Health November 17, 2025
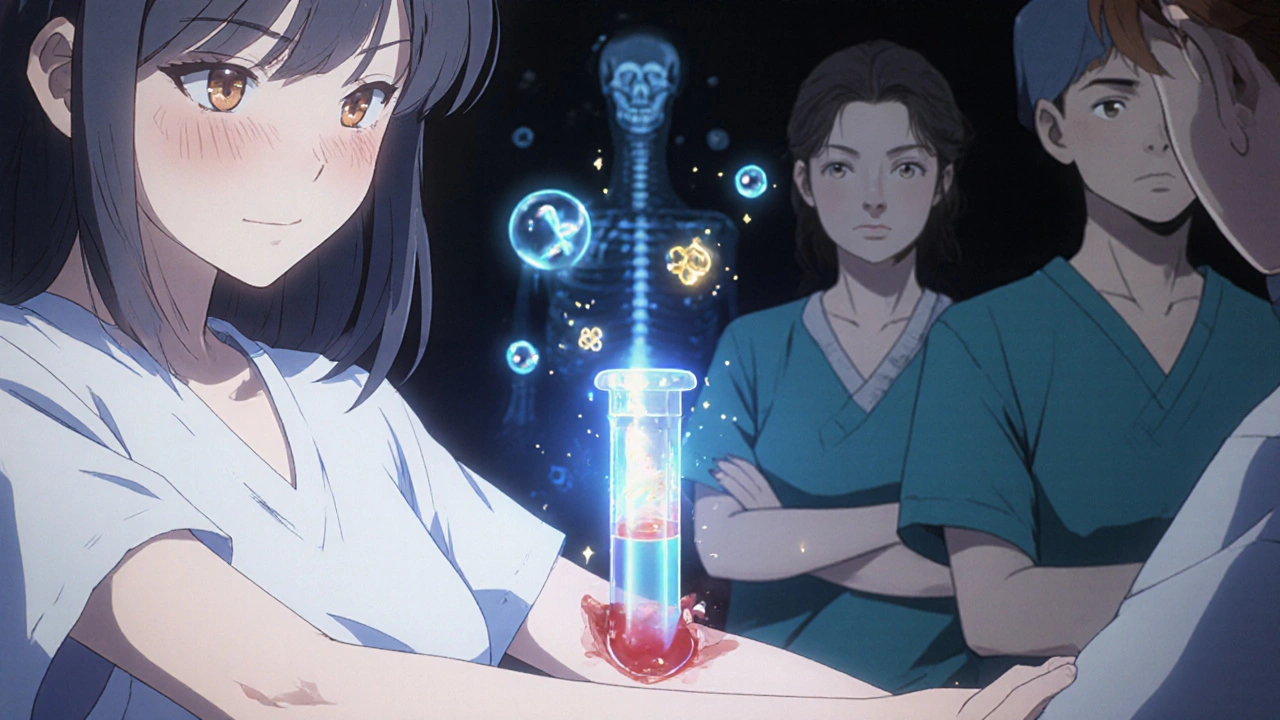
Bone Turnover Markers: How They Help Monitor Osteoporosis Treatment
When you start treatment for osteoporosis, you don’t have to wait two years to know if it’s working. That’s the big shift happening in bone health right now. Instead of relying only on slow, expensive DEXA scans that show changes after 12 to 24 months, doctors are turning to something faster, simpler, and more immediate: bone turnover markers. These are tiny protein fragments and enzymes in your blood or urine that tell you exactly how fast your bones are breaking down and rebuilding. And for people on osteoporosis meds, that speed matters.
What Are Bone Turnover Markers?
Bone is always changing. Old bone breaks down, new bone forms. This process is called remodeling. In osteoporosis, the balance tips-too much breakdown, not enough rebuilding. Bone turnover markers (BTMs) are the byproducts of this process. When bone cells break down old bone, they release fragments like collagen pieces into the bloodstream. When new bone is made, cells produce proteins that show up in the blood too. There are two main types:- Resorption markers: Show how fast bone is being broken down. The most reliable is β-CTX-I (beta-C-terminal telopeptide of type I collagen). It’s measured in plasma and drops when you take drugs like bisphosphonates or denosumab.
- Formation markers: Show how fast new bone is being made. The gold standard here is PINP (procollagen type I N-terminal propeptide). It rises when you take anabolic drugs like teriparatide or romosozumab.
These aren’t just lab curiosities. They’re validated, standardized, and recommended by the International Osteoporosis Foundation and the European Calcified Tissue Society as the go-to markers for tracking treatment.
