
Health October 3, 2025
Urispas (Flavoxate) vs Alternatives: Which Bladder Spasm Drug Is Right for You?
Bladder Spasm Medication Comparison Tool
No Dry Mouth No Constipation £4-£6/month
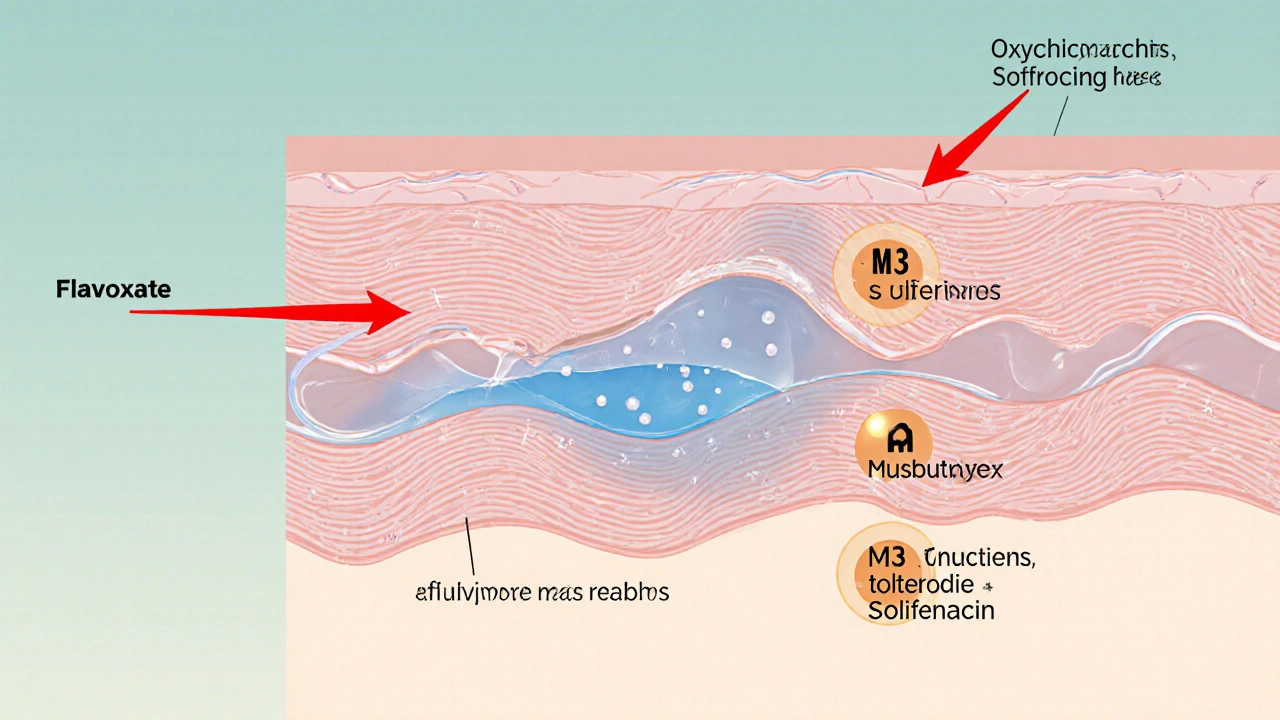
Direct smooth-muscle relaxant. Works by stabilizing bladder muscle membranes.
Dry Mouth Constipation £10-£45/month
Non-selective anticholinergic. Blocks M3 receptors in bladder.
Mild Dry Mouth Low Cognitive Effects £12-£35/month
Selective muscarinic antagonist. Less cognitive impact than oxybutynin.
Dry Mouth Constipation £15-£45/month
Highly selective M3 antagonist. Once-daily dosing preferred.
- Flavoxate: Direct smooth-muscle relaxant
- Oxybutynin: Non-selective anticholinergic (blocks M1/M3)
- Tolterodine: Selective muscarinic antagonist (M1/M3)
- Solifenacin: Highly selective M3 antagonist
- Flavoxate: Patients needing mild relief with fewer side effects
- Oxybutynin: Strong urgency control but with more side effects
- Tolterodine: Patients with mild to moderate symptoms seeking reduced side effects
- Solifenacin: Long-acting once-daily dosing for chronic management
Flavoxate is suitable for mild cases; anticholinergics offer stronger control.
