Health December 27, 2025
Opioid Reactions: How to Tell Itching from a Real Allergy and What to Do
Itching from opioids isn’t always an allergy - and mistaking it for one can limit your pain relief
If you’ve ever felt itchy after taking morphine or oxycodone, you’re not alone. Most people assume it’s an allergy. You might have even been told to avoid all opioids because of it. But here’s the truth: itching from opioids is rarely a true allergy. In fact, up to 80% of people who say they’re allergic to opioids are actually experiencing a side effect - not an immune reaction. This misunderstanding leads to unnecessary pain, higher costs, and fewer treatment options.
True opioid allergies are rare. They involve your immune system reacting to the drug, causing symptoms like hives, swelling of the throat, trouble breathing, or a sudden drop in blood pressure. These reactions can be life-threatening. But itching alone? That’s usually something else entirely.
What’s really happening when you itch after an opioid?
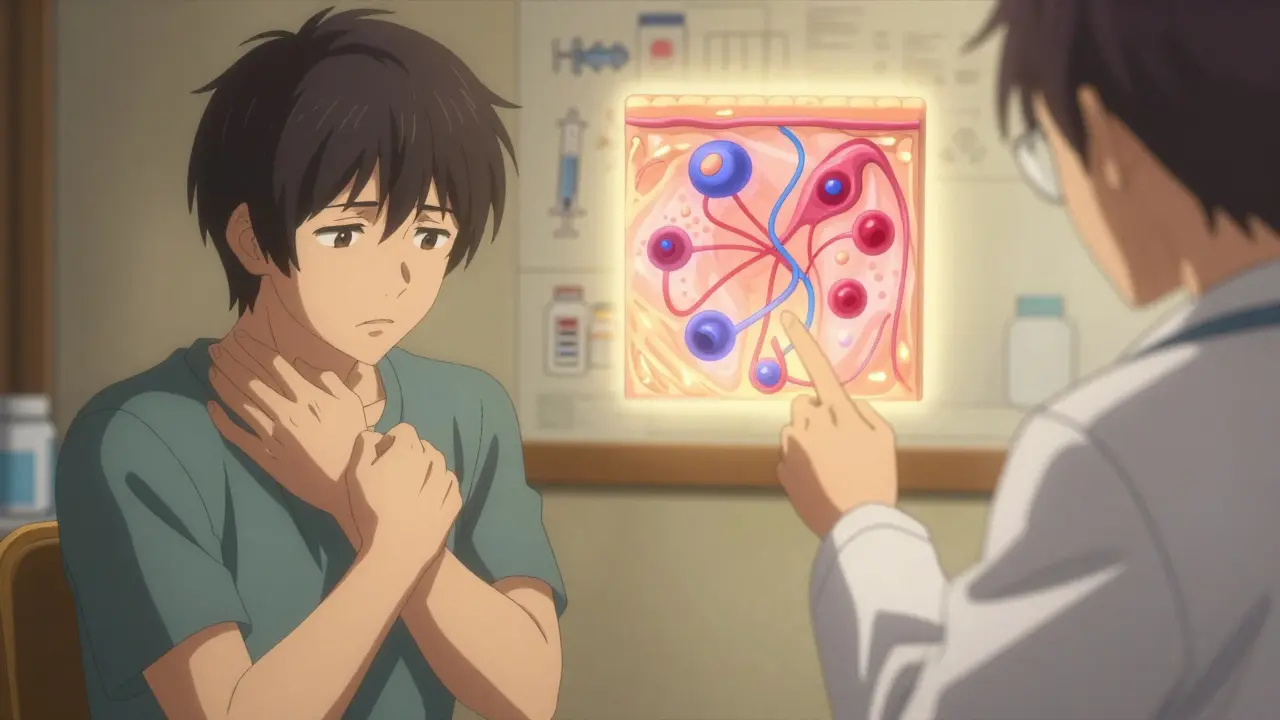
When you get itchy after taking morphine, codeine, or hydromorphone, it’s most likely a pseudoallergic reaction. This means your body isn’t attacking the drug like it would with pollen or peanuts. Instead, the opioid directly triggers mast cells in your skin to release histamine - the same chemical that makes you sneeze during allergy season. No immune system involvement. No memory. No future risk beyond this dose.
