
Health February 16, 2026
Corneal Ulcers: Contact Lens Risks and Urgent Care
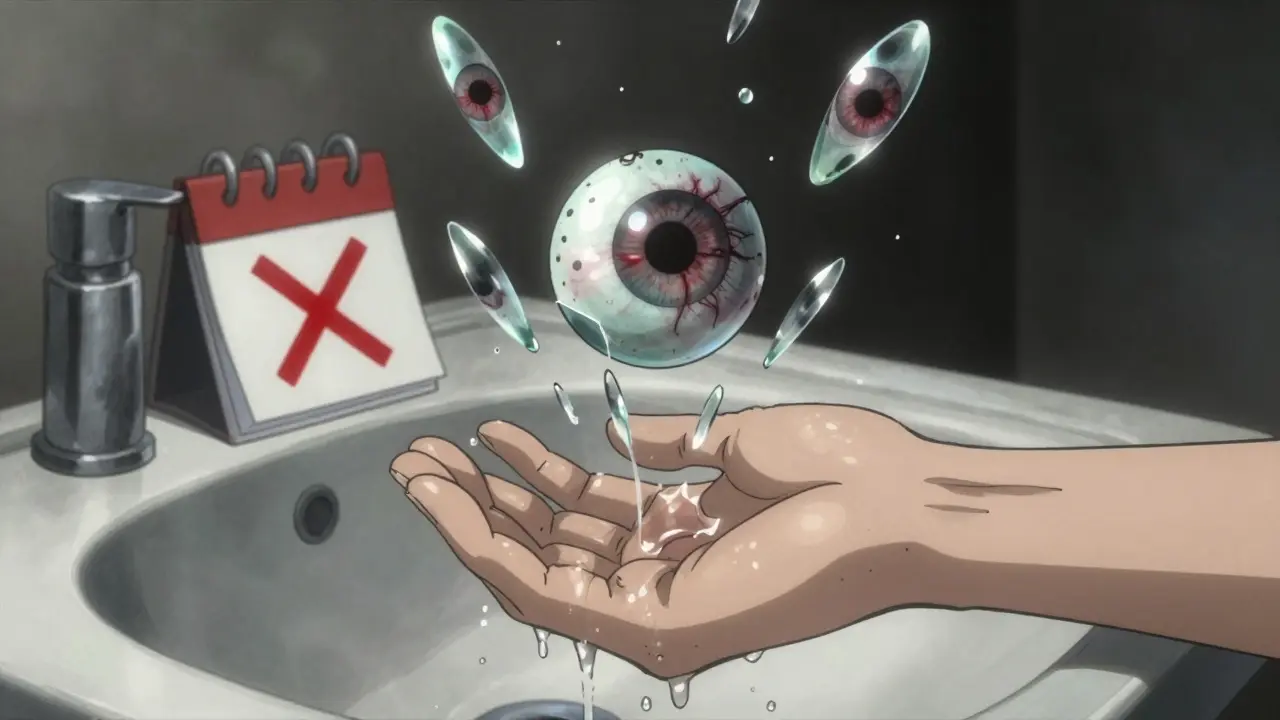
Imagine waking up with a burning sensation in your eye, blurred vision, and light so painful you have to keep it closed. This isn’t just a bad day-it could be a corneal ulcer. It’s not just a scratch. It’s an open wound on the clear front surface of your eye, often caused by bacteria, fungi, or viruses that get trapped under your contact lens. Left untreated, it can scar your cornea, steal your vision, or even lead to blindness. And yes, wearing contacts-even if you’ve done it for years-can put you at serious risk.
Why Contact Lenses Increase Your Risk
Contact lenses are convenient, but they’re not harmless. They sit directly on your cornea, blocking oxygen flow and trapping debris, bacteria, and moisture. The risk isn’t theoretical-it’s backed by data. According to the Cleveland Clinic, contact lens wearers are about 10 times more likely to develop a corneal ulcer than people who don’t wear lenses. If you sleep in them? That risk jumps to 100 times higher. The FDA calls this one of the most serious hazards of contact lens use.Soft lenses, especially extended-wear types meant for overnight use, are the biggest offenders. Why? They’re designed to be worn longer, which means more time for bacteria to build up. A single night of sleeping in lenses can turn a tiny scratch or a speck of dust into an infection. Even clean hands can transfer microbes. One study found that nearly 70% of people who wear contacts don’t wash their hands properly before touching them. And don’t think rinsing with water helps-tap water, even bottled, can carry dangerous organisms like Acanthamoeba, a parasite linked to severe, hard-to-treat infections.
What Symptoms Shouldn’t Be Ignored
Corneal ulcers don’t always start with a dramatic event. Often, they creep in slowly. But there are clear warning signs you can’t afford to ignore:- Severe eye pain, even when you’re not touching it
- Redness that won’t go away
- Blurry or hazy vision
- Sensitivity to light-turning away from sunlight or even indoor lighting
- Excessive tearing or pus-like discharge
- A white or gray spot on the colored part of your eye (the cornea)
- Feeling like something’s stuck in your eye-even when there’s nothing there
If you notice even one of these, especially if you wear contacts, don’t wait. Don’t try to “sleep it off” or use over-the-counter drops. These symptoms mean your cornea is already damaged. Delaying care by even 24 hours can mean the difference between full recovery and permanent vision loss.
