
Health December 19, 2025
Antiretroviral Generics in Africa: How Local Production Is Transforming HIV Treatment Access
For years, millions of people living with HIV in Africa relied on medicines shipped from halfway across the world. Tablets made in India, packed in boxes, cleared customs, and traveled through long, fragile supply chains just to reach a clinic in rural Mozambique or a township in Nigeria. That system worked - barely. But it was never sustainable. Then, in May 2025, everything changed. For the first time in history, the Global Fund bought HIV treatment made in Africa. Not just any treatment - TLD, the current gold-standard antiretroviral combo of tenofovir, lamivudine, and dolutegravir - produced by a Kenyan company, Universal Corporation Ltd. And it wasn’t a test run. It was enough to treat over 72,000 people a year.
Why Local Production Matters More Than Ever
Sub-Saharan Africa carries 65% of the world’s HIV cases, yet produces less than 3% of its own medicines. That gap isn’t just a statistic - it’s a lifeline problem. When the pandemic hit, borders closed. Air cargo stalled. Countries scrambled. Some ran out of ARVs for months. People stopped taking their pills. Viral loads rose. Resistance grew. The system didn’t just break - it exposed how dangerous it is to depend on others for your survival.
Local production flips that script. When medicines are made in Africa, for Africa, supply chains shrink. Delivery times drop from months to weeks. Costs fall because you cut out shipping, tariffs, and middlemen. And when a country makes its own drugs, it gains control. No more waiting for donors to decide what’s available. No more price shocks from global markets. This isn’t just about HIV. It’s about health sovereignty.
The TLD Breakthrough: What Changed in 2023 and 2025
The real turning point came in 2023, when Universal Corporation Ltd became the first African manufacturer to get WHO prequalification for TLD. That’s not just a badge. It’s the gold standard. WHO prequalification means the drug meets the same quality, safety, and effectiveness benchmarks as those made in the U.S. or Europe. It’s the green light the Global Fund, UNICEF, and other major buyers need before they spend a single dollar.
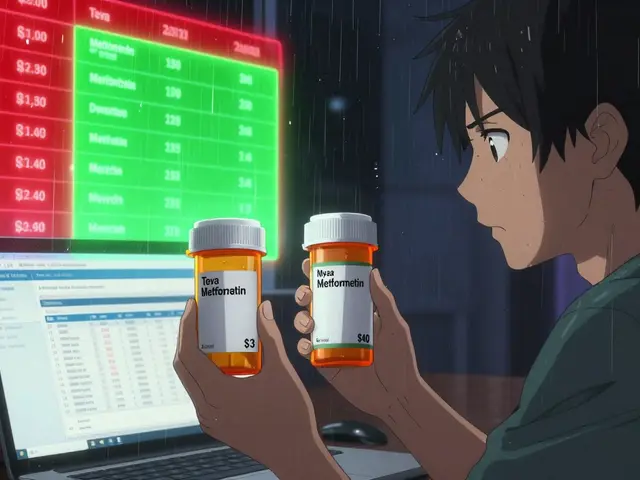
Before this, African countries had two choices: expensive brand-name drugs or cheap generics from India. The Indian generics brought prices down from $10,000 per patient per year in 2000 to under $100 by 2015. Huge win. But India’s production wasn’t built for Africa’s needs. It didn’t account for regional drug resistance patterns. It didn’t respond quickly to spikes in demand. And when global supply chains got disrupted, Africa was last in line.
Now, with TLD made in Kenya and shipped directly to Mozambique, the model is different. It’s predictable. It’s faster. It’s owned. The Global Fund didn’t just buy medicine - it bought confidence in African manufacturing. And that’s what’s starting to change everything.
Who’s Building the Future - And Where
Kenya isn’t alone. Nigeria’s Codix Bio just started making HIV rapid diagnostic tests after receiving a technology transfer from SD Biosensor, backed by WHO’s Health Technology Access Programme. That’s huge. You can’t treat what you can’t detect. Now, clinics in rural areas can test and start treatment in the same visit - no need to send samples to Lagos or Abidjan.
South Africa is moving fast too. In October 2025, it became the first African country to register the twice-yearly HIV injection, cabotegravir long-acting (CAB LA). Six local companies got licenses from Gilead to make generic versions. Experts say prices could drop 80-90% once generics hit the market. That means more people can get the treatment - and stick with it. No more daily pills. Just two shots a year. That’s life-changing for someone who works long hours, travels often, or lives far from a clinic.
And it’s not just ARVs. Gilead is working with the U.S. State Department and the Global Fund to supply lenacapavir, a new long-acting PrEP drug, at no profit until generics are ready. They’re submitting regulatory applications in 18 high-burden countries by the end of 2025. That’s not charity - it’s strategy. They’re creating a bridge to local production.