Flavoxate avoids dry mouth and constipation; anticholinergics may cause these.
Avoid anticholinergics in glaucoma, enlarged prostate, or severe constipation.
Quick Take
- Flavoxate (Urispas) is a direct smooth‑muscle relaxant, not an anticholinergic.
- Anticholinergics such as oxybutynin, tolterodine and solifenacin work by blocking acetylcholine receptors.
- Flavoxate tends to cause fewer dry‑mouth and constipation issues but may be less effective for severe urgency.
- Cost varies: generic flavoxate is cheap in the UK, while newer anticholinergics can be pricier.
- Kidney function, glaucoma, and certain heart conditions dictate which drug is safest.
When you’re trying to calm bladder spasms, you’ll hear names like Flavoxate, oxybutynin, and solifenacin tossed around. All aim to ease urgency and frequency, but they do it in very different ways. This guide breaks down the science, the side‑effect profiles, and the practical considerations so you can decide which option fits your lifestyle and health status.
What Is Flavoxate (Urispas)?
Flavoxate is a muscle‑relaxing antispasmodic used primarily for urinary bladder irritability and detrusor overactivity. It was first approved in the 1970s and is marketed in the UK under the brand name Urispas.
Flavoxate works by stabilising the smooth‑muscle cell membrane, reducing the sensitivity of the bladder wall to irritants. It does not block the neurotransmitter acetylcholine, which means it avoids many classic anticholinergic side effects like dry mouth and blurred vision.
How Do the Common Alternatives Work?
The most widely prescribed rivals belong to the anticholinergic class. Below are the three big players you’ll encounter:
Oxybutynin is an anticholinergic that blocks M3 muscarinic receptors in the bladder, reducing involuntary contractions. It’s available as a tablet, patch, and gel.
Tolterodine is a selective muscarinic antagonist that offers a slightly smoother side‑effect profile than oxybutynin. It comes in immediate‑release and extended‑release forms.
Solifenacin is a highly selective M3 antagonist, marketed as a once‑daily tablet that tends to cause less constipation than older agents. It’s often reserved for patients who need a long‑acting option.
Other anticholinergics like darifenacin and propiverine fall into the same mechanism bucket but differ in dosing frequency and cost.
Side‑Effect Landscape
Because the mechanisms differ, the side‑effect profiles are distinct. Here’s a quick snapshot:
- Flavoxate: mild dizziness, headache, rare hepatic enzyme changes.
- Oxybutynin: dry mouth (up to 60% of users), constipation, blurred vision, possible cognitive slowing in older adults.
- Tolterodine: moderate dry mouth, occasional urinary retention, lower incidence of cognitive effects.
- Solifenacin: dry mouth (lower than oxybutynin), constipation, rare tachycardia.
Patients with glaucoma, prostate enlargement, or severe constipation should steer clear of strong anticholinergics. Flavoxate is generally safer for these conditions but may be less potent for intense urgency.
Comparison Table
| Attribute | Flavoxate (Urispas) | Oxybutynin | Tolterodine | Solifenacin |
|---|---|---|---|---|
| Mechanism | Direct smooth‑muscle relaxant | Non‑selective anticholinergic (M1/M3) | Selective anticholinergic (M1/M3) | Highly selective M3 antagonist |
| Typical dose (UK) | 200mg 2-3×daily (tablet) | 5mg 2-3×daily (tablet) or 3mg/24h patch | 2mg daily (ER) or 1mg immediate‑release | 5mg daily (tablet) |
| Onset of relief | 30-60min | 30min (tablet), 2h (patch) | 1-2h | 2-3h |
| Common side effects | Dizziness, headache | Dry mouth, constipation, blurred vision | Dry mouth, mild constipation | Dry mouth, constipation, occasional tachycardia |
| Key contraindications | \nSevere hepatic impairment | Glaucoma, urinary retention, MAO‑I use | Severe urinary retention, uncontrolled narrow‑angle glaucoma | Severe liver disease, uncontrolled narrow‑angle glaucoma |
| Average monthly cost (NHS) | £4-£6 (generic) | £30-£45 (brand) / £10-£15 (generic) | £25-£35 (brand) / £12-£18 (generic) | £35-£45 (brand) / £15-£22 (generic) |
| Regulatory status (UK) | Approved, prescription‑only | Approved, prescription‑only | Approved, prescription‑only | Approved, prescription‑only |
How to Pick the Right Option for You
Choosing isn’t just about price. Consider these decision points:
- Severity of symptoms: If urgency is modest, flavoxate’s milder action may be enough. For frequent, strong urges, an anticholinergic often provides better control.
