Health November 13, 2025
Fluoroquinolones and Delirium in Older Adults: What You Need to Know
Fluoroquinolone Risk Assessment for Older Adults
Assess Your Risk
This tool helps evaluate the risk of fluoroquinolone-induced delirium for older adults based on key factors. Use it to make informed decisions about antibiotic selection.
Risk Assessment Results
When an older adult suddenly becomes confused, hallucinates, or can’t remember where they are, doctors often check for strokes, infections, or medication interactions. But one of the most common - and preventable - causes is often overlooked: fluoroquinolones.
What Are Fluoroquinolones?
Fluoroquinolones are a class of antibiotics used to treat serious bacterial infections like pneumonia, urinary tract infections, and kidney infections. Common ones include ciprofloxacin, levofloxacin, and moxifloxacin. They work by stopping bacteria from copying their DNA, which kills them off. These drugs are powerful and effective - which is why they’ve been prescribed for decades.
But here’s the problem: they don’t just target bacteria. Fluoroquinolones can cross the blood-brain barrier easily. Once inside the brain, they interfere with GABA-A receptors - the brain’s main calming system. This throws off the balance between excitation and inhibition, leading to neurological chaos. In older adults, this can trigger delirium - a sudden, severe confusion that can feel like a mental breakdown.
What Does Fluoroquinolone-Induced Delirium Look Like?
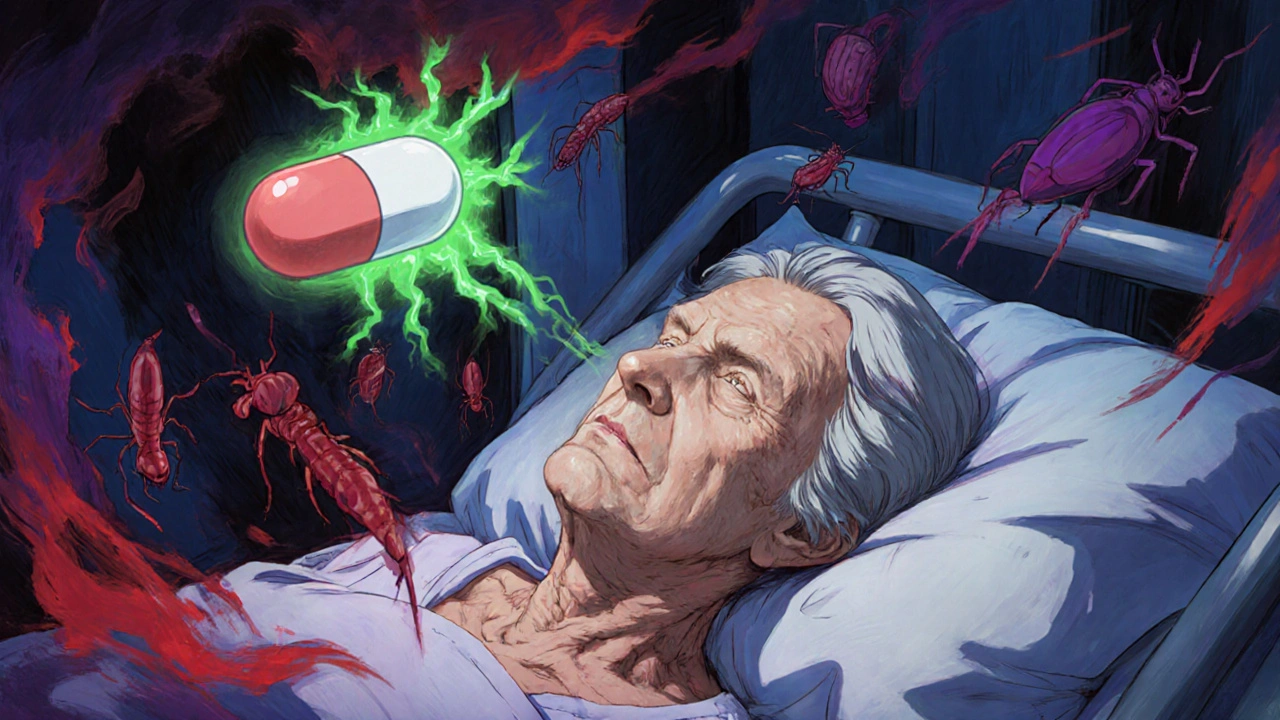
Delirium isn’t just being forgetful. It’s acute, fluctuating, and dangerous. Symptoms usually appear within 1 to 3 days of starting the antibiotic. People may:
- Not recognize family members or their own home
- See or hear things that aren’t there - voices, shadows, bugs crawling on the wall
- Struggle to focus on a conversation or follow simple instructions
- Become agitated, aggressive, or unusually withdrawn
- Have trouble sleeping or stay awake all night
One case published in the PMC6089571 report described a 72-year-old woman who started levofloxacin for a UTI. On day three, she became terrified, screaming that the walls were breathing. She didn’t know the year or where she was. Her EEG and brain scan were normal. Her electrolytes were fine. The only change? She’d started an antibiotic two days earlier. When doctors stopped it, she returned to baseline in 48 hours.
