Health October 17, 2025
Blood Clots in Stents: What to Expect During Recovery & Rehabilitation
Recovery Timeline Estimator
Next Phase to Expect
Key Actions
If you've had a coronary stent placed, the phrase blood clots in stents might sound scary. The good news is that with the right care, most people bounce back fully. Below you’ll find a straight‑forward guide that walks you through what actually happens after a clot forms, how doctors treat it, and what you can do at home to speed up healing.
Key Takeaways
- Blood clots can form inside a stent-watch for chest pain, shortness of breath, or unusual fatigue.
- Immediate treatment typically involves antiplatelet drugs and sometimes a repeat angiography.
- Recovery follows a predictable timeline: 1‑2 weeks for basic healing, 4‑6 weeks for full activity, 3‑6 months for cardiac rehab.
- Stick to prescribed medication, especially dual antiplatelet therapy, to keep the stent open.
- Lifestyle tweaks - quit smoking, adopt a heart‑healthy diet, and stay active - dramatically lower the risk of another clot.
Understanding Blood Clots in Stents
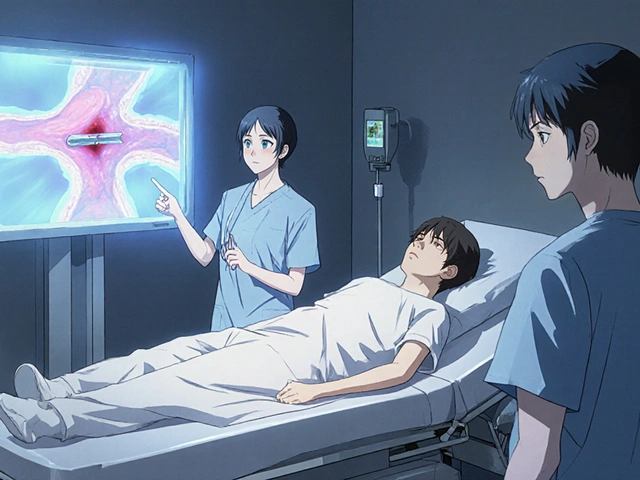
When a blood clot in a stent forms after a percutaneous coronary intervention (PCI), it can partially or completely block blood flow, the heart muscle may not get enough oxygen. This situation is medically called stent thrombosis and is considered an emergency because it can trigger a heart attack.
A stent is a tiny metal mesh tube that props open a narrowed coronary artery after PCI. While stents are lifesaving, the body sometimes reacts by forming a clot on the metal surface, especially if medication adherence slips.
Symptoms&When to Call Your Doctor
Spotting a problem early can save heart muscle. Typical warning signs include:
- Sudden, crushing chest pain that doesn’t improve with rest.