- Side‑effect tolerance: Dry mouth and constipation can be annoying, especially for older adults. Flavoxate sidesteps these, making it attractive for patients with existing GI issues.
- Other health conditions: Glaucoma, enlarged prostate, or severe constipation push you toward flavoxate or a low‑dose anticholinergic like tolterodine.
- Medication burden: Once‑daily solifenacin wins for people who hate multiple pills, while flavoxate requires 2-3 doses daily.
- Cost and NHS coverage: Generic flavoxate is the cheapest. Some anticholinergics may need a prescription pre‑authorization, affecting out‑of‑pocket cost.
Discuss these factors with your GP or urologist. They can run a simple bladder diary to gauge urgency frequency and help you weigh the trade‑offs.
Practical Tips for Using These Medications
- Take flavoxate with food to reduce occasional stomach upset.
- If you start oxybutynin, stay hydrated and consider sugar‑free gum to combat dry mouth.
- Tolterodine’s extended‑release tablet should be swallowed whole-crushing destroys its release profile.
- Solifenacin works best when taken at the same time each day; missing a dose by more than 12hours may reduce efficacy.
- Monitor blood pressure and heart rate if you have cardiac disease, especially with solifenacin.
When to Call Your Doctor
Even the best‑chosen drug can backfire. Seek medical advice if you notice:
- Sudden inability to empty the bladder (acute urinary retention).
- Severe constipation lasting more than a week.
- Vision changes, especially blurred near vision.
- Marked dizziness or fainting spells.
- Persistent liver‑function test abnormalities (rare with flavoxate).
Early intervention prevents complications like urinary tract infections or kidney damage.
Frequently Asked Questions
Can flavoxate be used for overactive bladder (OAB)?
Flavoxate is officially approved for bladder irritation and detrusor overactivity, which overlap with OAB symptoms. However, many clinicians reserve it for patients who cannot tolerate anticholinergics.
Is it safe to combine flavoxate with an anticholinergic?
Co‑therapy is rarely recommended because both act on the same bladder muscles, increasing the risk of urinary retention. Your doctor would only consider it in very specific, monitored cases.
How long does it take to see improvement?
Flavoxate usually starts relieving irritation within an hour, while anticholinergics may need 2-3 days of consistent dosing for full effect.
Are there any dietary restrictions?
No strict bans, but avoid grapefruit juice with solifenacin because it can raise drug levels. Alcohol can worsen dizziness from flavoxate, so limit intake.
What monitoring is required?
Baseline liver function tests for flavoxate, and renal function for most anticholinergics, especially in patients over 65. Follow‑up after 4 weeks to assess efficacy and side effects.
In the end, the “best” drug is the one that eases your symptoms without adding new problems. Flavoxate offers a gentler side‑effect profile, while anticholinergics like oxybutynin, tolterodine, and solifenacin provide stronger urgency control. Use this comparison as a conversation starter with your healthcare provider, and you’ll be on the right track to a calmer bladder.
Write a comment
Items marked with * are required.





18 Comments
Mia Michaelsen October 3, 2025 AT 08:13
While the cost differential between flavoxate and the anticholinergics is striking, the decision really hinges on the side‑effect tolerability profile; flavoxate’s lack of dry mouth and constipation makes it a solid first‑line for patients with existing gastrointestinal concerns, whereas oxybutynin and solifenacin can exacerbate those issues. In practice, I’ve seen a number of older adults who simply can’t handle the anticholinergic burden, so opting for flavoxate can preserve quality of life without sacrificing much efficacy in mild cases. It’s also worth noting that the hepatic metabolism of flavoxate may require occasional LFT monitoring, especially in patients with known liver disease. Ultimately, a shared decision‑making approach that weighs both cost and side‑effects will yield the most satisfactory outcomes.