Why They’re Better Than DEXA Scans for Early Feedback
DEXA scans measure bone mineral density. They’re the gold standard for diagnosis. But they’re slow. Even if your medication is working perfectly, it takes 1 to 2 years before the scan shows a clear improvement. By then, you might have already missed your chance to adjust your treatment. BTMs change much faster. Within 3 to 6 weeks of starting a new drug, you’ll see measurable shifts. A drop in β-CTX-I? That means your bone breakdown is slowing. A jump in PINP? Your body is building new bone. This gives your doctor real-time feedback-no waiting. Studies like the TRIO trial show this isn’t theoretical. Patients who had a 30% or greater drop in β-CTX-I after 3 months of bisphosphonate therapy had a 1.6% lower fracture risk after just 22 weeks. That’s a direct link between early marker changes and real-world outcomes.How Doctors Use Them in Practice
The routine isn’t complicated, but it’s precise:- Before treatment: Get a baseline test for PINP and β-CTX-I. This sets your personal starting point.
- At 3 months: Repeat the test. For antiresorptive drugs (like alendronate or denosumab), you want to see at least a 30% drop in β-CTX-I or a 35% drop in PINP. For anabolic drugs (like teriparatide), PINP should rise by 70-100%.
- At 12-24 months: Get a DEXA scan to confirm structural changes. BTMs tell you if the drug is working. DEXA tells you if your bones are getting stronger.
This two-step approach saves time, money, and risk. If your BTMs don’t move after 3 months, you’re probably not responding-or not taking your meds. That’s not failure. It’s information. Your doctor can switch drugs, adjust dosing, or check for adherence before you suffer a fracture.
What You Need to Know Before the Test
BTMs are sensitive. Small mistakes in how the test is done can throw off results. If you don’t follow the rules, your numbers could look wrong-even if your treatment is fine.- For β-CTX-I: You must fast overnight. Eat or drink anything (even coffee) before the test, and your levels can spike by 20-30%. Collect the sample between 8 and 10 a.m. CTX levels vary by up to 40% during the day. Morning is the only reliable time.
- For PINP: Less affected by meals, but still best collected in the morning. Diurnal variation is around 10-15%-still enough to matter.
- Don’t take your meds on the day of the test unless your doctor says otherwise. Some drugs interfere with results.
- Don’t get tested after a fracture or surgery. Healing bones cause wild spikes in turnover markers.
These aren’t just suggestions. They’re requirements. If your lab doesn’t know this, ask them to follow the IFCC guidelines. Not all labs do.
Who Should Get Tested?
Not everyone needs BTMs. But they’re especially useful for:- People starting a new osteoporosis drug for the first time
- Those who aren’t responding to treatment after 6 months
- Patients with poor adherence-maybe they forget pills or skip injections
- People with kidney disease (CKD), where traditional markers like β-CTX-I can be misleading
- Anyone on anabolic therapy, where PINP rise confirms the drug is activating bone-building cells
For most healthy postmenopausal women on standard therapy, a baseline test and one follow-up at 3 months is enough. After that, DEXA scans take over.

Limitations and Pitfalls
BTMs aren’t perfect. They measure whole-body bone turnover-not what’s happening in your hip or spine. Two people with the same PINP level can have very different fracture risks. That’s why they’re never used alone. They also vary naturally. Stress, illness, menstrual cycle, even time of year can affect levels. That’s why the least significant change (LSC) matters. A 20% drop in PINP or 25% drop in β-CTX-I might just be noise. You need at least a 30% change to say the treatment is working. And there’s still inconsistency in labs. Only about 65% of U.S. labs follow the standardized protocols. If your results seem odd, ask which assay was used. Roche’s Elecsys platform is widely trusted. Other tests may not be as reliable.What’s Next for Bone Turnover Markers?
The field is moving fast. New research is looking at bone alkaline phosphatase (BALP) and TRACP5b as better options for people with kidney disease. Clinical trials are testing whether using BTMs to guide treatment decisions actually reduces fractures more than standard care. Insurance coverage is improving. Medicare has covered PINP and β-CTX-I since 2020. Reimbursement is low-around $30 per test-but it’s coverage. European clinics use them routinely. In the U.S., adoption is growing, but still under 35%. The next big step? Making BTMs part of routine care-not just for specialists, but for primary care doctors too. Training programs are being developed to help clinicians interpret the numbers. Point-of-care tests are in development. Soon, you might get your BTM results before you leave the clinic.Bottom Line: BTMs Are a Game Changer
Osteoporosis treatment isn’t about guessing anymore. With bone turnover markers, you get early, objective proof that your medication is doing what it’s supposed to. No more waiting a year to find out if you’re on the right path. No more assuming you’re taking your pills because you say you are. If you’re on osteoporosis therapy, ask your doctor: “Have you checked my bone turnover markers?” If they haven’t, it’s not because they don’t matter. It’s because they’re still new to many practices. But the science is solid. The guidelines are clear. And the results? They speak for themselves.Write a comment
Items marked with * are required.