This isn’t rare. A 2016 review in Neurology analyzed 391 cases of antibiotic-related delirium. Fluoroquinolones were responsible for nearly 18% of them - more than any other antibiotic class. And it’s not just one drug. Levofloxacin and ciprofloxacin are the most commonly reported, but moxifloxacin and gemifloxacin have also triggered similar reactions.
Why Are Older Adults So Vulnerable?
It’s not just age. It’s biology.
As we get older, our kidneys slow down. About 85% of levofloxacin leaves the body through the kidneys. If kidney function drops - and many older adults have mild, undiagnosed decline - the drug builds up in the bloodstream. Higher levels mean more brain exposure.
Older brains also have fewer GABA receptors and less ability to compensate when those receptors are blocked. The blood-brain barrier becomes more permeable with age, letting more of the drug in. Many older adults already have mild cognitive changes - maybe they forget names or misplace keys. Fluoroquinolones don’t cause dementia. But they can push a fragile system over the edge.
Studies show that over 40% of hospitalized adults over 65 develop delirium during their stay - and fluoroquinolones are one of the top triggers. The American Geriatrics Society now lists fluoroquinolones as “potentially inappropriate medications” for seniors in their 2023 Beers Criteria. That means: avoid them if you can.
How Common Is This Side Effect?
It’s rare - but deadly.
Less than 0.5% of people taking fluoroquinolones develop neuropsychiatric side effects. That sounds small. But when you consider that over 26 million fluoroquinolone prescriptions were filled in the U.S. in 2019, even 0.5% means tens of thousands of people are at risk.
And here’s the catch: most cases go unreported. Doctors don’t always connect the dots. A Reddit post from a physician with 10 years of experience said he’d seen three cases of fluoroquinolone-induced delirium - each took 24 to 48 hours to recognize. By then, the patient was already in a hospital bed, possibly restrained, possibly sedated.
The FDA issued a safety alert in July 2018, adding delirium, memory loss, and attention problems to the official warning label. But prescribing habits haven’t changed fast enough. A 2020 JAMA Network Open study found that after the 2016 and 2018 warnings, fluoroquinolone use in older adults dropped by just 20.4%. That’s progress - but not enough.
What Should Doctors Do Instead?
Fluoroquinolones are not first-line for most infections. For urinary tract infections in older adults, nitrofurantoin or trimethoprim-sulfamethoxazole are safer. For pneumonia, amoxicillin-clavulanate or doxycycline often work just as well - and don’t touch the brain.
Some beta-lactams like cefepime can also cause neurotoxicity, but they’re less likely to trigger delirium than fluoroquinolones. The key is choosing an antibiotic that targets the infection without crossing into the brain unnecessarily.
Hospitals are starting to catch on. UCSF Medical Center cut levofloxacin use for UTIs in elderly patients by 35% after implementing a protocol that flags high-risk patients before prescribing. That kind of change saves lives.
What If You or a Loved One Is Already on Fluoroquinolones?
If someone over 65 is taking ciprofloxacin, levofloxacin, or another fluoroquinolone and suddenly seems confused, disoriented, or hallucinating - don’t wait. Call the doctor immediately. Do not stop the drug on your own unless told to - but do insist on evaluation.