The Numbers Don’t Lie - But They’re Still Not Enough
Let’s put this in perspective. Africa needs about 15 million person-years of first-line ARV treatment every year. Right now, African-made generics cover maybe 1-2% of that. The Global Fund’s first TLD order? Enough for 72,000 people. That’s a drop in the ocean - but it’s the first drop that matters.
The African Union’s Pharmaceutical Manufacturing Plan for Africa (PMPA) wants to get local production up to 40% by 2040. That’s ambitious. And it’s possible - but only if three things happen: better regulation, more investment, and stronger markets.
Right now, every African country has its own drug approval process. One drug approved in South Africa might take two years to get cleared in Nigeria. Harmonizing those rules is the next big challenge. Then there’s money. Building a factory that meets WHO standards costs tens of millions. Who pays? The Gates Foundation, Unitaid, and CIFF are stepping in with market-shaping funds - but it’s not enough. African governments need to invest too. Not just in factories, but in training pharmacists, inspectors, and lab technicians.
What’s Next? The Long-Term Vision
This isn’t just about HIV anymore. It’s about building a system that can respond to the next pandemic, the next outbreak, the next health crisis. When you have labs that can make ARVs, you can make vaccines. When you have supply chains that move medicines fast, you can move insulin, antibiotics, or maternal health drugs too.
And it’s not just about making pills. It’s about making knowledge. African scientists are starting to lead clinical trials for drugs tailored to regional strains of HIV. That’s something no Indian or Western lab could do as well. Because the virus evolves differently here. The people’s needs are different. The access barriers are different. Local production means local research. And that’s where real innovation happens.
By 2030, experts predict African-made ARVs could cover 20-30% of the continent’s needs. That’s not the finish line - it’s the starting line. The goal isn’t just to replace imports. It’s to build an industry that creates jobs, trains engineers, powers innovation, and gives Africa control over its own health future.

Challenges Still Loom
Don’t get it twisted - this isn’t a fairy tale. There are still big problems. Regulatory systems are slow. Power outages shut down factories. Skilled workers leave for better pay abroad. Some governments still buy cheaper, lower-quality imports because they’re easier to get through procurement systems.
And let’s not forget: even with local production, you still need funding. The Global Fund and PEPFAR aren’t going away. But the goal is to make Africa less dependent on them - not to replace them. It’s about shifting from aid to partnership.
Integration is another hurdle. HIV programs have run in silos for decades. Nurses trained only on ARVs. Labs only for HIV testing. Clinics don’t talk to maternal health units. The future means combining HIV services with diabetes care, TB treatment, and mental health support - all under one roof. That’s more efficient. And it’s cheaper.
Why This Is a Game Changer
Twenty years ago, an HIV diagnosis in Africa was a death sentence. Today, it’s a manageable condition - thanks to antiretrovirals. But access was always the bottleneck. Now, the bottleneck is breaking.
The fact that a Kenyan company made a drug that met WHO standards and got bought by the Global Fund? That’s historic. It tells African manufacturers: you can compete. It tells African governments: you can lead. It tells people living with HIV: your treatment doesn’t have to come from someone else’s country.
This isn’t just about pills. It’s about dignity. About self-reliance. About a continent finally writing its own health story - not just reading someone else’s.
Write a comment
Items marked with * are required.



15 Comments
Dorine Anthony December 20, 2025 AT 00:24
This is actually kind of beautiful. I never thought I'd see the day when Africa was making its own life-saving meds and the Global Fund was buying them straight up. No middlemen. No delays. Just dignity.
It’s the kind of thing that makes you believe in progress again.
Carolyn Benson December 21, 2025 AT 14:23
Let’s not romanticize this. Local production sounds noble, but it’s still a drop in the ocean. 72,000 people out of 15 million? That’s 0.48%. You’re celebrating a teaspoon while the ocean is still drying up.
Real sovereignty isn’t about making pills - it’s about dismantling the entire colonial architecture of global health. And we’re not even close.
Aadil Munshi December 22, 2025 AT 14:28
Oh wow, Kenya made TLD? Cool. Now tell me how many of those pills are actually getting to the people who need them, or are they sitting in a warehouse in Nairobi while some bureaucrat waits for the right color of stamp?
Also, let’s not pretend Indian generics were the problem. They dropped prices from $10k to $100. That’s the real miracle. African production? It’s just the latest flavor of ‘African solution’ hype. The math still doesn’t add up.
Danielle Stewart December 22, 2025 AT 17:29
Let me just say - this is the kind of progress we should be cheering for. Not because it’s perfect, but because it’s possible.
Someone believed in African science. Someone invested. Someone didn’t give up. That’s the real story here. The rest? We’ll fix it - one clinic, one factory, one trained pharmacist at a time.
