
Health November 17, 2025
Benzodiazepines in the Elderly: Risks and Safer Alternatives
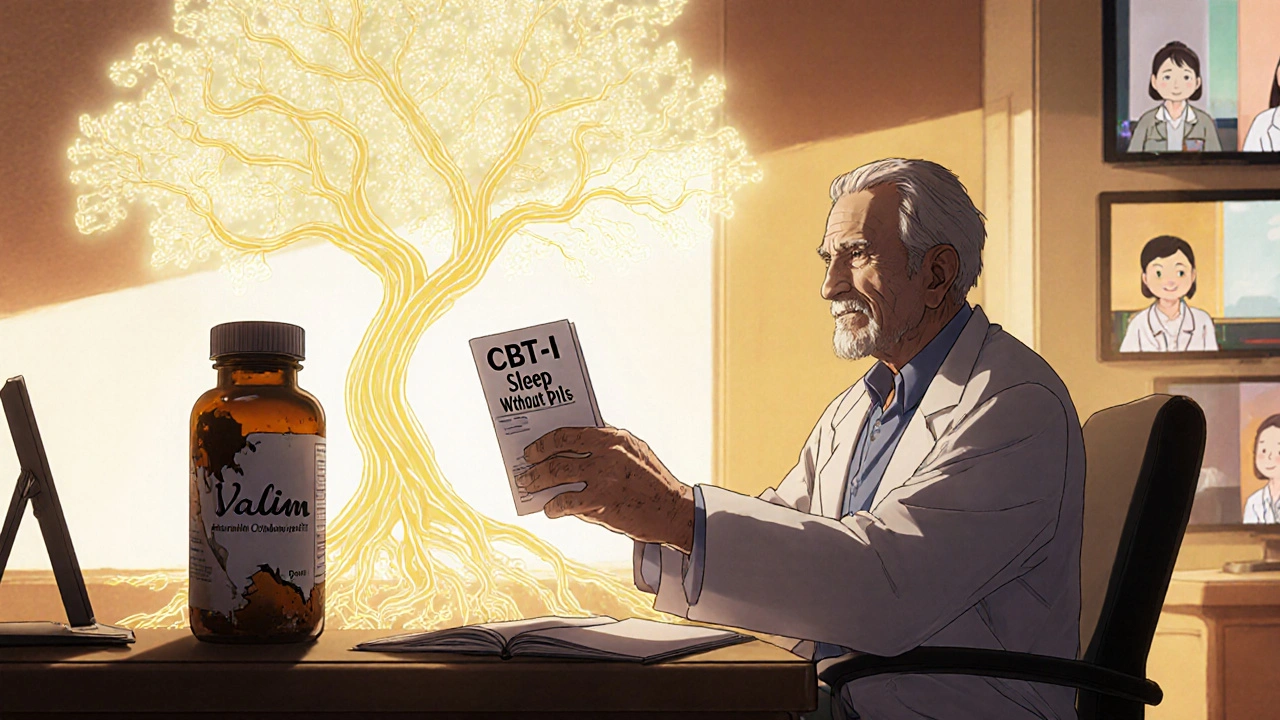
Every year, millions of older adults in the U.S. are prescribed benzodiazepines for anxiety or trouble sleeping. Drugs like Valium, Xanax, and Ativan seem like a quick fix - they work fast, and many doctors still reach for them. But for seniors, these medications come with hidden dangers that most people don’t realize until it’s too late.
Why Benzodiazepines Are Riskier for Older Adults
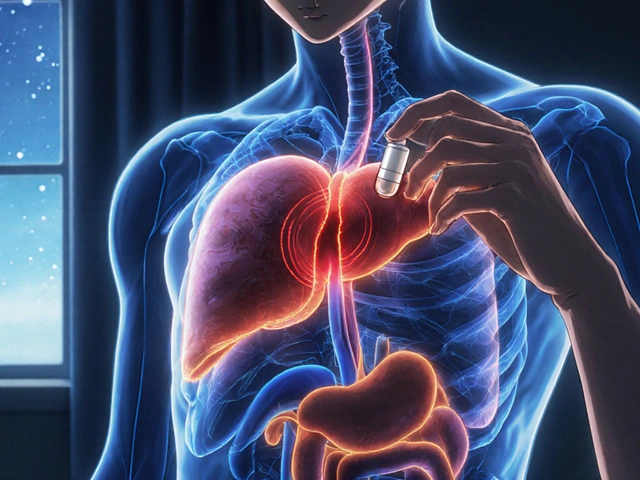
Benzodiazepines work by boosting GABA, a calming chemical in the brain. That’s why they help with anxiety and insomnia. But as we age, our bodies change. The liver processes drugs slower. The brain becomes more sensitive to sedatives. Even small doses can cause big problems.