- Shortness of breath or a feeling of “tightness” in the chest.
- Unexplained fatigue, light‑headedness, or sweating.
- New‑onset arrhythmia detected on a home monitor.
If any of these appear, call emergency services right away. Early intervention dramatically improves outcomes.
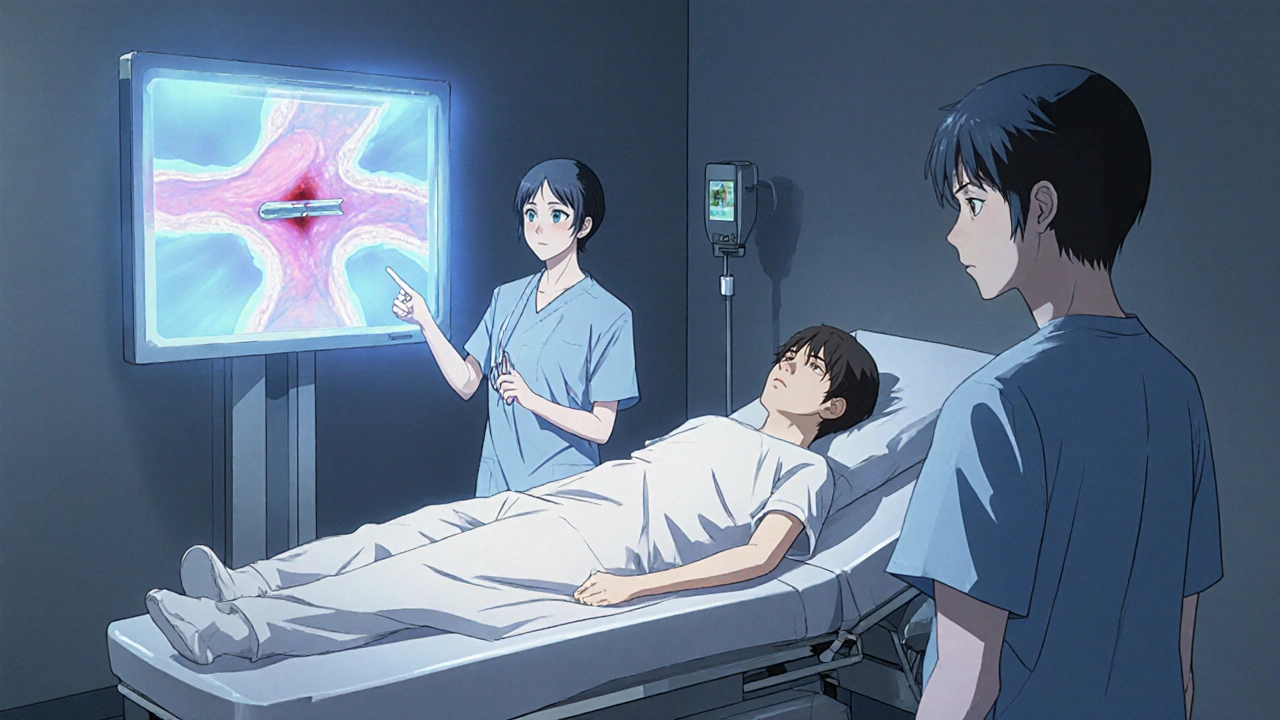
Immediate Medical Management
In the hospital, doctors usually follow a protocol:
- Confirm clot presence with an angiography X‑ray imaging of the coronary arteries after injecting contrast dye.
- Administer a high‑dose antiplatelet therapy medication that prevents platelets from clumping together, often a fast‑acting intravenous agent.
- If the clot is large, perform a repeat PCI-balloon inflation or a new stent may be needed.
- Start or intensify dual antiplatelet therapy (DAPT) a regimen that typically combines aspirin with a P2Y12 inhibitor such as clopidogrel for at least 6-12 months.
Most patients leave the cath lab within a day, but the real work begins at home.
Recovery Timeline
| Time Frame | What to Expect | Key Actions |
|---|---|---|
| Days 1‑3 | Hospital monitoring; pain may improve. | Take prescribed DAPT exactly as directed; limit physical strain. |
| Weeks 1‑2 | Gradual return to light activity (short walks). | Schedule follow‑up appointment; begin gentle stretching. |
| Weeks 3‑6 | Participate in supervised cardiac rehabilitation structured exercise and education program for heart patients. | Track heart rate during exercise; maintain medication schedule. |
| Months 3‑6 | Full clearance for moderate‑intensity activities (jogging, swimming). | Continue DAPT until doctor advises stopping; adopt long‑term lifestyle changes. |
| Beyond 6months | Stable cardiovascular health, low re‑thrombosis risk. | Annual check‑ups; keep heart‑healthy diet and exercise routine. |
