
Health October 24, 2025
Methotrexate and Diabetes: Safety Guide & Key Considerations
When you’re living with diabetes and your doctor prescribes Methotrexate is a disease‑modifying drug often used for rheumatoid arthritis, psoriasis and certain cancers. It works by slowing cell growth and dampening immune activity. While it can be a game‑changer for inflammatory conditions, its impact on blood sugar and organ health can raise eyebrows. This guide walks you through the main safety points, monitoring tips, and how to tweak diabetes meds so you stay in control.
Key Takeaways
- Methotrexate can affect blood‑glucose levels, mainly by influencing liver function and folate status.
- Regular HbA1c checks average glucose over 2‑3 months and liver/kidney labs are essential.
- Folate supplementation (usually 1 mg daily) helps prevent spikes in glucose and reduces side‑effects.
- Adjustments to insulin or oral agents may be needed; close communication with both your rheumatologist and diabetes team is a must.
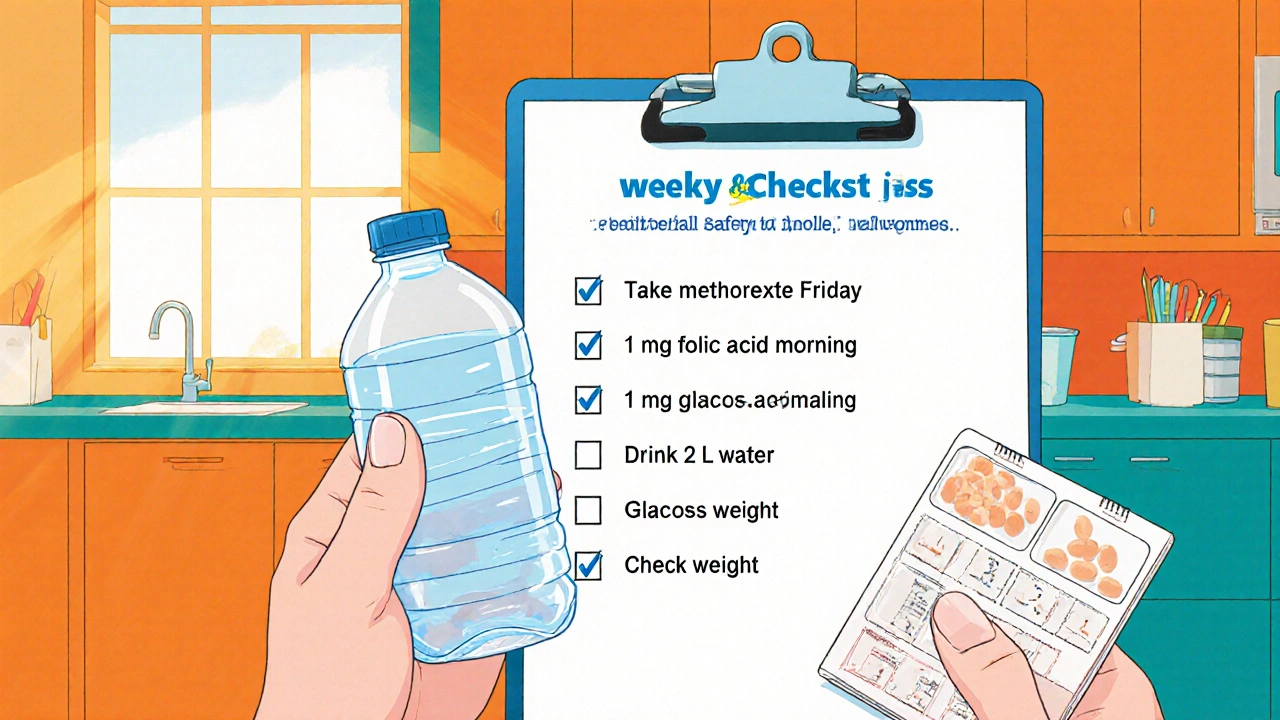
- A simple weekly checklist can catch problems early and keep you feeling steady.
What is Methotrexate?
Methotrexate is a folate antagonist that blocks dihydrofolate reductase, limiting DNA synthesis in rapidly dividing cells. In low weekly doses (7.5‑25 mg), it tames the overactive immune system that drives rheumatoid arthritis, psoriatic arthritis, and severe psoriasis. The drug is taken orally or by injection once a week, often with a day‑off after dosing to reduce nausea.
Because it interferes with folate pathways, doctors usually prescribe a daily folic acid supplement (1 mg) to offset side‑effects like mouth ulcers, liver irritation, and, for people with diabetes, potential disturbances in glucose metabolism.