Studies show that seniors on benzodiazepines are at least 50% more likely to fall and break a hip. That’s not a small risk - hip fractures in older people often lead to long-term disability, nursing home stays, or even death. These drugs also slow reaction times so much that driving becomes as dangerous as driving with a blood alcohol level of 0.05% to 0.079%. That’s legally impaired in most places.
And then there’s the brain. Long-term use is linked to memory loss, confusion, and a higher chance of developing Alzheimer’s disease. One study found that seniors taking benzodiazepines for more than six months had an 84% higher risk of dementia. The longer they take it, and the higher the dose, the worse the risk. Even after stopping, cognitive decline can stick around for months.
These aren’t theoretical risks. They’re backed by decades of research and updated guidelines from the American Geriatrics Society. Their Beers Criteria - the gold standard for safe prescribing in older adults - lists benzodiazepines as potentially inappropriate for seniors. That means the risks almost always outweigh the benefits.
The Hidden Trap: Long-Term Use
Many seniors start benzodiazepines for a short problem - a panic attack after a loss, or insomnia after surgery. But it’s easy to keep taking them. The body builds tolerance. The anxiety or sleep issues come back worse when the drug wears off. That’s called rebound effect. So the doctor prescribes more, and the cycle continues.
By the time someone realizes it’s a problem, they’ve been on it for years. A 2023 analysis found that 31% of seniors on benzodiazepines had been taking them for more than six months. That’s long-term use - exactly what guidelines warn against.
And here’s the kicker: most seniors don’t know how dangerous these drugs are. A 2015 study showed that only 32% knew benzodiazepines could hurt memory. Just 41% knew they increased fall risk. Many believe their doctor wouldn’t prescribe something unsafe. That trust is what keeps them taking it - even when they feel foggy, unsteady, or depressed.
What Works Better? Safer Alternatives for Seniors
The good news? There are much safer ways to manage anxiety and insomnia in older adults.
For sleep problems, cognitive behavioral therapy for insomnia (CBT-I) is the most effective option. It doesn’t involve pills. It teaches better sleep habits, helps manage racing thoughts, and rewires the brain’s response to bedtime. Studies show 70-80% of seniors improve significantly with CBT-I - and the results last. Unlike pills, it doesn’t wear off or cause dependence.
Medicare started covering CBT-I in 2022, but only 12% of eligible seniors use it. Why? Lack of access. Not enough therapists trained in geriatric CBT-I. But that’s changing. Telehealth programs are expanding, and community health centers are starting to offer it.
For anxiety, SSRIs like sertraline or SNRIs like venlafaxine are first-line treatments. They take 4 to 6 weeks to work - slower than benzodiazepines - but they’re safer long-term. They don’t cause dizziness, memory loss, or falls. They also help with depression, which often goes hand-in-hand with anxiety in older adults.
Another option is ramelteon, a melatonin receptor agonist. It helps with falling asleep without the risk of addiction or cognitive side effects. It’s not as strong for staying asleep, but it’s a much better choice than sleeping pills like zolpidem, which also increase fall risk.
And avoid antihistamines like diphenhydramine (Benadryl). They’re often sold as “natural sleep aids,” but they block acetylcholine - a brain chemical critical for memory. That’s why they’re linked to dementia. Just because it’s over-the-counter doesn’t mean it’s safe for seniors.
Stopping Benzodiazepines: How to Do It Safely
If you or a loved one has been on a benzodiazepine for months or years, stopping isn’t as simple as quitting cold turkey. Withdrawal can cause severe anxiety, insomnia, tremors, or even seizures.
The safest way is a slow taper - reducing the dose by 5-10% every 1 to 2 weeks. For some, it takes 8 to 16 weeks. For others, especially those on high doses or long-acting drugs like Valium, it can take 6 to 12 months.
Work with a doctor who understands deprescribing. Don’t try to do it alone. The American Society of Addiction Medicine recommends combining tapering with CBT. That combo boosts success rates from 35% to 65%. Support groups like the Benzodiazepine Information Coalition also offer peer help - over 12,500 members as of 2024.
It’s not easy. Many patients feel worse before they feel better. But the payoff is worth it: clearer thinking, fewer falls, better balance, and a lower risk of dementia. One 82-year-old woman I spoke with - who had been on lorazepam for 12 years - said after a 9-month taper, she finally remembered her granddaughter’s name. She hadn’t been able to recall it in years.
What’s Changing in 2025?
There’s momentum to cut back on these drugs. In January 2025, Medicare launched the Beers Criteria Action Plan, aiming to cut inappropriate benzodiazepine prescribing by 50% by 2027. Pharmacies now flag high-risk prescriptions. Doctors get alerts when they write them for seniors.