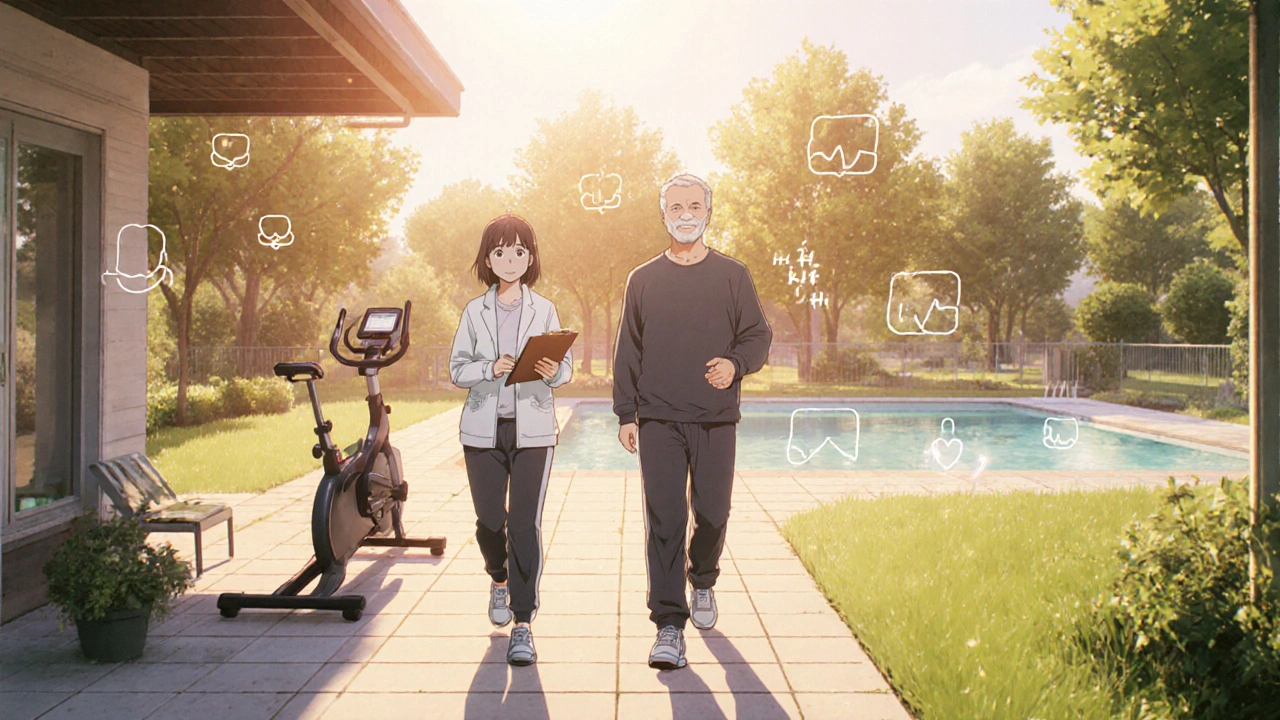
Rehabilitation Exercises
Exercise is a cornerstone of recovery, but it must be progressive. Here’s a simple 4‑stage plan you can discuss with your rehab specialist:
- Phase1 (Weeks1‑2): Light walking 5‑10minutes, 2‑3 times per day. Goal: keep circulation moving without raising heart rate above 50% of your predicted maximum.
- Phase2 (Weeks3‑4): Add seated marching or gentle stationary‑bike for 10‑15minutes. Monitor for any chest discomfort.
- Phase3 (Weeks5‑6): Start low‑impact aerobic classes (water aerobics, rec‑room cycling). Aim for 20‑30minutes, 3times per week.
- Phase4 (Month3+): Incorporate moderate‑intensity activities like brisk walking, jogging, or swimming. Maintain a heart‑rate target of 60‑70% of maximum.
Always warm‑up for 5minutes and cool‑down for 5minutes. If you notice new chest pain, shortness of breath, or dizziness, stop and call your cardiologist.
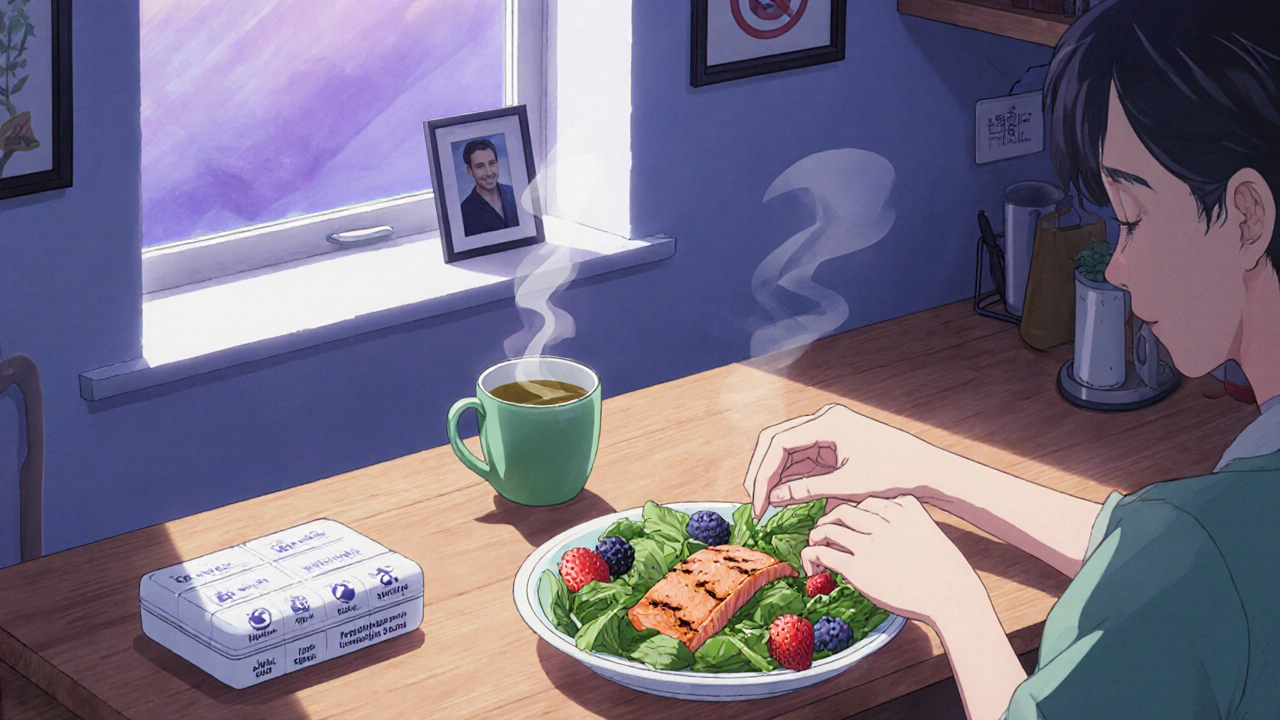
Lifestyle Adjustments that Lower Re‑Clot Risk
Medication adherence is non‑negotiable, but habits outside the pillbox count just as much:
- Quit smoking: Nicotine speeds platelet activation. Use nicotine‑replacement therapy or prescription meds if needed.
- Heart‑healthy diet: Emphasize leafy greens, berries, whole grains, oily fish, and limit saturated fats and processed sugars.
- Control blood lipids: A statin medication lowers LDL cholesterol and stabilizes arterial plaque is usually prescribed after PCI.
- Manage blood pressure: Target < 130/80mmHg, using lifestyle changes and antihypertensives if required.
- Stay hydrated: Dehydration can thicken blood, increasing clot risk.
- Regular check‑ups: Blood tests to verify platelet inhibition levels and cholesterol control.
Follow‑up Care & Monitoring
Typical follow‑up schedule looks like this:
- 2‑week post‑procedure visit: review DAPT tolerance, ECG, basic labs.
- 6‑week visit: stress test or coronary CT to confirm stent patency.
- 3‑month visit: adjust medication dosage, discuss rehab progress.
- 6‑month and yearly visits: long‑term lipid panel, blood pressure, and symptom review.
Some physicians order a repeat angiography to visually confirm no new clot formation if symptoms recur or if the patient had a high‑risk clot initially.
Common Pitfalls and How to Avoid Them
Even with the best plan, people slip up. Here are the most frequent mistakes and quick fixes:
- Skipping doses: Set alarms or use a pill‑box. Missing even one dose of DAPT can double clot risk.
- Returning to intense exercise too early: Follow the phased rehab schedule; talk to your physiotherapist before upping intensity.
- Ignoring mild chest discomfort: Report any new sensation, even if it feels “just a little”.
- Underestimating diet impact: Keep a food diary for the first 2months to identify hidden saturated fats.
- Delaying follow‑up appointments: Schedule them before you leave the hospital; add them to your calendar.
What’s Next?
Recovering from a clot in a stent is a team effort - you, your cardiologist, rehab specialists, and your support network. By staying on medication, moving responsibly, and keeping lifestyle choices heart‑friendly, you give yourself the best shot at a full, symptom‑free life.
Frequently Asked Questions
Can a blood clot in a stent happen months after the procedure?
Yes. Late stent thrombosis can occur up to a year later, especially if DAPT is stopped early or if the patient smokes.
Is dual antiplatelet therapy necessary for everyone?
Most guidelines recommend DAPT for at least 6months after a drug‑eluting stent, and longer if a clot has already formed.
What are the signs that a clot is forming again?
