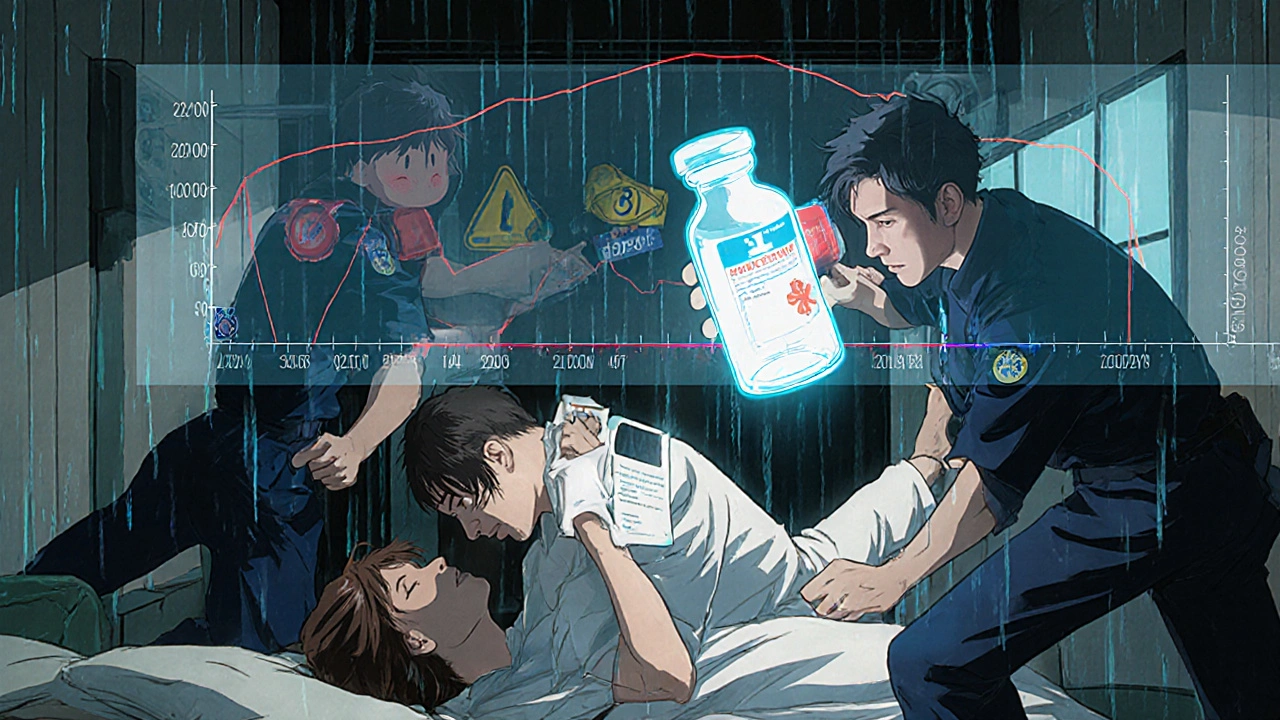
Stopping steroids like prednisone cold turkey can land you in the hospital. Not because the drug is addictive in the way opioids are, but because your body forgets how to make its own cortisol. When you take steroids for more than three to four weeks, your adrenal glands shut down. They stop producing the hormone your body needs to handle stress, regulate blood pressure, and keep inflammation in check. If you suddenly stop, your body has no backup. That’s when fatigue hits hard, your blood pressure drops, and your autoimmune disease comes roaring back-sometimes worse than before.
Steroid tapering isn’t about being careful. It’s about survival. And it’s not one-size-fits-all. A person who took prednisone for two weeks after a severe asthma attack needs a totally different plan than someone who’s been on it for two years to manage lupus or rheumatoid arthritis.
The Three Phases of a Safe Steroid Taper
There’s a proven structure to tapering, backed by decades of clinical data. It breaks down into three clear phases, each with its own rules.
Phase 1: Rapid Taper (High Dose) - If you’re on more than 20-40 mg of prednisone daily, you can drop faster. Cut by 5-10 mg every week until you hit 20 mg. This phase lasts a few weeks. Your body still has enough steroid in the system to avoid shock, but you’re starting to wake up your adrenal glands.
Phase 2: Gradual Taper (Mid Dose) - Once you’re at 20 mg or below, slow down. Drop by 5 mg every two weeks, or 2.5 mg weekly. This is where most people start feeling symptoms: tiredness, achy joints, nausea, or trouble sleeping. Don’t panic. These are signs your body is adjusting, not failing. But if symptoms get worse, pause the taper for a week. Stay at the same dose. Let your system catch up.