13 Comments
Jenny Lee November 18, 2025 AT 06:43
Finally, something that actually tells you if your meds are working-no more guessing games.
Shravan Jain November 19, 2025 AT 10:37
While the scientific framework presented is undeniably robust, one must question the epistemological foundations of biomarker-driven clinical decision-making. Are we not reducing the phenomenological experience of bone health to a reductive quantification? The body, after all, is not a spreadsheet.
Brandon Lowi November 20, 2025 AT 23:20
Oh, so now we’re trusting blood tests over decades of DEXA data? That’s just another way for Big Pharma to sell more tests-while Medicare pays for it. In America, we don’t need more labs-we need more accountability. And maybe a little less ‘science-speak’ that sounds fancy but doesn’t stop fractures.
Joshua Casella November 21, 2025 AT 07:18
This is exactly the kind of precision medicine we need. If you’re on a drug that costs thousands a year, you deserve to know within weeks-not years-if it’s doing anything. The 30% drop threshold isn’t arbitrary; it’s validated across multiple cohorts. This isn’t hype-it’s biology meeting accountability. Let’s stop treating osteoporosis like it’s 1998.
Richard Couron November 22, 2025 AT 01:28
They’re tracking bone markers… but who’s tracking the labs? I’ve seen results that jumped 40% overnight-no change in meds, no fracture, just a different machine. And now they want us to trust this? What if the ‘standardized’ assays are just corporate marketing? Who owns the patents on these tests? Who profits when you get retested every 3 months? I’m not buying it.
Alex Boozan November 23, 2025 AT 03:49
BTMs are the only objective, quantitative, longitudinal biomarkers validated per IOF and ECTS guidelines for real-time therapeutic monitoring. The LSC thresholds are empirically derived from multicenter longitudinal cohorts. The diagnostic sensitivity and specificity for treatment response exceed 85% in meta-analyses. Any clinician dismissing this is operating in a pre-evidence-based paradigm.
mithun mohanta November 23, 2025 AT 14:57
Let’s be real-this whole BTM thing is just another way for doctors to charge more. I got tested, they said my PINP was ‘suboptimal’… so I had to pay $200 for a ‘re-evaluation’ and then they switched my meds. Meanwhile, I’ve been taking my pills. Maybe I just have… bad bones? Or maybe the system is rigged?
Evan Brady November 23, 2025 AT 18:01
One thing people miss: BTMs don’t replace DEXA-they complement it. Think of BTMs as your car’s check engine light and DEXA as the full diagnostic scan. You don’t wait for the engine to blow before checking the light. And yes, timing matters-skip the morning fast, and your β-CTX-I looks like you just ran a marathon. I’ve seen it happen. Labs need to train their staff. This isn’t rocket science-it’s basic protocol.
Ram tech November 24, 2025 AT 02:04
uuhh so u said u need to fast? but wat if u just eat a banana? its not like ur eating pizza right? also why do u need to test at 8am? cant u just do it anytime? and why do they even make it so complicated? i just want my bones to stop breaking.
Erica Lundy November 24, 2025 AT 04:04
There is a quiet tension here between the reductionist impulse of biomarker medicine and the holistic reality of aging bone. We measure fragments, yet the body’s integrity is not reducible to plasma concentrations. One may achieve the ‘30% drop’ and still fracture. The algorithm responds to numbers-but the human body responds to time, nutrition, gravity, and meaning. Are we healing bone-or optimizing a metric?
Kevin Jones November 24, 2025 AT 17:14
BTMs are the future. Period. If your doctor hasn’t ordered them, they’re operating on a 15-year-old playbook. This isn’t ‘new science’-it’s standard of care in Europe. We’re lagging because of inertia, not evidence. Get tested. Track it. Demand better.
Premanka Goswami November 26, 2025 AT 16:10
They say BTMs are reliable-but what if the whole bone remodeling model is wrong? What if bone isn’t just breaking and rebuilding? What if it’s… communicating? With the nervous system? With the gut? With the stars? I’ve read papers-this is all just a distraction. They want you to think it’s science. It’s control.
Alexis Paredes Gallego November 26, 2025 AT 20:35
So now we’re supposed to trust blood tests from labs that can’t even spell ‘osteoporosis’ correctly? And you think the government isn’t using this to track elderly patients? ‘Oh, your PINP dropped 30%-that’s good.’ Yeah, right. Next they’ll implant microchips in your femur. This isn’t medicine-it’s surveillance with a lab coat.