Sudden chest pressure, shortness of breath, sweating, or unexplained fatigue should trigger an emergency call.
Can I exercise at home before starting formal cardiac rehab?
Light walking or seated marching is safe after the first week, but avoid high‑intensity or heavy lifting until cleared by your cardiologist.
Do I need to continue statins forever?
Most experts recommend lifelong statin therapy after a stent, because it stabilises plaque and lowers re‑clot risk.
Is it safe to travel by plane during recovery?
Generally yes after the first two weeks, but stay hydrated, move your legs regularly, and keep medication on hand.
Write a comment
Items marked with * are required.




9 Comments
Grace Hada October 17, 2025 AT 21:10
Clot anxiety is a mental cage-break free with disciplined meds and movement.
nitish sharma October 18, 2025 AT 13:50
It is understandable to feel uneasy after a stent thrombosis, yet adherence to dual antiplatelet therapy remains paramount. By maintaining strict medication schedules, you significantly reduce the risk of recurrent events. Moreover, gradual re‑introduction of activity, as outlined in the recovery timeline, supports cardiovascular remodeling. Let us stay focused on these evidence‑based steps to ensure optimal healing.
Rohit Sridhar October 19, 2025 AT 06:30
Recovering from a clot in a stent can feel like climbing a steep mountain, but each step you take is a victory worth celebrating. First, remember that the medications you’re prescribed are not just pills; they are the scaffolding that keeps your artery open and your heart nourished. The first few days may be uncomfortable, but light walking for 5‑10 minutes a few times daily gently nudges blood flow without overtaxing the heart. As you move into weeks two and three, incorporate seated marching or a low‑resistance stationary bike; these activities keep circulation robust while allowing your heart to adapt.
By week five, you’ll likely feel more confident, and it’s an excellent time to join a supervised cardiac rehabilitation program. These programs not only provide safe aerobic exercise but also educate you on nutrition, stress management, and medication adherence. The knowledge you gain there reinforces the habits that keep clots at bay.
Nutrition plays a silent yet powerful role. Prioritize leafy greens, berries, whole grains, and oily fish; these foods combat inflammation and support vascular health. Simultaneously, eliminate processed sugars and saturated fats that can destabilize plaque. Hydration should not be overlooked-adequate fluid intake prevents blood from thickening, a subtle but crucial factor in clot prevention.
While you’re making progress, never underestimate the importance of regular follow‑up appointments. Blood tests that monitor platelet inhibition levels and lipid panels are essential checkpoints. If any new chest discomfort or unusual fatigue arises, treat it as a warning sign and contact your cardiologist immediately.
Finally, nurture your mental well‑being. Stress can elevate catecholamines, which in turn may increase platelet activity. Practices like mindfulness, gentle yoga, or simply spending time with loved ones can offset this effect.
In sum, your recovery is a coordinated effort of medication, graded exercise, heart‑healthy nutrition, vigilant monitoring, and emotional balance. Stay patient, stay disciplined, and you’ll emerge stronger on the other side of this challenge.
Sarah Hanson October 19, 2025 AT 23:10
Great summary, but make sure you double‑check the dosage timings-missed doses can double the risk. Also, keep a visible pill‑box; it helps a lot.
Nhasala Joshi October 20, 2025 AT 15:50
🚨⚠️Listen up: the pharma giants don’t want you to know that staying hydrated & eating greens actually *lowers* their profit margins! They push statins & pricey meds while the *real* cure is in nature 🌿💊. Don’t be a pawn, read the fine print and demand transparent studies! 😱💥
kendra mukhia October 21, 2025 AT 08:30
Honestly, if you’re still debating whether to quit smoking, you’re missing the point completely. The data is crystal clear: every cigarette pushes you closer to another clot. Stop the drama, quit now, and follow the rehab plan like it’s a lifeline.
Bethany Torkelson October 22, 2025 AT 01:10
Enough with the excuses! You’ve got the meds, the schedule, the guidance-just act on it. No more whining, just commitment.
alex montana October 22, 2025 AT 17:50
Wow!!! you really think this is just a simple thing??! i mean, sure, follow the plan---but also, listen to your body...or dont??
Wyatt Schwindt October 23, 2025 AT 10:30
Stick to the medication schedule and keep your activity level gradual.