This is why the itching often gets worse with higher doses or faster IV pushes. It’s not your body saying “I’m allergic.” It’s the drug saying “I’m triggering histamine release.” Morphine, for example, releases 3 to 4 times more histamine than an equivalent dose of hydromorphone. That’s why one person might itch badly on morphine but feel fine on fentanyl.
Even weirder? Some itching comes from a completely different pathway - one that has nothing to do with histamine. Researchers found that opioids activate special receptors in your spinal cord called GRPR (gastrin-releasing peptide receptors). These receptors are wired to make you itch, even if your skin is perfectly normal. That’s why antihistamines like Benadryl don’t always help.
How to tell if it’s a real allergy or just a side effect
Here’s how to spot the difference:
- Pseudoallergic reaction (common): Itching alone, flushing, mild sweating, nausea, or dizziness. Symptoms start within minutes of taking the drug and get worse with higher doses. They usually go away when you stop or reduce the dose.
- True allergy (rare): Hives, swelling of lips/tongue/throat, wheezing, low blood pressure, or a rash that spreads and blisters. These happen fast - often within 5 to 30 minutes - and can get worse with each exposure. If you’ve ever passed out or needed epinephrine after an opioid, that’s a true allergy.
Doctors use a simple tool called the Opioid Allergy Assessment Tool to tell them apart. It asks: Did the itching happen right after the dose? Did it get worse with more drug? Did antihistamines help? If the answer is yes to all three, it’s almost certainly a pseudoallergy.

What to do if you itch after an opioid
Don’t panic. Don’t refuse all opioids. Here’s what actually works:
- Try a lower dose. Cut the opioid amount by 25-50%. Often, the itching disappears at lower doses because there’s not enough drug to trigger histamine release.
- Take an antihistamine before the opioid. Diphenhydramine (Benadryl) 25-50 mg orally or IV 30 minutes before the dose helps in 85% of cases. It doesn’t fix everything, but it makes a big difference.
- Switch opioids. Not all opioids are the same. Morphine and codeine? High itch risk. Fentanyl, methadone, or hydromorphone? Much lower. Fentanyl is 100 times stronger than morphine but causes 3-4 times less itching. Methadone causes itching in only 5-10% of users, compared to 30-40% for morphine.
- Consider newer options. Nalfurafine (approved in Japan, in U.S. trials) targets the spinal itch pathway directly and reduces opioid-induced itching by 70% without dulling pain. It’s not widely available yet, but it’s coming.
One patient told me, “I was told I was allergic to all opioids because I got itchy on morphine. Then I tried a fentanyl patch with Benadryl - no itching, no problem.” That’s the story of 87% of people labeled allergic to opioids - they’re not allergic at all.
Why mislabeling opioid “allergies” is dangerous
When you’re labeled “allergic to opioids,” your doctors avoid them - even if you’re in severe pain. That means you might get weaker painkillers, more nerve blocks, or even be sent home untreated. Studies show patients with fake opioid allergy labels get less effective pain control, longer hospital stays, and higher rates of depression.
And it’s expensive. Mislabeling costs the U.S. healthcare system about $1,200 per patient because they use more costly alternatives like non-opioid drugs, nerve stimulators, or repeated ER visits. Multiply that by 20-30 million people annually who report opioid “allergies,” and you’re looking at $24-36 billion wasted every year.
Worse, some patients avoid opioids entirely - even when they’re the best option for cancer pain or post-surgery recovery. That’s not safety. That’s suffering.
When you really need to avoid opioids
There are times when avoiding opioids is the right call. If you’ve had:
- Hives or swelling after any opioid
- Difficulty breathing or a sudden drop in blood pressure
- A rash that blistered or peeled
Then you likely have a true allergy. Avoid that specific opioid and any chemically similar ones (like oxycodone or hydrocodone). But even then, you may still be able to take fentanyl or methadone - they’re structurally different and rarely cross-react.