Kat Mudd October 11, 2025 AT 09:38
Okay so you have flavoxate which is basically a muscle relaxant that doesn’t chew up your saliva, then you have oxybutynin that will leave you feeling like you’ve been chewing on sandpaper while you’re trying to sip water, next up is tolterodine which is supposed to be the “middle‑ground” but still manages to make you chase the bathroom for a snack, and finally solifenacin that promises once‑daily dosing but secretly charges you an arm and a leg for the privilege. The thing is, every one of these drugs comes with its own set of quirks – flavoxate may give you a light headache, oxybutynin can turn your mouth into a desert, tolterodine sometimes leads to mild urinary retention and solifenacin can occasionally cause a racing heart. If you’re on a tight budget the cheap flavoxate is a no‑brainer, yet if your symptoms are raging like a storm you might need the heavier hitters. Keep in mind that many of these medications also interact with other prescriptions, especially those that are metabolized by cytochrome P450 enzymes, which can lead to unexpected spikes in blood levels. For patients with glaucoma the anticholinergics are a red flag because they can increase intra‑ocular pressure, so flavoxate becomes the safer bet. Age also plays a big role; older adults are more susceptible to cognitive slowing from anticholinergics, making flavoxate or low‑dose tolterodine more appealing. The dosing frequency is another practical consideration – flavoxate asks you to pop a pill two to three times a day while solifenacin lets you forget about it once a day, which can be a life‑saver for people with chaotic schedules. Side‑effects like constipation can be managed with diet and fiber, but dry mouth often requires constant sipping of water or sugar‑free gum, which not everyone finds convenient. Some clinicians even combine low‑dose flavoxate with an anticholinergic for synergistic effect, but that strategy should only be undertaken under close medical supervision to avoid urinary retention. In the end, the “right” drug is the one that balances symptom control, side‑effect burden, cost, and your personal lifestyle – there’s no universal answer, just a personalized match.
Pradeep kumar October 19, 2025 AT 11:03
The pharmacodynamic distinction between a direct smooth‑muscle relaxant such as flavoxate and the muscarinic antagonists pivots on receptor occupancy versus membrane stabilization. Flavoxate attenuates detrusor overactivity by modulating intracellular calcium flux without impeding acetylcholine signaling, thereby preserving autonomic tone. Conversely, oxybutynin, tolterodine, and solifenacin exhibit competitive inhibition at M3 receptors, reducing parasympathetic drive but at the expense of xerostomia and decreased gastrointestinal motility. From a therapeutic index perspective, flavoxate offers a favorable safety margin in patients with comorbid glaucoma or prostatic hypertrophy, where anticholinergic blockade could precipitate acute urinary retention. Moreover, the half‑life variability-30‑60 minutes for flavoxate versus 24‑48 hours for solifenacin-necessitates distinct dosing regimens, influencing adherence. In clinical practice, the selection algorithm should incorporate symptom severity scales, renal clearance calculations, and pharmacogenomic data where available.
James Waltrip October 27, 2025 AT 11:27
What they don’t tell you in the glossy pamphlets is that the pharmaceutical conglomerates have engineered these anticholinergics to create a dependency loop, subtly nudging patients toward higher‑priced brand names while keeping newer agents like flavoxate under the radar. It’s no coincidence that the major trials for solifenacin were funded by the same parent company that owns the majority of urology clinics. If you look at the patent timelines, you’ll see a coordinated rollout designed to sideline older, cheaper generics. The truth is, most of the side‑effects are exaggerated to scare people away from the cheap alternatives, ensuring a steady revenue stream for the big pharma lobby.
Chinwendu Managwu November 4, 2025 AT 12:52
😂 cheap meds win every time.
Kevin Napier November 12, 2025 AT 14:17
Great rundown! If you’re unsure which route to take, start with a low dose of flavoxate to gauge tolerance, then reassess after a couple of weeks. It’s always a good idea to keep a symptom diary – note frequency, urgency, and any side‑effects – so you can have an informed conversation with your clinician.
