Health January 6, 2026
Cephalosporin Allergies: How Cross-Reactivity with Penicillins Really Works
Cephalosporin Cross-Reactivity Risk Calculator
Why This Matters
The outdated 10% cross-reactivity rule leads to unnecessary avoidance of cephalosporins. Modern research shows real risk is much lower based on reaction type and drug generation.
This tool helps determine your specific risk level based on clinical evidence from studies after 1980.
Your Risk Assessment
-
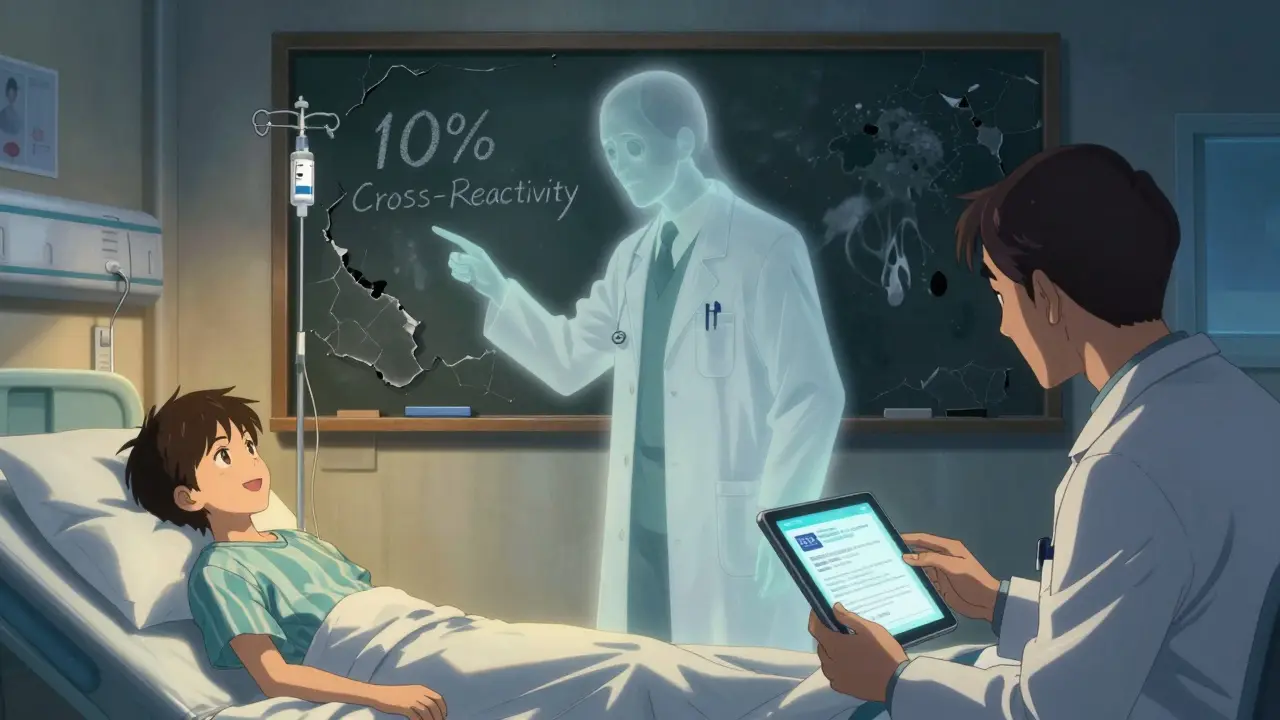
Many people believe if they’re allergic to penicillin, they can’t take cephalosporins. It’s a rule drilled into medical training for decades: 10% cross-reactivity. But that number is outdated-and it’s putting patients at risk. In reality, the chance of a true allergic reaction to a cephalosporin if you’re allergic to penicillin is far lower than most doctors still think. And using that old 10% figure is leading to unnecessary antibiotic choices, longer hospital stays, and even higher rates of dangerous infections like C. diff.
Why the 10% Rule Is Wrong
The idea that 10% of penicillin-allergic patients will react to cephalosporins came from studies in the 1960s and 70s. Back then, cephalosporin drugs weren’t pure. They were made using a mold called Cephalosporium, and trace amounts of penicillin often slipped into the final product. So when patients reacted, it wasn’t because cephalosporins were cross-reacting-it was because they were getting a little bit of penicillin mixed in. Once manufacturing improved after the 1980s, those contaminations dropped off. But the old warning stuck.Modern research tells a different story. A review of 12 studies after 1980 involving over 400 patients showed the real cross-reactivity rate is between 2% and 5%. For third- and fourth-generation cephalosporins like ceftriaxone or cefepime, it’s less than 1%. That’s not just a small adjustment-it’s a complete rethink of how we treat patients.