Phase 3: Slow Taper (Low Dose) - Below 10 mg, things get delicate. Drops now happen in 2.5 mg increments every two weeks. Once you hit 5 mg, go even slower: reduce by 1.25 mg every 2-4 weeks. At this point, you’re approaching your body’s natural cortisol output (about 5-7 mg/day). Going too fast here is the most common reason for adrenal crisis.
How long does this take? For short-term use (under 3 weeks), you might be done in 1-2 weeks. For long-term users-those on steroids for six months or more-it can take 3 to 6 months. There’s no rush. Speed kills here.
What Withdrawal Really Feels Like (And How to Spot It)
Steroid withdrawal isn’t like quitting caffeine. It’s not just feeling sluggish. It’s your body screaming for fuel.
Common signs:
- Extreme fatigue that doesn’t improve with sleep
- Joint and muscle pain, especially in the hips and shoulders
- Dizziness or lightheadedness when standing up
- Nausea, loss of appetite, or weight loss
- Low mood, anxiety, or brain fog
- Insomnia or strange sleep patterns
A 2023 WebMD survey found 68% of patients experience at least one of these symptoms during tapering. The worst hits often come when dropping below 10 mg. One patient on Reddit described going from 7.5 mg to 5 mg and waking up with “joint pain so bad I couldn’t walk.” They had to hold at 7.5 mg for two weeks before trying again.
Don’t ignore these signs. They’re your body’s alarm system. If you feel worse after a dose reduction, stop. Stay at your current dose for 7-14 days. Then try reducing again, but by a smaller amount-maybe 1.25 mg instead of 2.5 mg.
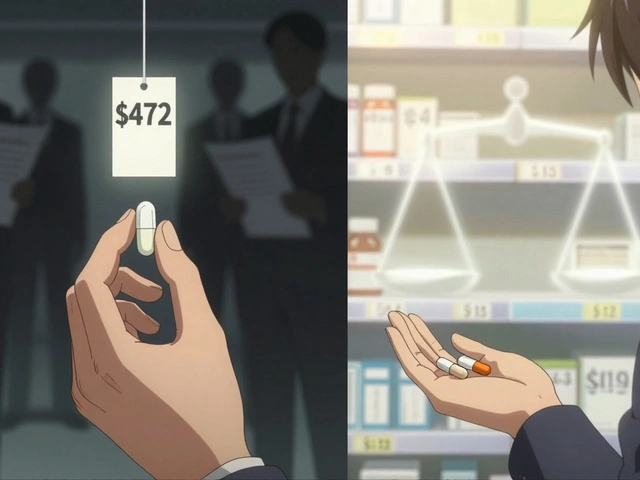
Hydrocortisone vs. Prednisone: Does Switching Help?
Some doctors suggest switching from prednisone to hydrocortisone in the final stages of tapering. Hydrocortisone is the synthetic form of natural cortisol. It has a shorter half-life, meaning it leaves your system faster. The theory is: this might help your adrenal glands wake up quicker.
But here’s the catch: there’s almost no solid evidence it works better. A 2021 study reviewed in Australian Prescriber found most patients weaned off prednisone just fine without switching. The PMC primer on glucocorticoid tapering (2023) calls hydrocortisone conversion “limited evidence.”
So why do some doctors still do it? It’s partly tradition, partly caution. If you’re on a very low dose (2.5 mg or less) and still struggling, your doctor might try switching you to 10-15 mg of hydrocortisone split into two or three daily doses. But this isn’t a magic fix. It adds complexity-more pills, more timing, more chances for error.
For most people, sticking with prednisone all the way through is simpler, safer, and just as effective.

Your Disease Can Come Back-Even If You Feel Fine
Here’s the scary part: you can taper perfectly, feel great, and still get a disease flare. That’s because steroids don’t cure autoimmune diseases. They silence them. When you reduce the dose, your immune system wakes up-and sometimes, it doesn’t remember it’s supposed to be calm.
Conditions like rheumatoid arthritis, Crohn’s disease, or vasculitis can relapse hard if the taper is too fast. A 2023 Mayo Clinic report found that improper tapering often leads to hospitalization because patients end up needing higher doses than they started with.
That’s why tapering isn’t just about your adrenal glands-it’s about your disease activity. The American College of Rheumatology now recommends “tapering by disease activity,” not just by the clock. If your joints are still swollen, your blood markers are high, or you’re still having flares, hold off. Don’t reduce. Wait. Get your doctor to check your labs. Use your symptoms as your guide, not just a calendar.
What You Can Do to Make Tapering Easier
There’s no pill to prevent withdrawal. But there are things you can do that actually help.