Erica Vest December 23, 2025 AT 19:15
The WHO prequalification of Universal Corporation Ltd’s TLD is a landmark regulatory achievement. Prior to this, no African manufacturer had met the stringent GMP, pharmacovigilance, and stability testing requirements for a fixed-dose combination antiretroviral. This sets a precedent for future submissions from other regional producers.
Furthermore, the reduction in logistical latency from 90+ days to under 14 days significantly improves adherence metrics - a critical factor in suppressing viral resistance.
Kinnaird Lynsey December 24, 2025 AT 18:24
I get why people are excited. But let’s be real - this feels like the kind of thing that gets a TED Talk and then disappears into a donor report.
I’ve seen this movie before. ‘Local production!’ they say. Then the funding dries up, the power goes out, the engineers leave for Europe, and suddenly it’s 2028 and we’re back to importing from India.
Hope is good. Sustained investment? That’s the hard part.
shivam seo December 25, 2025 AT 23:03
Oh great, another African miracle. Meanwhile, the U.S. and EU are still the ones funding 90% of this. Don’t act like Africa is doing this on its own. Someone’s gotta pay for the labs, the machines, the training.
It’s not sovereignty - it’s just a fancy rebrand of foreign aid with more PowerPoint slides.
Andrew Kelly December 26, 2025 AT 23:28
Wake up. This is all a distraction. The real reason the Global Fund bought African-made TLD? Because they’re being pressured by activists to ‘decolonize’ aid. Not because it’s better. Not because it’s cheaper. Because it’s politically correct.
Meanwhile, real patients are dying because some NGO director wanted to feel good about their impact metrics.
Stop pretending this is about health. It’s about virtue signaling.
Anna Sedervay December 28, 2025 AT 19:30
Did you know? The Kenyan factory that makes TLD is actually owned by a Swiss holding company with ties to a pharmaceutical conglomerate that also owns the patent for the original brand drug? It’s all a shell game. They’re just outsourcing production to avoid tariffs.
And the WHO prequalification? That’s just a rubber stamp now - they’ve lowered standards to ‘support African development.’ It’s not medicine. It’s performance art.
Also, I read on a blog that dolutegravir causes neural tube defects in 1 in 200 births. Are we really comfortable giving this to women without proper prenatal screening? No one’s talking about that.
Ashley Bliss December 29, 2025 AT 07:10
Twenty years ago, a child in Malawi got an HIV diagnosis and her mother cried because she knew it was a death sentence.
Now? She gets a pill. From her own country. Made by people who look like her. Who speak her language. Who understand her life.
That’s not just medicine. That’s healing. That’s hope with a pulse.
I’m not crying. You’re crying.
Meenakshi Jaiswal December 31, 2025 AT 00:41
As someone from India, I’ve seen how our generics changed the game. But I also know the limits - we didn’t design for African resistance patterns, we didn’t adapt packaging for low-literacy communities, we didn’t train local pharmacists.
This African-led shift? It’s the next evolution. Local manufacturing + local context = better outcomes. Simple.
And yes, it’s still small. But momentum is everything. Keep going.
Mahammad Muradov January 1, 2026 AT 13:01
Let’s be honest - this only happened because the West got scared. Pandemic exposed their fragility. Now they’re handing over scraps to Africa so they don’t look bad.
Real sovereignty? You don’t get it from donor grants. You get it by building your own R&D, your own supply chains, your own patents.
Right now, Africa is still playing catch-up. And the rules are still written in Geneva and New York.
Connie Zehner January 3, 2026 AT 11:24
OMG I just cried 😭 this is the most beautiful thing I’ve read all year. Someone finally did something right. I’m so proud of Africa 🙌 I’m sharing this with EVERYONE. Like, right now. 💪❤️
holly Sinclair January 5, 2026 AT 10:47
What’s interesting here isn’t just the production - it’s the epistemological shift. For centuries, medical knowledge was extracted from African bodies and processed in Western labs, then sold back as commodities. Now, for the first time, African scientists are generating data from African populations, using African infrastructure, to produce interventions tailored to African realities.
This isn’t just pharmaceutical independence - it’s a reclamation of medical ontology. The virus evolves differently here. The social determinants are different. The lived experience is different. And now, the response is being authored by those who live it.
That’s revolutionary. Not because it’s efficient. But because it’s truthful.
Monte Pareek January 6, 2026 AT 03:20
This is the future. Africa doesn’t need to wait for permission to heal itself.
Look at Nigeria making rapid tests. South Africa rolling out two-shot-a-year HIV treatment. Kenya meeting WHO standards. These aren’t lucky breaks - they’re the result of years of quiet work by engineers, pharmacists, nurses, and policymakers who refused to accept ‘it’s too hard’ as an answer.
Don’t call it aid. Call it partnership. And don’t you dare call it charity.
Next stop: vaccines. Then insulin. Then cancer drugs. Africa is just getting started.