
Health January 3, 2026
How to Store Medications to Extend Their Shelf Life Safely
Most people check the expiration date on their medicine and toss it out without a second thought. But what if that pill, capsule, or liquid is still perfectly safe and effective - even after the date on the bottle? The truth is, medication storage matters far more than most realize. Improper storage can ruin a drug long before its expiration date. And with the right conditions, many medicines last years beyond what’s printed on the label.
Why Expired Medications Aren’t Always Dangerous
The expiration date on your medicine isn’t a "use-by" date like milk. It’s a guarantee from the manufacturer that the drug will remain at full potency and safety under ideal storage conditions. But that doesn’t mean it suddenly turns toxic or useless the day after. In fact, the U.S. government’s Shelf-Life Extension Program (SLEP), run by the FDA and Department of Defense since 1986, tested over 3,000 lots of 122 different drugs. The results? 88% were still stable and effective - sometimes for years past their labeled expiration. Drugs like naloxone, fentanyl, and halothane showed 100% stability even five years past their expiration. Tamiflu, stored in federal stockpiles, was cleared for use up to 10 years after manufacture. These aren’t rare exceptions. They’re proof that proper storage keeps medicine working - and saves billions in replacement costs.What Storage Conditions Actually Matter
Not all medicines are the same. How you store them makes all the difference. Here’s what works:- Keep it cool and dry: Most solid pills and capsules (like ibuprofen, antibiotics, or blood pressure meds) are fine at room temperature - between 20°C and 25°C (68°F-77°F) with humidity under 60%. Avoid storing them above 30°C or in damp places like bathrooms. Humidity breaks down coatings and causes pills to crumble.
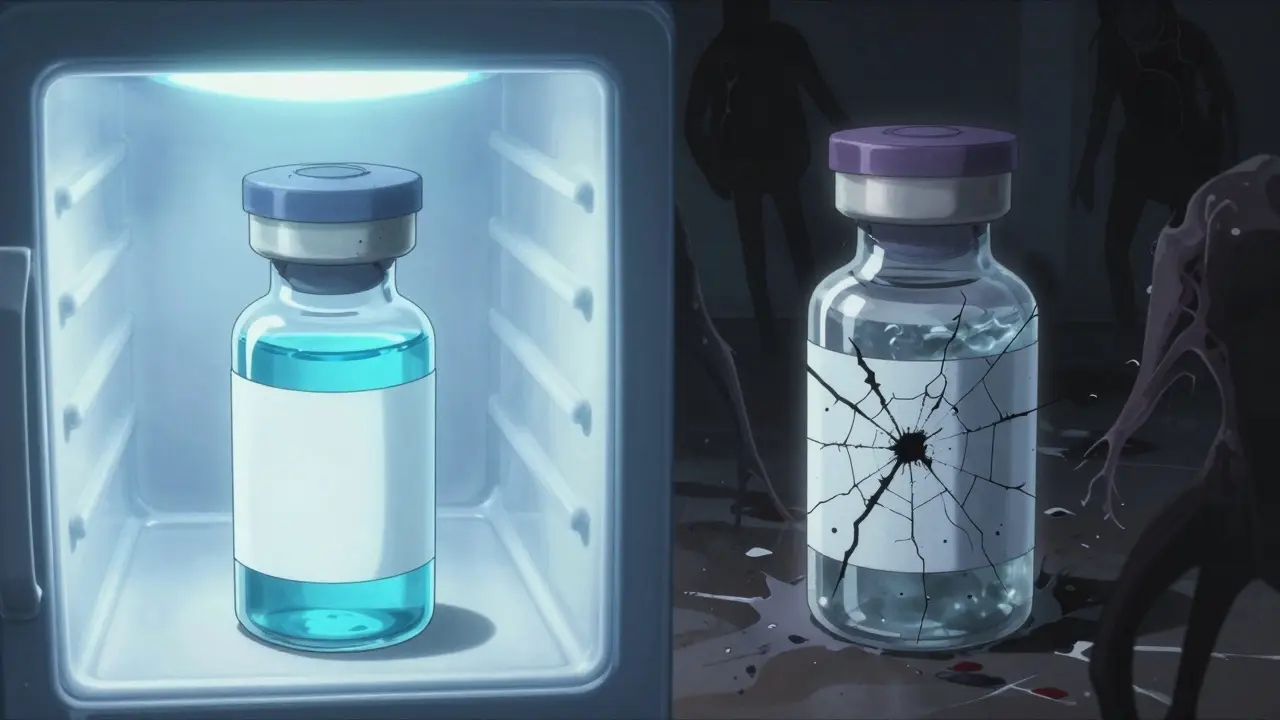
- Refrigerate when needed: Some drugs - insulin, certain antibiotics, eye drops, and vaccines - must be kept between 2°C and 8°C (36°F-46°F). Never freeze them unless the label says so. Freezing can destroy the structure of biologics and render them useless.