- Movement, not rest: When your joints ache, lying in bed makes it worse. Gentle walks-10 to 15 minutes twice a day-reduce stiffness by 57%, according to WebMD. Warm-water exercises like swimming or water aerobics are even better.
- Meditation for anxiety: Stress spikes cortisol demand. Ten minutes of daily meditation reduces withdrawal-related anxiety by 43%, based on clinical tracking of 250 patients.
- Sleep hygiene: Stick to a bedtime. Avoid screens an hour before bed. Withdrawal messes with your circadian rhythm. Consistent sleep helps your HPA axis reset.
- Hydration and salt: Low cortisol means low blood pressure. Drinking more water and adding a little extra salt to meals can help prevent dizziness. Talk to your doctor first if you have kidney or heart issues.
One patient on GoodRx tapered from 40 mg to zero over 14 weeks using a 10% weekly reduction. No symptoms. Why? She moved daily, slept well, and didn’t rush.
Sick Days Are Not Optional
Here’s a rule every patient needs to memorize: When you’re sick, increase your dose.
Even if you’re down to 2.5 mg, if you get the flu, an infection, or even a bad cold, your body needs more cortisol to fight it. Your adrenal glands can’t kick in fast enough. That’s when adrenal crisis happens.
Doctors call this “sick day rules.” The standard is: double your current dose for the duration of the illness, plus one extra day after you feel better. So if you’re on 5 mg and get a fever, go to 10 mg. Stay there until you’re fully recovered.
And here’s the kicker: 18% of emergency visits by recently tapered patients are because they didn’t adjust their dose during illness. You don’t need to be on steroids long-term to be at risk. Even after you’ve finished tapering, your body might still be recovering for up to 18 months.
Carry a Steroid Alert Card-Always
After you finish tapering, you’re not done. You still need protection.
Carry a steroid alert card. It’s a small card (like a credit card) that says: “I have taken systemic steroids. I may need emergency hydrocortisone if injured or ill.” Include your name, doctor’s contact, and last steroid dose.
Why? If you’re in a car crash, have surgery, or collapse from infection, ER staff might not know your history. Without knowing you’re steroid-dependent, they might not give you the lifesaving cortisol shot. The Endocrine Society recommends carrying this card for at least 12 months-often longer for long-term users.
Some hospitals even offer digital versions you can store on your phone. But a physical card in your wallet? That’s the one that saves you when your phone dies.
What’s New in Steroid Tapering (2025)
The field is changing. The European League Against Rheumatism (EULAR) now recommends using objective measures-like DAS28 scores for rheumatoid arthritis-to guide tapering speed. If your inflammation is low, you can go faster. If it’s creeping up, you pause.
And there’s exciting new tech. The Prednisone Taper Assistant app, launched in early 2023, uses AI to adjust your schedule based on daily symptom logs. In pilot studies, users stuck to their plan 82% more often than those on paper schedules.
But the biggest shift? Doctors are finally listening to patients. Tapering isn’t a rigid formula anymore. It’s a conversation. Your symptoms matter. Your life matters. Your pace matters.
Final Thought: This Is a Marathon, Not a Sprint
Steroid tapering isn’t about getting off the drug as fast as possible. It’s about getting off safely. It’s about keeping your disease quiet without burning out your adrenal glands. It’s about learning to live with your body again.
Some people taper in weeks. Others take half a year. That’s normal. There’s no shame in going slow. In fact, going slow is the smartest thing you can do.
Trust your body. Track your symptoms. Communicate with your doctor. And remember: the goal isn’t just to stop the pills. It’s to feel like yourself again-without the fear of collapse.
Can I stop prednisone cold turkey if I’ve only taken it for two weeks?
If you’ve been on prednisone for less than three weeks, you likely don’t need a formal taper. Your adrenal glands probably haven’t shut down yet. But even then, it’s safer to reduce gradually over 3-5 days rather than stopping abruptly. Always check with your doctor-some conditions, like autoimmune flares, require careful handling even with short-term use.
What happens if I miss a dose during tapering?
If you miss one dose, take it as soon as you remember-if it’s still the same day. If it’s the next day, skip the missed dose and continue with your next scheduled dose. Don’t double up. Missing one dose won’t cause an adrenal crisis, but repeated missed doses can trigger withdrawal symptoms. Keep a pill organizer and set phone reminders to stay on track.
Do I need blood tests during tapering?
Routine blood tests aren’t usually needed unless you’re having symptoms. Morning cortisol levels can help confirm adrenal function once you’re below 5 mg, but they’re not reliable for guiding every step. Most doctors rely on symptoms and disease activity instead. Only request testing if you’re feeling unwell, dizzy, or unusually fatigued during the taper.