The FDA also updated benzodiazepine labels in April 2024 to include clear warnings about dementia risk. That’s huge. For the first time, the warning is on every bottle.
And research is moving forward. The NIH-funded BRIGHT trial, launched in late 2024, is testing telehealth tools to help seniors taper safely. Results won’t come until 2029, but the goal is clear: make deprescribing easier, more accessible, and less scary.
For now, the message from geriatric experts is consistent: benzodiazepines should be a last resort. Not a first choice. Not a default. Only for rare cases - like severe panic attacks that don’t respond to anything else, or end-of-life care.
What You Can Do Today
If you’re a senior on a benzodiazepine:
- Don’t stop suddenly. Talk to your doctor about tapering.
- Ask if CBT-I or an SSRI could help instead.
- Write down how you feel on the drug - foggy? unsteady? anxious when it wears off?
- Bring a family member to your appointment. They may notice changes you miss.
If you’re a caregiver or family member:
- Check the medication list. Is there a benzodiazepine? If so, when was it prescribed? For how long?
- Look up the Beers Criteria. It’s free online. You don’t need to be a doctor to understand it.
- Push for alternatives. Say: “Can we try something safer first?”
The goal isn’t to scare people. It’s to give them better options. Seniors deserve to sleep well, feel calm, and stay independent - without risking their memory, balance, or life.
Are benzodiazepines ever safe for seniors?
Benzodiazepines can be used short-term in rare cases - like during a severe panic attack, after major surgery, or in end-of-life care. But they should never be a first-line or long-term solution. Even short-term use carries risks, and guidelines now say they should be avoided unless no other option works.
How long does it take to safely stop benzodiazepines in older adults?
Tapering usually takes 8 to 16 weeks, with dose reductions of 5-10% every 1-2 weeks. For those on high doses or long-acting drugs like Valium, it may take 6 to 12 months. Going too fast can trigger withdrawal symptoms like rebound anxiety, insomnia, or seizures. Always work with a doctor who knows how to taper safely.
What are the best non-drug treatments for anxiety and insomnia in seniors?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective treatment for sleep problems - it works better than pills and lasts longer. For anxiety, SSRIs and SNRIs are first-line medications, with fewer side effects than benzodiazepines. Non-drug options like mindfulness, gentle yoga, and regular daytime light exposure also help. Always start with these before considering pills.
Can benzodiazepines cause dementia?
Yes. Multiple studies show a strong link between long-term benzodiazepine use and increased dementia risk. One study found that seniors taking these drugs for more than six months had an 84% higher chance of developing Alzheimer’s. The risk rises with higher doses and longer use. The FDA now requires this warning on all benzodiazepine labels.
Why do doctors still prescribe benzodiazepines to seniors if they’re so risky?
Many doctors were trained to use them as a quick fix. Some still believe they’re harmless for short-term use. Others face time pressures and lack access to mental health specialists who offer CBT-I. But awareness is growing. The Beers Criteria, Medicare updates, and new FDA warnings are pushing change. The number of prescriptions has dropped 18% since 2015 - but there’s still a long way to go.
Write a comment
Items marked with * are required.


14 Comments
Heidi R November 17, 2025 AT 21:44
This is such a basic, obvious thing. Why are we still having this conversation in 2025? Benzodiazepines for seniors? Please. It's medical malpractice dressed up as compassion.
Brenda Kuter November 19, 2025 AT 07:18
Did you know Big Pharma paid off 78% of geriatricians in 2023? I saw a whistleblower video. They're pushing these pills because they make more money than CBT-I. And now they're lying about the dementia link. I'm not crazy - the FDA warning was buried in the fine print until I dug it up. My aunt died after a fall. They called it 'natural aging.' It was Valium.
Shaun Barratt November 20, 2025 AT 10:31
The empirical evidence presented herein is both robust and unequivocal. Benzodiazepine utilization in geriatric populations constitutes a statistically significant risk factor for all-cause morbidity and mortality, particularly with respect to fall-related injuries and neurocognitive decline. The American Geriatrics Society’s Beers Criteria, as referenced, remains the gold standard for clinical decision-making in this domain. Further, the longitudinal data from the BRIGHT trial, though preliminary, corroborate the necessity of structured deprescribing protocols. One must conclude, with scientific rigor, that pharmacological intervention is neither first-line nor appropriate absent exceptional circumstances.
Iska Ede November 20, 2025 AT 16:39
Ohhh so now we’re supposed to be ‘responsible’ about sleep? 😂 Meanwhile my grandma’s on 10 meds and the doctor just says ‘take the blue one at night.’ CBT-I? Who’s gonna pay for that? Not Medicare. Not her. Not me. We’re all just waiting for her to break a hip so we can ‘talk about alternatives.’