How Doctors Diagnose It
Your eye doctor won’t just look at your eye and guess. They’ll use specialized tools to confirm it’s a corneal ulcer-and not just a scratch or irritation.First, they’ll put a drop of fluorescein dye in your eye. Under a special blue light, any damaged area will glow green, showing exactly where the ulcer is. Then comes the slit-lamp exam, a high-powered microscope that lets them see the depth and size of the sore. If it’s deep or large (over 2 mm), they’ll likely take a corneal scraping-gently collecting a tiny sample from the ulcer to test for bacteria, fungi, or viruses. This tells them exactly what to treat it with.
They’ll also check your visual acuity, measure your cornea’s curvature, and look for signs of swelling or spreading infection. Newer imaging systems are now able to capture high-resolution photos of ulcers, helping doctors spot problems earlier and track healing more precisely. This isn’t science fiction-it’s standard care today.

Treatment: Speed Is Everything
There’s no time to wait. Treatment must start within hours of diagnosis.For bacterial ulcers-which are the most common-doctors usually start with fluoroquinolone antibiotic eye drops. These are broad-spectrum, meaning they fight many types of bacteria at once. You’ll need to use them every hour or two at first, then taper off as it heals. If the ulcer is near the center of your vision (the visual axis) or larger than 2 mm, it’s considered sight-threatening. In those cases, they’ll pause treatment to get culture results before deciding on the next step.
If it’s a fungal infection-often from contaminated solutions or water exposure-you’ll need antifungal drops like natamycin. Viral ulcers, usually from herpes simplex, require antivirals like acyclovir. In rare cases, if the ulcer has destroyed a large part of the cornea, a corneal transplant may be the only way to restore vision.
One thing you must avoid: steroid eye drops. While they reduce swelling, they also weaken your eye’s defenses. If you use them without knowing the cause of the ulcer, you could make the infection worse. Only a doctor should prescribe them-and only after confirming the infection is under control.
How to Prevent a Corneal Ulcer
The best treatment is prevention. And it’s simpler than you think.- Never sleep in your lenses-even if they’re labeled “extended wear.” The risk is 100 times higher. Take them out every night.
- Wash your hands with soap and dry them before touching your lenses. No exceptions.
- Use only the solution your doctor recommends. Never use water, saliva, or homemade solutions. Even “sterile” saline isn’t safe for cleaning lenses.
- Replace your lenses on schedule. Don’t stretch out the life of daily, weekly, or monthly lenses. Overused lenses trap more bacteria.
- Avoid water. Don’t swim, shower, or use a hot tub while wearing contacts. Chlorine doesn’t kill all microbes-and Acanthamoeba thrives in water.
- Give your eyes a break. Wear glasses at least one day a week. Let your cornea breathe.
- Replace your case weekly. Bacteria build up in the case. Rinse it daily with solution, never water, and let it air-dry upside down.
It’s not about being perfect. It’s about being consistent. One slip-up-like sleeping in lenses once-can be enough. But if you follow these steps every day, your risk drops to near zero.
What Happens If You Ignore It
Corneal ulcers don’t heal on their own. What starts as a small sore can turn into a deep scar. That scar doesn’t go away. It blocks light from entering your eye properly. You might notice glare, double vision, or a permanent blind spot. In worst-case scenarios, the cornea can perforate-meaning your eye leaks fluid. That’s an emergency requiring immediate surgery.Even after healing, some people need lifelong vision correction. Others never regain full sight. The American Academy of Ophthalmology reports that up to 15% of severe corneal ulcers result in permanent vision loss. And that’s with treatment. Without it? The numbers are far worse.
When to Seek Help
If you wear contacts and have any of the symptoms listed above, call your eye doctor immediately. Don’t wait for an appointment. Don’t try to treat it yourself. Go to an urgent eye clinic or emergency room if you can’t reach your provider within a few hours. Time is your most valuable resource here.Stopping contact lens wear right away is step one. But stopping isn’t enough-you need professional treatment. Your eye isn’t like a scraped knee. It doesn’t heal on its own. And every hour counts.
Can you get a corneal ulcer without wearing contacts?
Yes, but it’s much less common. Trauma like a scratch from a fingernail or plant matter, severe dry eye, or viral infections like herpes simplex can cause ulcers. People with weakened immune systems or those who use steroid eye drops improperly are also at higher risk. But for most people, contact lenses are the leading cause.
How long does it take to heal from a corneal ulcer?
It depends on the cause and severity. Mild bacterial ulcers can heal in 1-2 weeks with proper treatment. Deeper or fungal ulcers may take weeks to months. Scarring can remain even after the infection clears, which may require further treatment like vision correction or surgery.
Are daily disposable lenses safer than other types?
Yes, they reduce risk significantly. Since you throw them away after one use, there’s no buildup of protein, bacteria, or debris from reuse. But they’re not risk-free. If you sleep in them, expose them to water, or don’t wash your hands, you can still get an ulcer. Hygiene matters more than the lens type.
Can you wear contacts again after a corneal ulcer?
Only after your eye doctor says it’s safe. This usually means waiting until the ulcer is fully healed, the cornea has regained strength, and you’ve had a follow-up exam. Many people are advised to switch to daily disposables and avoid overnight wear permanently. Some may be told to stop wearing contacts altogether.
Is it true that water can cause corneal ulcers?
Absolutely. Tap water, swimming pools, hot tubs, and even showers can harbor dangerous microbes like Acanthamoeba. This parasite is extremely hard to treat and can burrow into the cornea through tiny scratches. Never wear contacts in water, even if you close your eyes. The risk isn’t worth it.





