Health February 20, 2026
Hypoparathyroidism: How to Manage Low Calcium and Vitamin D Effectively
When your body doesn’t make enough parathyroid hormone (PTH), your blood calcium drops-and that’s not just a lab number. It’s tingling fingers, muscle cramps, fatigue, and sometimes seizures. Hypoparathyroidism is rare, but for those living with it, daily life revolves around pills, blood tests, and constant balancing acts. Most cases happen after thyroid or neck surgery, but it can also come from genetics, autoimmunity, or radiation. The goal isn’t just to raise calcium. It’s to keep it just high enough to feel normal, but not so high that you damage your kidneys or heart. And it’s harder than most people realize.
Why Calcium and Vitamin D Alone Aren’t Enough
You might think, ‘Just take calcium and vitamin D, and you’re good.’ But hypoparathyroidism isn’t like osteoporosis. Here, your body can’t turn vitamin D into its active form because PTH is missing. That’s why regular vitamin D3 (cholecalciferol) often fails. Instead, you need active vitamin D analogues like calcitriol or alfacalcidol. These bypass the broken step in your body’s system and work directly. Studies show calcitriol brings calcium levels up 2.3 times faster than regular vitamin D. Without it, you’re stuck with symptoms no matter how many pills you swallow.
Calcium supplements are just as critical. But not all forms are equal. Calcium carbonate is the go-to because it’s 40% elemental calcium-meaning a 1,250 mg tablet gives you 500 mg of usable calcium. Calcium citrate? Only 21%. So you’d need nearly twice as many pills to get the same amount. Most patients take 1,000 to 2,000 mg of elemental calcium daily, split into two or three doses, always with meals. Why? Food helps absorption, and it also acts as a phosphate binder, which matters because phosphate levels tend to spike when PTH is low.
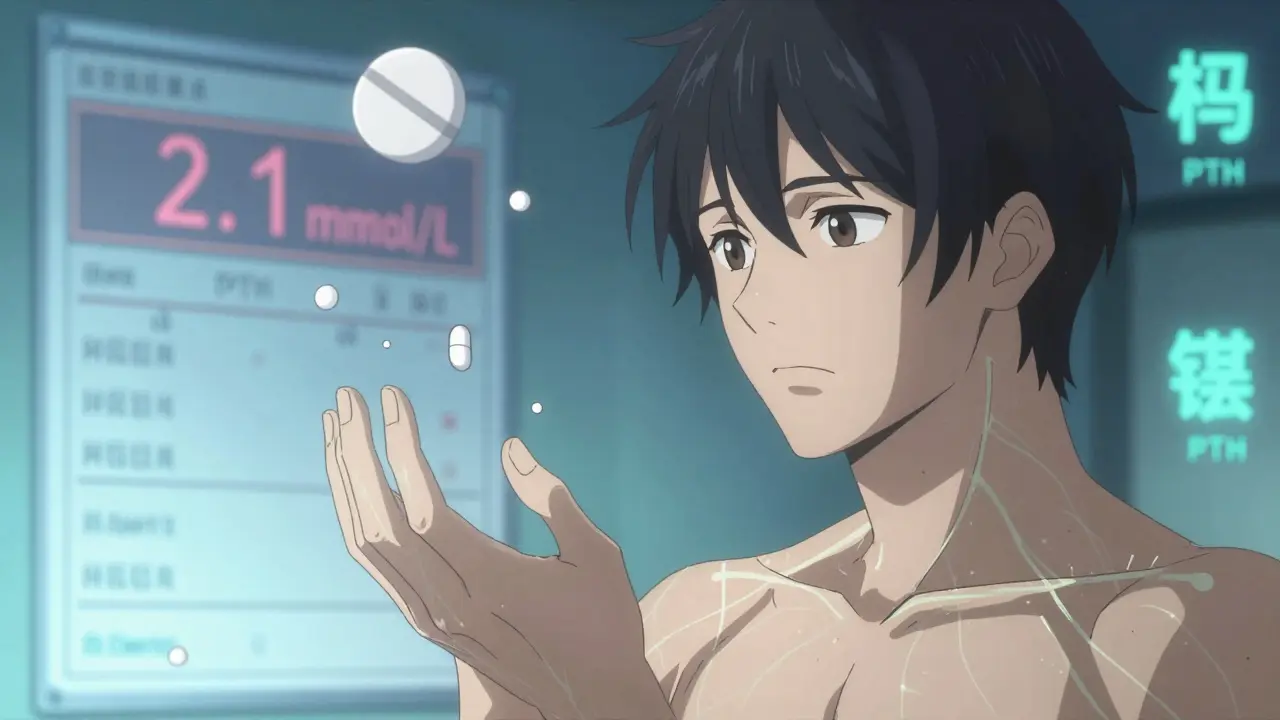
What Your Blood Numbers Should Look Like
Target ranges aren’t one-size-fits-all. The goal isn’t to hit the middle of the normal range. It’s to stay in the lower half: 2.00 to 2.25 mmol/L (8.0 to 8.5 mg/dL). Why? Because pushing calcium higher increases the risk of kidney stones, calcification in your brain, and hardened arteries. The Hypopara Registry found that 30-40% of patients struggle to hit this target. Too low? You get numbness and cramps. Too high? You risk long-term organ damage.
Here’s what else to watch:
- Urinary calcium: Keep it under 250 mg per day. Over this, and your kidneys are at risk. A 24-hour urine test is required before any dose increase.
- Phosphate: Aim for 2.5 to 4.5 mg/dL. High phosphate worsens symptoms and makes calcium harder to control.
- Magnesium: Below 1.7 mg/dL? You need supplementation. Low magnesium stops PTH from working-even if you’re taking the right drugs.
- Vitamin D3 (25-OH-D): Maintain 20-30 ng/mL. This isn’t your active form, but it’s a backup. Too low, and your body can’t respond well.
How to Avoid the ‘Calcium Rollercoaster’
One of the biggest complaints from patients? The ‘calcium rollercoaster.’ One day you feel fine. The next, your hands are tingling. Why? Inconsistent dosing. Taking all your calcium in two big doses? That’s a recipe for spikes and crashes. Experts now recommend splitting it into four or five smaller doses throughout the day. Parathyroid UK’s patient data shows this reduces symptoms by up to 40%. Take calcium with each meal and a snack. Set phone alarms. Write it on your fridge. Stability comes from routine, not quantity.
Also, timing matters. Take active vitamin D at bedtime. It absorbs better when your stomach is empty, and it helps avoid nighttime muscle cramps. Magnesium? Take it with calcium if you’re using citrate, or separately if you’re on oxide. Don’t mix them if they cause stomach upset.
When High Doses Don’t Work-And What to Do Next
Some people just can’t get stable, no matter how many pills they take. If you need more than 2 grams of calcium daily or over 2 micrograms of calcitriol, you’re in the 25-30% of patients who don’t respond well to conventional therapy. That’s not your fault. It’s the limitation of the treatment.
Here’s what your doctor might suggest:
- Thiazide diuretics: Hydrochlorothiazide 12.5-25 mg daily helps your kidneys reabsorb calcium, reducing urine loss. It’s cheap, effective, and often overlooked.
- Sodium restriction: Cut salt to under 2,000 mg per day. High sodium makes your kidneys dump more calcium.
- PTH replacement: Drugs like Natpara (PTH 1-84) or teriparatide (Forteo) mimic natural hormone action. They can cut calcium and vitamin D needs by 30-40%. But they’re expensive-around $15,000 a month-and require daily injections. They’re also not first-line. You need to fail conventional therapy first.
There’s new hope on the horizon. TransCon PTH, a once-daily long-acting injection, showed 89% of patients normalized calcium in a 2022 trial. It’s not approved everywhere yet, but it’s coming. For now, it’s still an option for those who can’t manage with pills.