How Diabetes Changes the Risk Profile
Diabetes Mellitus is a chronic condition where the body cannot properly regulate blood glucose already puts stress on the liver and kidneys. Adding methotrexate introduces three main concerns:
- Liver toxicity: Both diabetes and methotrexate can raise liver enzymes. When combined, the risk of steatosis or hepatitis climbs.
- Renal clearance: Methotrexate is excreted unchanged through the kidneys. Impaired renal function-common in long‑standing diabetes-can lead to drug accumulation and heightened toxicity.
- Folate depletion: Low folate levels can worsen insulin resistance, nudging blood glucose higher.
These interactions don’t mean you can’t use methotrexate, but they do demand tighter monitoring.

Monitoring Blood Sugar While on Methotrexate
Here’s a practical routine you can adopt:
- Baseline labs: Before starting methotrexate, get a full liver panel (ALT, AST, ALP, bilirubin), serum creatinine, eGFR, and HbA1c to capture average glucose control.
- Weekly self‑checks: Use a finger‑stick or CGM to note any unusual spikes or drops. Record the data in a log alongside methotrexate dosing days.
- Monthly labs: Repeat liver enzymes and renal function every 4-6 weeks for the first three months, then every 2-3 months if stable.
- Quarterly HbA1c: Assess whether your average glucose has shifted. An increase of ≥0.5 % may signal a need to tweak your diabetes meds.
If you spot rising liver enzymes (ALT >2× upper limit) or a sudden dip in eGFR, contact your prescriber immediately. They may pause methotrexate for a week or lower the dose.
Managing Folate and Renal Concerns
Folate supplementation is the single most effective strategy to keep glucose steady while on methotrexate. Aim for 1 mg of folic acid daily, taken at a different time than your methotrexate dose to avoid absorption competition.
For kidney protection, stay well‑hydrated-aim for at least 2 L of fluid daily unless you have heart‑failure restrictions. Avoid NSAIDs (e.g., ibuprofen) unless your doctor says it’s safe, as they can further reduce renal perfusion.
When eGFR falls below 60 mL/min/1.73 m², discuss a dose reduction (often 15 mg → 10 mg weekly) or alternative therapies with your rheumatologist.
Adjusting Diabetes Medications
Different diabetes drugs interact with methotrexate in distinct ways:
| Medication | Potential Interaction | Management Tip |
|---|---|---|
| Metformin | Generally safe; may need dose tweak if renal function declines. | Check eGFR; if <60, consider reducing metformin dose. |
| Sulfonylureas (e.g., glipizide) | Risk of hypoglycemia if liver metabolism is altered. | Monitor fasting glucose closely after each methotrexate dose. |
| SGLT2 inhibitors | May increase dehydration risk, especially with high fluid loss from methotrexate side‑effects. | Ensure adequate hydration; watch for signs of ketoacidosis. |
| Insulin | Dose may need adjustment if glucose trends shift. | Re‑evaluate basal rates after the first month of therapy. |
In practice, most clinicians keep the diabetes regimen unchanged unless lab or glucose logs show a clear trend. When a change is needed, do it gradually-adjust one medication at a time and give at least one week to see the effect.
Practical Checklist for Patients on Methotrexate with Diabetes
- Take methotrexate on a set day each week (e.g., every Friday).
- Consume 1 mg folic acid daily, preferably in the morning.
- Log daily glucose readings, noting the day you took methotrexate.
- Check weight and blood pressure weekly; sudden drops may hint at dehydration.
- Attend the first three lab appointments (liver panel, creatinine, HbA1c) as scheduled.
- Stay hydrated-aim for 2 L of water, more if you exercise.
- Inform any new prescriber (e.g., dentist, surgeon) that you’re on weekly methotrexate.
- Report any yellowing of skin/eyes, persistent nausea, or unexplained fatigue immediately.
Following this routine keeps you ahead of potential problems and gives your care team actionable data.
Frequently Asked Questions
Can methotrexate raise my blood sugar?
It doesn’t directly increase glucose, but liver stress and folate depletion can make insulin work less efficiently, causing modest rises in fasting glucose.
Do I need to stop my diabetes medication when starting methotrexate?
Usually no. Your diabetes regimen stays the same unless labs or glucose logs show a pattern that warrants a tweak.
How often should I get liver function tests?
Every 4‑6 weeks for the first three months, then every 2‑3 months if results are stable.
Is folic acid enough, or do I need a stronger supplement?
A daily 1 mg folic acid dose is standard and works for most people. If your doctor notices persistent low folate levels, they may increase it to 5 mg weekly.
Can I take ibuprofen for joint pain while on methotrexate?
Occasional short‑term use is okay, but regular NSAIDs can worsen kidney function, so discuss alternatives like acetaminophen with your doctor.