Desensitization is an option for people who truly need an opioid but have a confirmed allergy. Under close supervision, doctors can slowly introduce tiny doses over several hours. Success rates are over 95%. It’s not common, but it’s life-changing for cancer patients or those with chronic pain who have no other options.
What you should tell your doctor
Don’t just say, “I’m allergic to opioids.” Say this instead:
- “I got itchy after morphine, but I didn’t break out in hives or have trouble breathing.”
- “I took Benadryl and the itching got better.”
- “I’ve tried fentanyl before and it didn’t cause itching.”
Give your doctor the full picture. Bring up the dose, timing, and what helped. Most doctors don’t know the difference - so educate them gently. You’re not being difficult. You’re helping them give you better care.
The future: Better tools, fewer misdiagnoses
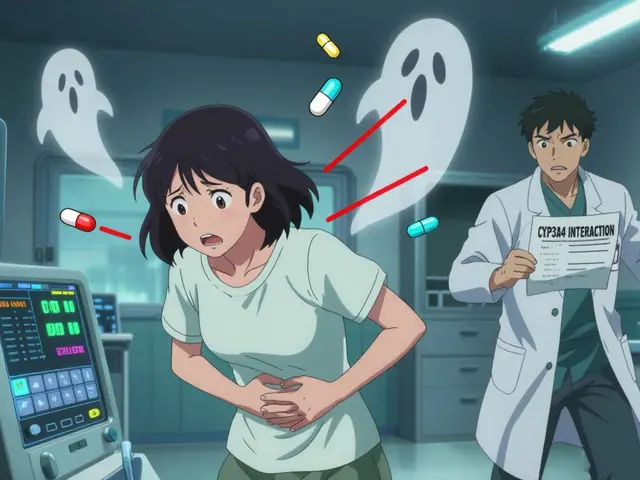
Hospitals are starting to fix this. Epic’s electronic health records now flag whether a reaction was “itching” or “anaphylaxis” - and automatically suggest safer alternatives. In one study, this cut false allergy labels by 45%.
Research is moving fast. Scientists are developing a simple blood test that can spot mast cell activation in minutes - no skin prick needed. Genetic tests might soon tell you if you’re prone to histamine release based on your DNA. And new drugs like CR845 (korsuva) are showing 80% reduction in itching without affecting pain relief.
But the biggest change won’t come from a test or a new drug. It’ll come from doctors learning to ask the right questions. “Did you get itchy? Or did you swell up?” That one question saves millions from unnecessary pain.
Bottom line
Itching from opioids is common. It’s not dangerous. It’s not an allergy. You can still get strong pain relief - you just need the right drug and the right approach. Don’t let a simple side effect rob you of effective treatment. Talk to your doctor. Ask about alternatives. Try a lower dose with antihistamines. You don’t have to suffer - and you don’t have to avoid opioids forever.
Is opioid itching a sign of a real allergy?
No, opioid itching is rarely a true allergy. In fact, 70-80% of people who say they’re allergic to opioids are actually experiencing a pseudoallergic reaction - a direct histamine release from mast cells, not an immune response. True allergies involve swelling, trouble breathing, or hives, not just itching.
Can I still take opioids if I get itchy?
Yes. Many people who itch on morphine can safely take fentanyl, methadone, or hydromorphone with a lower dose and an antihistamine like diphenhydramine. Switching opioid types often eliminates the itching without losing pain control.
What’s the best way to treat opioid-induced itching?
Start by lowering the opioid dose by 25-50%. Then take diphenhydramine (Benadryl) 25-50 mg 30 minutes before the next dose. If that doesn’t help, switch to an opioid with lower histamine-releasing potential - like fentanyl or methadone. Avoid antihistamines alone if the itching is severe or persistent; it might be from a different spinal pathway.
Which opioids cause the most itching?