Diet: What to Eat-and What to Avoid
Food isn’t just fuel. It’s part of your treatment. You need calcium-rich foods: dairy (300 mg per serving), kale (100 mg per cup), broccoli (43 mg per cup), and fortified plant milks. But you also need to avoid phosphate traps.
Phosphate lurks in:
- Colas and sodas (500 mg per liter)
- Processed meats (150-300 mg per serving)
- Hard cheeses (500 mg per ounce)
- Instant soups and packaged snacks
Try to keep daily phosphate under 1,000 mg. That means reading labels. Skip the soda. Choose fresh chicken over deli meat. Use herbs instead of salt. It’s not about perfection-it’s about reducing the burden on your body.

What Most Doctors Don’t Tell You
A 2021 survey found 78% of family doctors feel unprepared to manage hypoparathyroidism. That means you might be the expert on your own condition. Keep a log: calcium doses, symptoms, urine output. Bring it to every appointment. Ask for a 24-hour urine test before any dose change. Push for magnesium checks if you’re tired or crampy. And don’t accept ‘it’s just how it is.’
Emergency plan? If you feel numbness, tingling, or a muscle spasm, chew 2-3 calcium tablets (500-1,000 mg total) right away. Keep them in your bag, your car, your desk. This isn’t a drill. It’s your safety net.
The Long Game: Protecting Your Kidneys and Brain
This isn’t a short-term fix. Hypoparathyroidism is lifelong. And over time, even well-managed cases carry risks. Studies show 15-20% of patients develop early kidney disease after 10 years. Brain calcification? That’s 2.8 times more likely if your calcium stays above 2.35 mmol/L for years. That’s why the lower target matters. You’re not just treating symptoms. You’re protecting your future.
Regular monitoring is non-negotiable. In the first 3 months, expect visits every 4-6 weeks. Once stable, 3-4 times a year is enough. But if you’re on PTH therapy or have kidney issues, you’ll need more frequent checks.
What Works for One Person Might Not Work for You
There’s no single ‘right’ way. Some do great on low-dose calcium and vitamin D. Others need injections. Some manage with diet. Others need diuretics. The key is personalization. Track what works. Talk to others. Join a community like the Hypopara Alliance. You’re not alone-and your experience can help shape better care for others.
Can I just take more calcium if I feel symptoms?
No. Taking extra calcium without checking your urine levels can lead to kidney stones or calcification in soft tissues. Always test your 24-hour urinary calcium before increasing doses. If you’re having symptoms, chew 2-3 calcium tablets immediately, but contact your doctor within 24 hours to adjust your long-term plan.
Why is my vitamin D3 not working?
Vitamin D3 (cholecalciferol) needs PTH to become active in your kidneys. With hypoparathyroidism, that step is broken. That’s why you need active forms like calcitriol or alfacalcidol-they skip the missing step and work directly. Taking more D3 won’t help. You need the right form.
Is magnesium really that important?
Yes. Low magnesium stops PTH from being released and makes cells resistant to it-even if you’re on replacement therapy. If your magnesium is below 1.7 mg/dL, you’ll still have symptoms. Supplement with magnesium oxide or citrate (400-800 mg daily) and retest in 4-6 weeks.
Can I stop taking these meds someday?
In most cases, no. Hypoparathyroidism is usually permanent, especially after surgery or due to genetics. Rare exceptions exist-like temporary cases after neck surgery where the glands recover. But even then, doctors monitor for 6-12 months before considering stopping. Never stop without medical supervision.
What’s the biggest mistake people make?
Taking all calcium in one or two doses. That causes spikes and crashes, leading to symptoms and poor control. Splitting doses into 4-5 smaller ones, taken with meals, is far more effective. Also, skipping urine tests. You can’t adjust safely without knowing how much calcium your kidneys are losing.