- Protect from light: Light-sensitive drugs like nitroglycerin, certain antibiotics, and thyroid meds degrade fast in sunlight. Keep them in their original amber bottles or wrap them in aluminum foil if you’ve transferred them.
- Don’t transfer to pill organizers: Unless they’re airtight and light-blocking, those plastic weekly containers expose meds to air and moisture. That’s why some people report their Xanax or levothyroxine losing effectiveness after a few weeks in a dispenser.
What Doesn’t Work - and What Could Be Dangerous
Some myths about storing medicine are dangerous. Don’t fall for them:- Freezing isn’t a magic fix: Freezing doesn’t extend shelf life for most drugs. It can damage injectables, liquids, and suspensions. Insulin that’s been frozen won’t work - even if it looks fine.
- Don’t store in cars or garages: Temperatures in parked cars can hit 60°C (140°F) in summer. That’s enough to melt capsules, break down active ingredients, and create harmful byproducts.
- Never use expired liquids or reconstituted drugs: Liquid antibiotics, eye drops, or insulin that’s been mixed (reconstituted) can grow bacteria or break down into toxic compounds. Tetracycline, for example, can degrade into a kidney toxin after expiration. These aren’t safe to use, even if they look clear.
- Don’t rely on smell or color: A pill might look fine but still be degraded. A liquid might not smell bad but could have lost potency. You can’t tell by sight or smell.
How the Government Extends Medicine Shelf Life - And What It Means for You
The FDA doesn’t just guess when to extend expiration dates. They use strict science. Stability testing follows ICH Q1A (R2) guidelines: drugs are tested over time under real-world conditions, plus higher heat and humidity, to predict how long they’ll last. The goal? Find the point where the drug’s potency drops below 90% - that’s the new expiration date. In 2024, the FDA extended the shelf life of TPOXX (tecovirimat) from 48 to 60 months for stockpiled doses. That’s a 25% increase. The Strategic National Stockpile now uses lot-specific tracking instead of printed dates, so each batch has its own timeline based on real data. This isn’t just for government stockpiles. The same science applies to your medicine. If you’ve stored your asthma inhaler or blood pressure pill properly, it’s likely still good. But unless you’re storing it in a climate-controlled lab, don’t assume it’s safe past the date.What You Can Do Right Now
You don’t need a lab to store your meds safely. Here’s a simple checklist:- Read the label. If it says "refrigerate," put it in the fridge - not the door, where temperatures swing.
- Keep all medicines in a cool, dry place - a bedroom drawer or closet works better than the bathroom.
- Use original packaging. Don’t dump pills into random containers.
- Check for changes. If a pill is cracked, discolored, or smells odd, throw it out.
- Don’t hoard. Buy only what you need. Expired meds clutter your medicine cabinet and create confusion.
- Ask your pharmacist. They know your meds and can tell you if yours are likely to last beyond the date.
What’s Changing in the Future
The pharmaceutical industry is moving away from fixed expiration dates. More companies are using real-time stability tracking. Some new packaging includes time-temperature indicators - little dots that change color if the drug was exposed to too much heat. This could let you know if your medicine is still good, even if the printed date has passed. By 2027, the global market for advanced packaging that extends shelf life will be worth over $150 billion. That’s because better storage = less waste = lower costs. But these technologies are still mostly for hospitals and stockpiles. For now, you’re on your own - and that’s why proper storage matters.When to Throw It Out
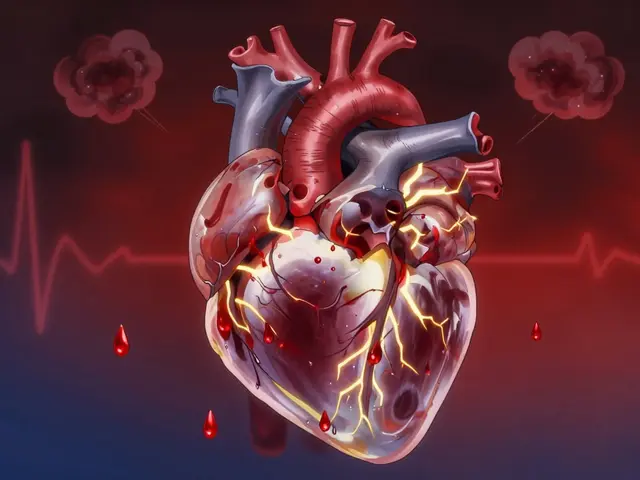
Some medicines are never safe to use after expiration:- Insulin (even if refrigerated)
- Reconstituted antibiotics (like amoxicillin suspension)
- Eyedrops and ear drops
- Nitroglycerin tablets (they lose potency fast)
- Any medicine that looks or smells wrong
Are expired medications dangerous to take?