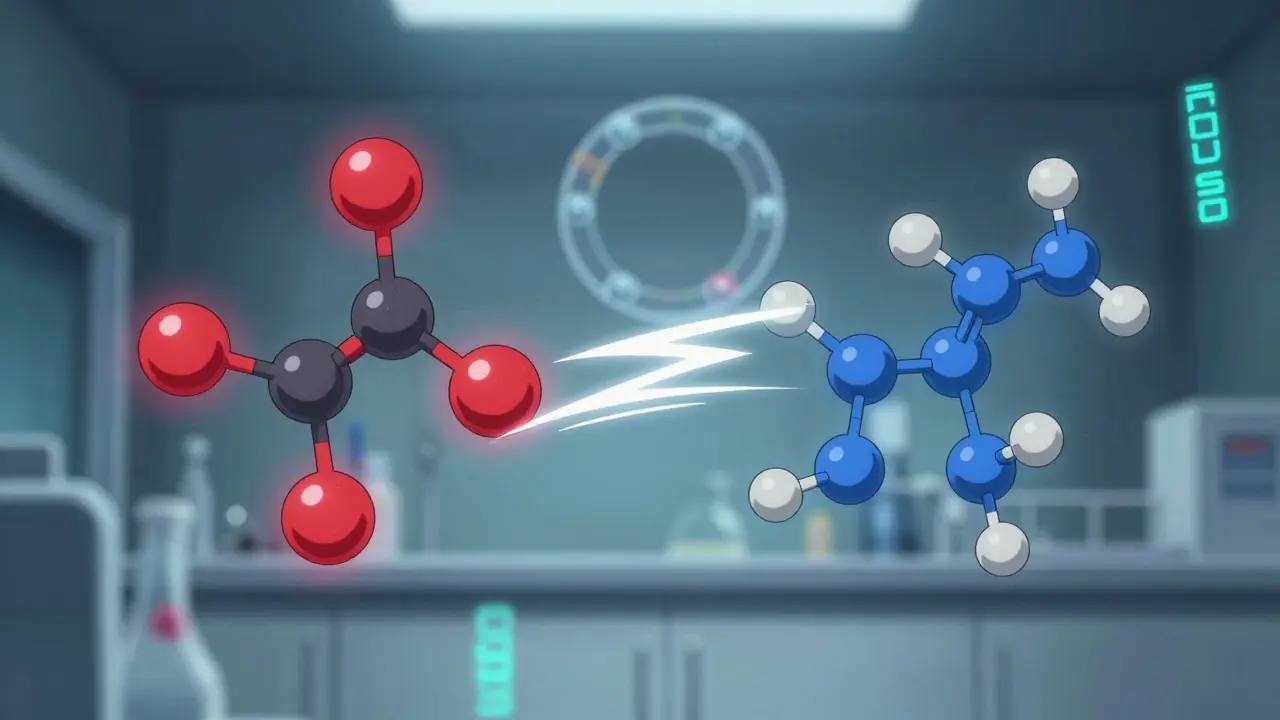
It’s Not the Ring-It’s the Side Chain
Penicillins and cephalosporins both have a beta-lactam ring, which is what makes them structurally similar. For years, doctors thought that ring was the problem. But that’s not what triggers most allergic reactions. The real culprit is the side chain-the chemical group attached to the core structure.Think of it like this: two cars might have the same engine, but if one has a red hood and the other has a blue one, they look different. Your immune system doesn’t care about the engine. It cares about the hood. In penicillins and cephalosporins, the side chain is that hood. If the side chain of the cephalosporin looks a lot like the side chain of the penicillin you reacted to, then there’s a higher risk. If it’s different? You’re probably fine.
First-generation cephalosporins like cefazolin and cephalexin have side chains that are more similar to penicillin G and ampicillin. That’s why they carry a higher risk-up to 8% in some studies. But ceftriaxone? Its side chain is completely different. So is cefixime and cefepime. That’s why the CDC says these drugs are safe for most penicillin-allergic patients, as long as they didn’t have a severe reaction like anaphylaxis in the last 10 years.
Generations Matter-Here’s What’s Safe
Not all cephalosporins are created equal. Here’s what the data shows:| Generation | Examples | Approx. Cross-Reactivity with Penicillin | Safety for Penicillin-Allergic Patients |
|---|---|---|---|
| First | Cefazolin, Cephalexin | 1%-8% | Use with caution; avoid if IgE-mediated reaction |
| Second | Cefaclor, Cefuroxime | 1%-5% | Generally safe if side chain differs |
| Third | Ceftriaxone, Cefotaxime, Cefixime | <1% | Safe for most, even with prior penicillin allergy |
| Fourth | Cefepime | <1% | Very low risk; preferred in complex cases |
For example, if you had a rash after taking amoxicillin, ceftriaxone is likely safe. But if you had anaphylaxis after penicillin, you should still be evaluated before any beta-lactam is given-even if it’s a third-gen cephalosporin. The key is distinguishing between a mild rash and a life-threatening reaction.