Doctors should check for:
- Normal electrolytes (sodium, calcium, glucose)
- Normal kidney function
- No signs of stroke or infection in the brain
- No recent changes in other medications
If all those are clear and the person started a fluoroquinolone within the last 72 hours - stop it. The symptoms almost always reverse within 48 to 96 hours. In one case, a patient’s baseline cognition returned fully after just 72 hours off the drug.
Don’t assume it’s “just aging.” Don’t assume it’s dementia. Don’t assume it’s “psychiatric.” It could be a simple, reversible reaction to a common antibiotic.
How to Prevent It
Prevention is the best strategy. Here’s what works:
- Avoid fluoroquinolones in people over 65 unless there’s no other option - and even then, use the lowest effective dose.
- Check kidney function before prescribing. If creatinine clearance is below 50 mL/min, reduce the dose or choose another antibiotic.
- Don’t use fluoroquinolones for simple UTIs, sinus infections, or bronchitis - these are usually viral or can be treated with safer drugs.
- Monitor closely in the first 72 hours of treatment. Ask family members: “Has their behavior changed?”
- Use alternatives: Nitrofurantoin, fosfomycin, amoxicillin, doxycycline, or cephalexin are often just as effective and much safer.
The CDC now recommends fluoroquinolones be reserved for infections with no alternative treatment options - especially in older adults. That’s not a suggestion. It’s a standard of care.
What’s Next?
Research is moving forward. Scientists are studying biomarkers that might predict who’s most at risk. Clinical decision tools are being built into electronic health records to warn doctors before they prescribe. New fluoroquinolone derivatives with less brain penetration are in early development.
But right now, the answer is simple: stop treating older adults like they’re just smaller versions of younger patients. Their bodies process drugs differently. Their brains are more sensitive. And what’s safe for a 40-year-old can be dangerous for a 75-year-old.
If you’re a caregiver, ask: “Is this antibiotic really necessary?” If you’re a doctor, ask: “Could this be causing more harm than good?”
Fluoroquinolones saved lives. But they’re not magic bullets. And in older adults, the cost can be too high.
Can fluoroquinolones cause permanent brain damage?
No, fluoroquinolone-induced delirium is almost always reversible. Symptoms typically resolve within 48 to 96 hours after stopping the drug. There’s no evidence it causes permanent cognitive decline. However, if delirium isn’t recognized and treated quickly, it can lead to longer hospital stays, increased risk of falls, or even death - especially in frail older adults.
Are all fluoroquinolones equally risky?
No. Levofloxacin and ciprofloxacin have the most documented cases of delirium in older adults. Moxifloxacin and gemifloxacin are also linked, but less frequently. The risk is tied to how much of the drug reaches the brain - and levofloxacin achieves 50-90% of plasma levels in cerebrospinal fluid, making it especially likely to cause neurological side effects.
Can I take fluoroquinolones if I have kidney problems?
If you have reduced kidney function (CrCl < 50 mL/min), fluoroquinolones should be avoided or significantly dosed down. Most of the drug is cleared by the kidneys, so poor function leads to buildup in the blood - and higher brain exposure. Safer alternatives like nitrofurantoin or cephalexin are preferred in these cases.
Why don’t doctors always know about this risk?
Delirium is often mistaken for dementia, depression, or psychiatric illness. Antibiotics aren’t usually the first thing doctors suspect. Many weren’t trained to link sudden confusion to an antibiotic started just days earlier. The FDA warning came in 2018, but awareness still lags in clinical practice - especially in outpatient settings.
What are the safest antibiotics for older adults?
For urinary tract infections: nitrofurantoin or trimethoprim-sulfamethoxazole. For pneumonia: amoxicillin-clavulanate or doxycycline. For skin infections: cephalexin or clindamycin. These have minimal brain penetration and far lower risk of delirium. Always ask: Is there a safer option?
Write a comment
Items marked with * are required.