Morphine and codeine cause the most itching - up to 30-40% of users. Hydromorphone is less likely, and fentanyl and methadone cause itching in only 5-10% of people. This is because morphine and codeine have chemical structures that trigger mast cells more easily.
Should I get skin tested for opioid allergies?
Usually not. Skin tests for opioids are unreliable and often give false positives. Unless you had a severe reaction like anaphylaxis, doctors recommend a therapeutic trial with a different opioid instead. Testing is only considered in rare cases where a true allergy is strongly suspected.
Can opioid itching be dangerous?
The itching itself isn’t dangerous. But if you stop taking needed pain medication because you think you’re allergic, that can be harmful. Chronic pain leads to depression, sleep loss, and reduced mobility. Mislabeling an opioid as “allergic” can do more harm than the itching ever could.
Write a comment
Items marked with * are required.




10 Comments
Celia McTighe December 28, 2025 AT 10:09
This is such a needed post! 🙌 I had no idea itching wasn't always an allergy. My grandma was denied morphine after hip surgery because of a "reaction"-turns out she just got itchy. She cried because she was in so much pain. Thank you for explaining this so clearly.
Sydney Lee December 29, 2025 AT 16:42
The fact that clinicians still conflate pseudoallergic histamine release with true IgE-mediated anaphylaxis is not merely negligent-it is a systemic failure of medical education. One must question the competency of any provider who cannot distinguish between mast cell degranulation and immune sensitization. The consequences are not anecdotal; they are catastrophic.
oluwarotimi w alaka December 30, 2025 AT 05:35
lol so now even pain meds are part of the westen medical conspiracy? they just want you to take more drugs so pharma can get rich. i heard in nigeria they use herbal mix and no one gets itchy. why? because they dont trust the white man's medicine.
Debra Cagwin January 1, 2026 AT 03:20
Thank you for writing this with so much care. I’ve seen too many patients shut down from pain treatment because of a label they didn’t understand. You’re right-this isn’t about being difficult, it’s about being informed. If you’re reading this and you’ve been told you’re "allergic" to opioids, please don’t give up. Talk to your doctor. Bring this article. You deserve relief.
Hakim Bachiri January 1, 2026 AT 14:53
Okay so let me get this straight-morphine is basically a histamine bomb, but fentanyl? Chill. Methadone? Chill. But we still use morphine because it's cheap? And we're surprised people get itchy? This is why American healthcare is a dumpster fire. We optimize for cost, not comfort. And then we blame the patient for "overreacting."
Ellen-Cathryn Nash January 2, 2026 AT 22:09
I got itchy on oxycodone once. Didn’t think twice. Just said, "Ew, nope." Now I’m stuck with gabapentin and NSAIDs that make my stomach feel like it’s been marinated in vinegar. I didn’t know I could’ve just switched. I feel so dumb. And also, kinda angry.
Ryan Touhill January 3, 2026 AT 04:17
It’s fascinating how the medical community clings to outdated terminology. "Allergy" is a loaded word-emotional, fearful, final. We need a new clinical term: "opioid-induced histaminergic response." It’s accurate. It’s precise. It removes stigma. And yet, we persist with lazy language because it’s easier than retraining 2 million clinicians. The system is designed to fail us.
Samantha Hobbs January 4, 2026 AT 20:29
I used to get itchy as heck on morphine. I just took Benadryl before and it was fine. Why is this even a thing? Like… it’s not rocket science. My nurse knew this. Why didn’t my doctor?
Nicole Beasley January 6, 2026 AT 09:46
Wait so if I get itchy on morphine but not on fentanyl… I’m not allergic? 😳 I’ve been avoiding all opioids for 5 years because of this. I just got back surgery last week and was terrified. I asked for fentanyl with Benadryl and… no itch. I’m crying. Thank you for this.
sonam gupta January 7, 2026 AT 01:01
In India we dont even have access to these fancy opioids. We get paracetamol and sometimes tramadol. If someone gets itchy they just stop. No one cares. But still we suffer. This article is for rich countries. We need pain relief first, then education.