Most expired medications aren’t dangerous - they just lose potency over time. The FDA and government studies show that 88% of properly stored drugs remain effective years past their expiration. However, certain drugs like insulin, liquid antibiotics, and tetracycline can break down into harmful substances. When in doubt, don’t take it.
Can I store medicine in the fridge to make it last longer?
Only if the label says so. Most pills don’t need refrigeration - and cold, damp air can actually damage them. Refrigeration helps only specific drugs like insulin, certain vaccines, and some liquid antibiotics. Storing other pills in the fridge can cause condensation, which leads to moisture damage and mold.
Is it safe to use medicine past its expiration date during an emergency?
Yes - if stored properly. During disasters or shortages, the FDA has approved using stockpiled drugs years beyond their labeled dates. For example, Tamiflu in federal reserves was cleared for use up to 10 years after manufacture. But this applies only to drugs that have been kept in controlled conditions. Don’t assume your home-stored pills are safe just because it’s an emergency.
Why do some drugs expire so quickly?
It’s not always about the drug itself - it’s about the formulation. Liquid medicines, suspensions, and reconstituted powders are more vulnerable to bacterial growth and chemical breakdown. Even the container matters. A pill in a sealed foil blister pack lasts longer than the same pill in a plastic bottle exposed to air. Manufacturers set conservative expiration dates to cover all possible storage conditions - not just ideal ones.
How can I tell if my medicine has gone bad?
Look for changes: pills that are cracked, discolored, or sticky; liquids that are cloudy, separated, or have particles; capsules that are soft or leaking. Smell matters too - a strong chemical odor or sour smell means degradation. If you’re unsure, don’t risk it. Take it to a pharmacy for disposal.
Final Thought: Storage Is More Important Than the Date
The expiration date on your medicine is just a starting point. What really determines if your drug still works is how you’ve kept it. A bottle of ibuprofen stored in a cool, dry drawer might be good for five years. The same bottle left on a sunny windowsill might be useless in six months. Your best tool isn’t a calendar - it’s common sense. Keep it cool, keep it dry, keep it in the original container, and ask your pharmacist when you’re not sure. You’ll save money, reduce waste, and keep your medicine working when you need it most.Write a comment
Items marked with * are required.




9 Comments
Dee Humprey January 4, 2026 AT 20:41
Just stored my insulin in the fridge door for months and didn’t realize it was ruining it. Thanks for the clear breakdown-this is the kind of info you wish you’d known sooner.
Stephen Craig January 4, 2026 AT 20:49
Expiration dates are social contracts, not scientific absolutes.
Justin Lowans January 5, 2026 AT 08:40
I never thought about light degradation until I read this. My old nitroglycerin was sitting on the bathroom counter for years-yikes. Now it’s wrapped in foil and tucked in a drawer. Small changes, big difference.
Clint Moser January 5, 2026 AT 14:39
the fda’s slep program is a classic case of gov’t overreach disguised as science-90% potency? who the hell defines potency? and why are we trusting corporate pharma’s lab conditions as gospel? i’ve seen pills degrade in sealed containers from humidity alone. this is all a controlled narrative to keep you buying new bottles. the real agenda? profit through planned obsolescence. also, i typo’d because i’m typing on a cracked screen. you’re welcome.
Michael Rudge January 6, 2026 AT 07:04
Oh wow. So we’re supposed to trust that some guy in a lab in 1998 stored your aspirin in a climate-controlled vault, and now you’re going to swallow it because it’s ‘probably fine’? How many people have died from this casual drug roulette? Your ‘common sense’ is just negligence with a thesaurus.
Jack Wernet January 6, 2026 AT 08:00
In my village in rural Ohio, we’ve been keeping meds in a metal box under the bed since the 70s. Never had an issue. Culture shapes how we care for things-sometimes better than manuals.
bob bob January 7, 2026 AT 12:18
My grandma used to keep all her pills in a tin inside a sock drawer. She’s 92 and still walking. Maybe the real secret is just not stressing about it?
mark etang January 9, 2026 AT 07:34
It is imperative to underscore the significance of adherence to manufacturer-specified storage protocols. Deviations, even minor, introduce unacceptable variability into pharmacokinetic integrity. One must treat pharmaceuticals with the same rigor as one would treat calibrated scientific instrumentation. Compromised storage conditions constitute a breach of therapeutic fidelity.
Roshan Aryal January 9, 2026 AT 12:03
USA thinks it’s the only country that knows how to store pills. In India, we keep everything in dry clay pots. No fridge, no foil, no FDA. Pills last 10 years. Your ‘science’ is just overengineering. We don’t need your $150 billion packaging. We need less arrogance.