Sherine Mary November 20, 2025 AT 15:41
Honestly, the over‑hyped anticholinergics feel like chemical shackles for the bladder. Flavoxate’s milder profile is underrated, but even that can cause odd headaches if you’re not careful with dosing. Keep an eye on liver panels; you don’t want to miss a silent rise.
Monika Kosa November 28, 2025 AT 17:06
Just a heads‑up: the “official” guidelines often omit the fact that long‑term anticholinergic use has been linked to subtle neuro‑degeneration. If you’re reading between the lines, flavoplate (flavoxate) feels like the safer, less conspiratorial option.
Gail Hooks December 6, 2025 AT 18:31
Every choice reflects a deeper cultural narrative about how we value comfort over cost 🌍💡. Embracing flavoxate can be a quiet rebellion against the hype machine. 🤔✨
Derek Dodge December 14, 2025 AT 19:56
i think flavoxate is ok but u need to watch out for dizzines and headcehs lol
AARON KEYS December 22, 2025 AT 21:20
From a grammatical standpoint, the comparison table is well‑structured, presenting each attribute in a clear, parallel format. This facilitates rapid scanning and helps patients align their priorities with the drug profiles.
Summer Medina December 30, 2025 AT 22:45
Look you cant deny the cheapness of flavoxate but the way the paper glosses over the hepatic risks is just lazy, the authors skip the fact that flavoxate is metabolised by liver enzymes that can be overloaded in patients with existing conditions, also the table says dry mouth is not a problem but some users report mild dryness that the guide ignores, the cost argument is oversimplified because generic pricing fluctuates, the anticholinergic side effects are well documented but the guide pretends they’re negligible, the recommendation for severe cases to go straight to solifenacin feels like a sales pitch, the dosing schedule for flavoxate is three times daily which many patients find inconvenient, the lack of mention of drug‑drug interactions with common antihypertensives is a glaring omission, the article also fails to address adherence issues with multiple daily dosing, overall the piece reads like a marketing brochure rather than an unbiased medical review.
Melissa Shore January 8, 2026 AT 00:10
Reading through the comparison, it becomes evident that each medication brings its own trade‑offs. Flavoxate’s advantage is its minimal anticholinergic burden, which is especially relevant for patients prone to dry mouth or constipation. However, the need for multiple daily doses may affect compliance, particularly for those with busy schedules. Oxybutynin, while potent, carries a higher risk of cognitive effects, a crucial consideration for elderly patients. Tolterodine strikes a balance with moderate efficacy and a somewhat reduced side‑effect profile, making it a reasonable middle ground. Solifenacin’s once‑daily regimen is convenient, yet its cost can be prohibitive without insurance coverage. Ultimately, the decision should be individualized, weighing symptom severity, comorbidities, financial constraints, and patient preference.
Michelle Pellin January 16, 2026 AT 01:34
Ah, the drama of choosing a bladder spasm drug! One could compose an epic saga where flavoxate is the humble underdog, while the anticholinergics are the flamboyant knights swaggering onto the battlefield. Yet, in the quiet moments, it is the modest, side‑effect‑light hero that often wins the day for the weary patient.
Keiber Marquez January 24, 2026 AT 02:59
Flavoxate is just cheap junk.
Lily Saeli February 1, 2026 AT 04:24
Choosing a medication is a moral decision; we must prioritize patient dignity over profit. Opting for the least intrusive therapy respects the body’s natural balance.
Joshua Brown February 9, 2026 AT 05:48
Here’s a quick practical tip: when starting flavoxate, take it with food to minimize gastrointestinal upset; if you experience mild dizziness, stay hydrated and avoid sudden position changes. For anticholinergics, keep sugar‑free gum handy to combat dry mouth, and schedule a bowel routine to prevent constipation. Monitoring liver enzymes at baseline and after one month is advisable for flavoxate, while renal function tests should be checked periodically for the anticholinergics, especially in older adults.
andrew bigdick February 17, 2026 AT 07:13
Everyone’s experience varies, so keep tracking your symptoms and side‑effects; that data will guide a smarter conversation with your doctor.