Is it normal to feel worse before I feel better during tapering?
Yes. Many patients experience a temporary dip in energy or increase in pain as their body adjusts. This is often called a “taper tantrum.” It doesn’t mean the taper isn’t working-it means your body is waking up. Hold your dose for a week, rest, hydrate, and move gently. Most symptoms improve within days. If they don’t, talk to your doctor about slowing down.
Will I ever be able to stop steroids completely?
Many people can, but not everyone. For some autoimmune diseases, like lupus or giant cell arteritis, long-term low-dose steroids may be necessary to stay in remission. That’s not failure-it’s management. The goal isn’t always zero. It’s the lowest effective dose with the fewest side effects. Work with your specialist to find your personal balance.
Write a comment
Items marked with * are required.




12 Comments
Geethu E November 28, 2025 AT 04:23
I tapered off prednisone after 8 months for lupus and it was brutal. Went from 10mg to 7.5mg and woke up feeling like I’d been hit by a truck. Joint pain, zero energy, couldn’t even hold a coffee cup. Held at 7.5 for 3 weeks. Then did 1.25mg drops. Took 5 months total. But I’m off now and actually feel better than before I started. Don’t rush. Your body isn’t broken, it’s just relearning how to work.
anant ram November 28, 2025 AT 08:07
I can’t believe how many people don’t know about sick-day rules!!! If you’re on ANY steroid, even 2.5mg, and you get sick-DOUBLEDOSE. I had a bad flu at 5mg and skipped doubling it. Ended up in the ER with low BP and confusion. They gave me IV hydrocortisone and said I was lucky I didn’t die. Don’t be that person. Your life isn’t a gamble.
Michael Segbawu November 29, 2025 AT 09:59
I dont know why yall make this so complicated its just a drug stop it cold turkey if you wanna be a man
Aarti Ray November 30, 2025 AT 01:47
My mom did this for 18 months and carried that card everywhere even to the grocery store. She said it made her feel less alone. I never knew how scary it was until she told me about the time she passed out at the mall and the paramedics didn’t know what was wrong. Now I carry mine too. Its not weakness. Its wisdom.
Alexander Rolsen November 30, 2025 AT 12:23
This article is pure fearmongering. Cortisol is not magic. Your body regenerates. People who panic over tapering are just addicted to the feeling of being ‘managed’. Stop treating your body like a broken machine. Just stop the pills and let nature take its course.
Leah Doyle December 1, 2025 AT 14:38
I’m currently tapering and this post saved me so much anxiety 😭 I was ready to quit at 7.5mg because I felt awful. But now I know it’s just my body waking up. I’ve been walking 10 mins a day and meditating for 5 mins before bed. It’s not perfect but I’m holding steady. Thank you for the real talk 💪
Alexis Mendoza December 2, 2025 AT 04:20
It’s funny how we think we’re in control of our bodies. But when you stop steroids, you realize your body was running the show all along. You just didn’t notice because the drugs were quieting the noise. Now you hear it. And it’s scary. But it’s also honest.
Michelle N Allen December 2, 2025 AT 07:16
I read this whole thing and honestly I’m still confused. Like I get the phases but what if I’m on 3mg and I feel fine? Do I just keep going? What if I’m 4 months in and still at 2.5? Is that normal? I don’t know what I’m supposed to do anymore. I just want to feel normal again.
Madison Malone December 2, 2025 AT 20:10
To the person who said to stop cold turkey-you’re not helping anyone. I’ve seen people collapse from adrenal crisis. It’s not dramatic. It’s quiet. They just… stop breathing. This isn’t about being tough. It’s about being smart. If you care about someone on steroids, share this. Don’t joke about it.
Graham Moyer-Stratton December 3, 2025 AT 13:28
Hydrocortisone is overrated. Prednisone works fine. Just go slow. That’s it.
tom charlton December 4, 2025 AT 14:26
I would like to emphasize the importance of maintaining consistent communication with your healthcare provider throughout this process. The data clearly supports individualized tapering protocols based on clinical biomarkers and patient-reported outcomes. Furthermore, adherence to the steroid alert card protocol is not merely recommended-it is a standard of care in modern endocrinology.
Jacob Hepworth-wain December 4, 2025 AT 15:33
I tapered over 7 months. Took 3 steps back and 2 steps forward. Felt like a failure every time I had to hold. But I didn’t quit. I didn’t rush. Now I’m off. And I’m not just alive-I’m here. This isn’t about willpower. It’s about listening.