What Counts as a Real Allergy?
Not every bad reaction is an allergy. Many people say they’re allergic to penicillin because they got a stomachache, a headache, or a mild rash as a kid. But true IgE-mediated allergies involve symptoms like hives, swelling of the face or throat, wheezing, or anaphylaxis. Those are rare-and they’re the only ones that matter when considering cephalosporin use.Studies show that 90-95% of people who say they’re allergic to penicillin aren’t actually allergic. Skin testing can confirm this. In one large study from Kaiser Permanente, 3,313 patients with a history of “cephalosporin allergy” were given cephalosporins. Zero had anaphylaxis. Many of those so-called allergies were just side effects or misdiagnoses.
If you’ve never had a serious reaction, and you need a cephalosporin for a serious infection like pneumonia or a kidney infection, avoiding it could be riskier than using it. Broad-spectrum antibiotics like vancomycin or clindamycin are often used instead-and they’re linked to more C. diff infections, which can be deadly.
What Should You Do If You Think You’re Allergic?
If you’ve been told you’re allergic to penicillin, here’s what to do:- Don’t assume you’re allergic forever. Many people outgrow it.
- Ask your doctor about penicillin skin testing. It’s accurate, safe, and widely available.
- If the test is negative, you can likely take penicillin or any cephalosporin safely.
- If you need a cephalosporin and can’t get tested, choose a third- or fourth-generation agent like ceftriaxone or cefepime.
- Avoid first-generation cephalosporins if you had a true IgE-mediated reaction.
Even if you’ve never been tested, don’t let a childhood label stop you from getting the right treatment. Many hospitals now have allergy delabeling programs-where they systematically re-evaluate patients with reported penicillin allergies. These programs cut down on unnecessary broad-spectrum antibiotics by 10-25% and shorten hospital stays by 1-2 days.

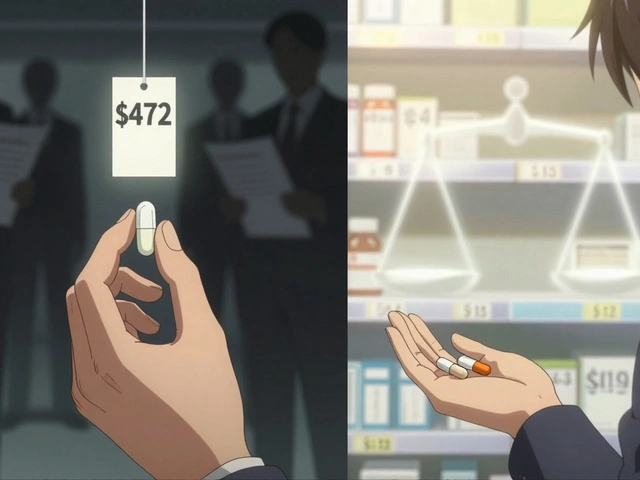
Why This Matters for Everyone
About 10% of people in the U.S. and U.K. say they’re allergic to penicillin. That’s tens of millions of people. And because of outdated beliefs, most of them are being treated with antibiotics that are less effective, more expensive, and more dangerous.When you avoid cephalosporins unnecessarily, you end up on drugs like fluoroquinolones or vancomycin. These drugs are broad-spectrum, meaning they kill good bacteria along with bad ones. That’s why C. diff infections are rising. They’re also linked to tendon ruptures, nerve damage, and antibiotic resistance.
Health systems are starting to catch on. The CDC, Medsafe (New Zealand’s drug safety agency), and major medical societies now recommend using third-generation cephalosporins in penicillin-allergic patients. But the FDA still lists a 10% cross-reactivity warning on many cephalosporin labels. That’s why doctors keep avoiding them-even when the evidence says it’s safe.
The Bottom Line
The idea that cephalosporins and penicillins are dangerously cross-reactive is a myth built on bad data. Modern science shows that cross-reactivity is rare, especially with newer cephalosporins. The real risk comes from side-chain similarity-not the beta-lactam ring. If you’ve had a mild reaction to penicillin, you’re probably fine with ceftriaxone. If you’ve had anaphylaxis, get tested before taking any beta-lactam. And if you’re a clinician, stop relying on the 10% rule. It’s costing lives-and it’s outdated.Antibiotics are powerful tools. Using them wisely saves lives. Misunderstanding cross-reactivity doesn’t just waste time-it wastes opportunity. The right drug, at the right time, can mean the difference between a quick recovery and a long hospital stay. Don’t let an old myth stand in the way of good care.