10 Comments
Brian Bell November 14, 2025 AT 14:47
Yikes. My grandma was on cipro for a UTI and started screaming at the ceiling like there were demons. We thought she was dying. Turns out? Just the antibiotic. She bounced back in two days after they pulled it. Why is this still a thing?
Ashley Durance November 15, 2025 AT 09:47
Let’s be real - this isn’t ‘negligence.’ It’s systemic laziness. Doctors are overworked, underpaid, and trained to treat symptoms, not root causes. They see ‘confusion’ and reach for the easiest diagnostic shortcut: dementia. Meanwhile, the real culprit - a $10 antibiotic - sits silently in the cabinet. The FDA warning? A footnote. The Beers Criteria? A PDF nobody reads. This is preventable medical malpractice dressed up as ‘standard care.’
Ryan Anderson November 17, 2025 AT 05:49
My mom had this happen last year. We thought she was having a stroke. ER said ‘probable dementia.’ Took three days and a family member who actually read the medication list to connect the dots. She’s fine now - but the trauma? Lasted months. 🙏 Please, if you’re a clinician: check the script before the scan.
Nathan Hsu November 18, 2025 AT 12:20
India, too, has seen this - in private hospitals, where antibiotics are sold like candy. My uncle, 74, was given levofloxacin for a ‘mild cough’ - and within 48 hours, he was seeing ‘ghosts’ in the mirror. The doctor laughed - ‘old people get weird.’ We switched antibiotics, and he returned to himself. But why does this keep happening? Because profit > precaution. Because ‘it’s just a UTI’ - and ‘it’s just old age.’
Kevin Wagner November 18, 2025 AT 13:52
THIS IS A SCANDAL. We’re poisoning our grandparents with pills that were never meant for their bodies. Fluoroquinolones are the nuclear option - and we’re using them to kill a mosquito. The fact that this is still happening in 2025? It’s not ignorance. It’s arrogance. We treat seniors like broken machines that need a quick fix - not humans with delicate, aging biology. Stop it. Fight for safer options. Demand better. Your grandma might be next.
Don Ablett November 18, 2025 AT 21:16
The pharmacokinetic data is unambiguous. Renal clearance declines by approximately 1% per year after age 40. Fluoroquinolones are renally excreted at 70-90 percent. The blood-brain barrier permeability increases with age due to reduced tight junction integrity. These are not theoretical risks. They are measurable, quantifiable, and predictable. The failure to adjust prescribing practices is not an oversight. It is a failure of clinical pharmacology education.
Hrudananda Rath November 20, 2025 AT 12:26
One must wonder whether this is a deliberate consequence of pharmaceutical marketing. The fluoroquinolone class has generated billions in revenue. The FDA warning, while technically present, is buried in the fine print. Medical education, increasingly corporatized, omits nuanced risk-benefit analysis in favor of branded protocols. The elderly are not merely vulnerable - they are monetarily expendable in the current paradigm. One cannot help but feel that this is not an accident. It is an economy.
Joe Goodrow November 21, 2025 AT 14:35
What’s next? Banning aspirin because old folks get tinnitus? This is why America’s healthcare is collapsing - everyone’s scared of lawsuits so they just avoid everything. My dad’s 78, had a UTI, took cipro, slept fine. No delirium. Maybe it’s not the drug - maybe it’s the weak-minded generation that thinks every old person is a walking dementia case.
Eleanora Keene November 23, 2025 AT 02:55
My mom’s a nurse - she told me about a patient who got so confused on cipro they tried to climb out the window. They stopped the med, and within 36 hours, he was joking again. It’s so simple. Why don’t we just… ask? Check the med list? Talk to family? It’s not rocket science. We just need to care enough to look. 💙
Scott Saleska November 24, 2025 AT 07:45
As someone who works in geriatrics - I see this every week. But here’s the thing: most patients are prescribed these drugs in outpatient settings - urgent care, primary care, even pharmacies. No one’s monitoring them. No one’s calling back. The system is designed for speed, not safety. I’ve started a checklist in my clinic: ‘Is this really necessary?’ - and if the answer isn’t a hard yes, we pick something else. It’s slow. It’s inconvenient. But it saves lives. And honestly? It’s the bare minimum.