Balancing methotrexate with diabetes isn’t magic-it’s about vigilance, communication, and a few simple habits. By keeping an eye on liver and kidney labs, staying on folic acid, and tweaking diabetes meds when needed, you can enjoy the anti‑inflammatory benefits without derailing your glucose control. methotrexate diabetes safety starts with informed decisions and a proactive care team.
Write a comment
Items marked with * are required.



10 Comments
Deborah Galloway October 24, 2025 AT 20:53
Thanks for the clear rundown-super helpful!
Benjamin Sequeira benavente October 24, 2025 AT 21:43
Look, if you’re already battling blood‑sugar swings, adding methotrexate isn’t a walk in the park. Your liver’s already on overtime from diabetes, so you need to keep those enzymes in check like a hawk. Hydration is key – think two‑liters a day unless your heart says otherwise. Pair your weekly dose with a separate folic acid pill to dodge the insulin‑resistance trap. And don’t forget to flag any sudden HbA1c jump with your endocrinologist ASAP.
Stay sharp, stay steady.
Charlie Stillwell October 24, 2025 AT 23:06
Alright, let’s dive deep into the methotrexate‑diabetes tango. First off, methotrexate is a folate antagonist that throws a wrench into the dihydrofolate reductase pathway, which, in lay terms, messes with DNA synthesis in rapidly dividing cells. This pharmacodynamic action is great for quelling autoimmune fires, but it also drags folate levels down, a nutrient that plays a pivotal role in insulin signaling. Low folate can amplify insulin resistance, nudging your glucose readings upward – yep, that’s a textbook example of a collateral effect. On top of that, the liver, already a metabolic workhorse for glucose homeostasis, has to metabolize the drug, raising the specter of hepatotoxicity, especially when you have concomitant non‑alcoholic fatty liver disease common in type‑2 diabetics. ☝️ Renal clearance is the other Achilles’ heel; methotrexate is excreted unchanged, so any diabetic nephropathy can cause drug accumulation and toxic spikes. The clinical guideline is simple: monitor ALT, AST, and bilirubin monthly, and check eGFR every 4‑6 weeks until you’re stable. If ALT spikes beyond twice the upper limit, consider a dose pause – it’s not a death sentence, just a safety checkpoint. Meanwhile, keep your folic acid intake at 1 mg daily, preferably timed several hours apart from the methotrexate dose to avoid absorption competition. Hydration is non‑negotiable; think two liters of water daily, unless contraindicated, to keep the kidneys flushing the drug out efficiently. 📊 For diabetes meds, metformin stays mostly safe but requires eGFR monitoring; sulfonylureas may need dose reduction if renal function declines. Insulin regimens might need tweaking – a modest basal reduction can offset the glucose‑raising effect of folate depletion. The good news is that with vigilant labs and a disciplined logbook, most patients sail through without major hiccups. In practice, a weekly checklist that logs dose day, folate intake, water volume, and glucose spikes can be a game‑changer. Bottom line: methotrexate can coexist with diabetes, provided you respect the monitoring protocol and stay proactive. 😊
Ken Dany Poquiz Bocanegra October 24, 2025 AT 23:15
Solid breakdown – the checklist idea really seals the deal. Keeping a log will catch any drift early.
krishna chegireddy October 25, 2025 AT 01:53
Everyone loves the hype around methotrexate, but have you considered the hidden agenda of pharma? They push it as a miracle drug while ignoring the subtle sabotage of your liver and kidneys. It’s like handing someone a sword and telling them to trust the blade. Think twice before you swallow that weekly pill.
Tamara Schäfer October 25, 2025 AT 02:01
i get what u’re saying – the liver part is scary, but i think regular labs can keep us safe. just dont forget the folic acid, it really helps.
Buddy Bryan October 25, 2025 AT 04:40
Quick tip: if your eGFR drops below 60, ask your rheumatologist about dropping the methotrexate dose to 10 mg weekly. Also, double‑check that your insulin pump settings account for any HbA1c uptick; a 10‑15% basal reduction can smooth things out. Remember to keep a hydration log – the kidneys love water. And always coordinate appointments so your endocrinologist and rheumatologist are on the same page.
Aaron Kuan October 25, 2025 AT 04:43
Love the guide keep it up
Brett Witcher October 25, 2025 AT 07:26
From a pharmacokinetic standpoint, the half‑life of methotrexate in patients with compromised renal function can extend beyond 12 hours, necessitating dose adjustments. Monitoring trough levels, though not routine, may be warranted in borderline eGFR cases.
Amber Lintner October 25, 2025 AT 07:35
Oh, so now we’re playing doctor with spreadsheets – how thrilling!