Write a comment
Items marked with * are required.





9 Comments
Alex Danner January 7, 2026 AT 17:01
For years I was taught the 10% rule like gospel. Then I saw a patient with a penicillin rash get ceftriaxone for sepsis and walk out three days later. No reaction. No drama. Just recovery. The data’s clear-most of us are still treating patients like they’re walking time bombs when they’re not. We’re overmedicating them with vancomycin just because we’re scared of outdated stats.
It’s not just inefficient-it’s dangerous. C. diff doesn’t care about your training. It just wants your gut microbiome to collapse. Time to update the protocols and stop letting myths kill more than infections.
Katrina Morris January 7, 2026 AT 21:16
i had a rash on my arm when i was 8 after amoxicillin and i’ve been avoiding all penicillins ever since. i just found out last year that i might not even be allergic? my doctor laughed and said ‘most people outgrow it’
so i got tested and turns out i’m fine. now i can take ceftriaxone if i need it. feels good to not be scared of my own medical history anymore
Rachel Steward January 8, 2026 AT 20:48
Let’s be real-this isn’t about science. It’s about institutional inertia. Doctors don’t update their knowledge because they’re too busy, too lazy, or too afraid of getting sued. The 10% myth persists because it’s easier to say ‘no’ than to think.
And don’t give me that ‘better safe than sorry’ crap. Safe for whom? The patient? Or the hospital’s liability insurance? We’re choosing convenience over care. We’re letting fear dictate treatment while patients suffer from C. diff, antibiotic resistance, and longer hospital stays because someone refused to read a 2015 meta-analysis.
The side chain argument? Brilliant. But it’s not going to change anything until medical schools stop teaching outdated crap and start teaching critical thinking. Until then, we’re just medical bureaucrats in white coats.
Adam Gainski January 9, 2026 AT 06:18
As a pharmacist, I’ve seen this play out too many times. A patient comes in with a penicillin allergy label, and we default to clindamycin or azithromycin-even when ceftriaxone would be perfect.
I started pushing for allergy delabeling in our hospital last year. We’ve done over 200 skin tests. Over 90% came back negative. We’ve cut down on vancomycin use by 30%. C. diff cases dropped. Nurses noticed patients were getting discharged faster.
It’s not magic. It’s just good medicine. If you’re a clinician and you haven’t looked into this yet, please do. It’s one of the easiest wins in patient care right now.
Elen Pihlap January 9, 2026 AT 12:08
wait so if i had a rash as a kid i can just take ceftriaxone now??
i dont even remember what happened but my mom always said no penicillin
so like... am i just allergic to being told no??
why does this feel like a trap
Sai Ganesh January 10, 2026 AT 09:54
In India, we see this too. Many patients are labeled penicillin-allergic after a simple fever or diarrhea. Doctors avoid cephalosporins out of habit, even when no real allergy exists.
Our hospitals don’t have skin testing programs like in the US. So patients get broader antibiotics-more expensive, more side effects. We need more awareness. This post is a good start.
Side chain logic makes perfect sense. It’s like two different phones with the same battery but different cases-you don’t react to the battery, you react to the case.
Paul Mason January 11, 2026 AT 05:46
Oh for crying out loud. I’m a GP and I’ve been using ceftriaxone on penicillin-allergic patients for years. The 10% rule is nonsense. I’ve had zero reactions. Zero.
And guess what? My patients get better faster. They don’t need 10 days of clindamycin with stomach cramps. They get one IV dose and go home.
Why is this even a debate? The data’s been out since 2010. Maybe we need a new rule: ‘If you haven’t read the latest guidelines, don’t prescribe antibiotics.’
Andrew N January 12, 2026 AT 09:05
So what you’re saying is, we’ve been mislabeling millions of people as allergic because we didn’t understand chemistry? And now we’re just supposed to trust that third-gen cephalosporins are safe?
What about the 5% who *do* react? What if you’re that one? Who takes responsibility then?
It’s easy to say ‘it’s just 1%’ when you’re not the one lying in the ER with anaphylaxis.
Science is great. But medicine isn’t math. It’s people. And people die when we get this wrong.
Jessie Ann Lambrecht January 14, 2026 AT 03:10
THIS. I’ve been screaming this from the rooftops since I got my first residency rotation. We’re not saving lives by avoiding cephalosporins-we’re burying them under piles of vancomycin and fluoroquinolones.
I had a 72-year-old woman with pneumonia. ‘Allergic to penicillin’ on her chart. We gave her cefepime. She walked out in 48 hours. No rash. No fever. No drama.
Meanwhile, her roommate got clindamycin and got C. diff. She’s still in rehab.
Stop being afraid of side chains. Start being brave for your patients. The science is here. The data is loud. The only thing holding us back is our own outdated ego.