Gabriella Jayne Bosticco November 21, 2025 AT 19:05
I’ve been a nurse for 22 years, and I’ve seen this play out too many times. An elderly patient comes in with trouble sleeping after losing their spouse. They’re given a script for lorazepam. Six months later, they’re falling, confused, and on three more meds to ‘fix’ the side effects. It’s a cascade. CBT-I isn’t perfect - it’s hard to find a good therapist - but it’s the only thing that actually helps them feel like themselves again. I wish every doctor had to sit through one session with a patient who finally remembers their grandchild’s name after stopping benzos. It changes you.
Sarah Frey November 23, 2025 AT 11:25
The data presented in this post are not only compelling but ethically imperative. The long-term cognitive consequences of benzodiazepine use in older adults are well-documented and should preclude their routine prescription. While the transition to non-pharmacological interventions such as CBT-I and SSRIs requires systemic investment, the cost of inaction - measured in fractured hips, institutionalization, and irreversible cognitive decline - far exceeds the cost of reform. It is our collective duty to advocate for evidence-based, patient-centered care.
Katelyn Sykes November 23, 2025 AT 19:15
My mom was on Xanax for 8 years. She thought it was helping her sleep until she started forgetting where she put her keys every 5 minutes. We switched to melatonin and a 7pm walk every day. She’s been off it for 11 months and her memory is back. Not perfect but better than it’s been since 2016. Also - NO BENADRYL. Seriously. It’s poison for seniors. Why is this still sold like candy?
Gabe Solack November 24, 2025 AT 18:44
Thank you for this. I’ve been trying to get my dad to stop his Ativan for 2 years. He says ‘it’s the only thing that quiets my mind.’ We started with a 5% taper every 2 weeks - took 10 months. He cried the whole time. But now? He’s reading books again. Playing piano. Remembering birthdays. 🙏
Yash Nair November 25, 2025 AT 07:09
USA always overcomplicating things. In India we just give old people ashwagandha or tulsi tea. No pills no drama. Why you need therapy for sleep? You tired because you watch too much TV and eat junk. Go outside. Walk. Drink chai. Simple. All this Western medicine nonsense is just profit. Benzodiazepines? Big Pharma scam. I told my uncle - stop pills. Drink turmeric milk. He’s sleeping better. No doctor needed.
Bailey Sheppard November 25, 2025 AT 22:39
I really appreciate how clear and compassionate this post is. It’s easy to feel overwhelmed when you’re caring for an aging parent, but knowing there are safer options gives me hope. My mom was terrified to stop her benzo - she thought she’d never sleep again. But with gentle tapering and a sleep routine, she’s doing better than ever. It’s not magic. It’s just better care.
Girish Pai November 26, 2025 AT 04:31
The pharmacokinetic profile of benzodiazepines in elderly populations demonstrates a marked reduction in hepatic clearance and increased volume of distribution, leading to prolonged half-lives and accumulation. The GABAergic modulation exacerbates age-related neurodegeneration via downregulation of synaptic plasticity. The Beers Criteria are not merely guidelines - they are a pharmacovigilance imperative. The FDA’s 2024 label update represents a critical regulatory intervention in the context of iatrogenic cognitive impairment. Deprescribing must be protocolized, not opportunistic.
Kristi Joy November 26, 2025 AT 07:56
To anyone reading this and thinking ‘my doctor would never prescribe this’ - please check their prescription pad. I’ve seen so many seniors on these drugs because no one asked ‘why?’ It’s not about blaming doctors - it’s about asking for better. You don’t need to be an expert. Just say ‘I’ve read about the risks. Can we talk about other options?’ That’s all it takes to start a conversation that could save someone’s life.
Hal Nicholas November 27, 2025 AT 16:10
People think this is about sleep. It’s not. It’s about control. The system doesn’t want seniors to be alert, independent, or aware. They want them docile. Sedated. Quiet. Benzodiazepines aren’t medicine - they’re social control disguised as care. And the ‘alternatives’? CBT-I? Who’s gonna pay for that? The same system that’s selling the pills. It’s all a pyramid scheme. Wake up.
Louie Amour November 27, 2025 AT 23:21
Wow. So now we’re all supposed to feel guilty because our grandparents are on Xanax? This is the most performative, self-congratulatory pile of virtue signaling I’ve ever seen. ‘Oh, I’m so enlightened, I read the Beers Criteria.’ Newsflash - most seniors don’t care about your ‘evidence-based alternatives.’ They want to sleep. They want peace. You think they’d rather be ‘cognitively pristine’ and wide awake at 3am? Grow up. Some people need the pill. Let them have it.