Health January 24, 2026
Autonomic Neuropathy: Why Blood Pressure Drops and GI Symptoms Happen
When you stand up, your body should automatically adjust your blood pressure to keep you from feeling dizzy or fainting. But for people with autonomic neuropathy, that automatic system breaks down. Their blood pressure plummets, their stomach stops working properly, and simple actions like walking to the kitchen or eating a meal become exhausting, unpredictable, or even dangerous. This isn’t just about being a little lightheaded-it’s a neurological disorder that quietly disables daily life.
What Is Autonomic Neuropathy?
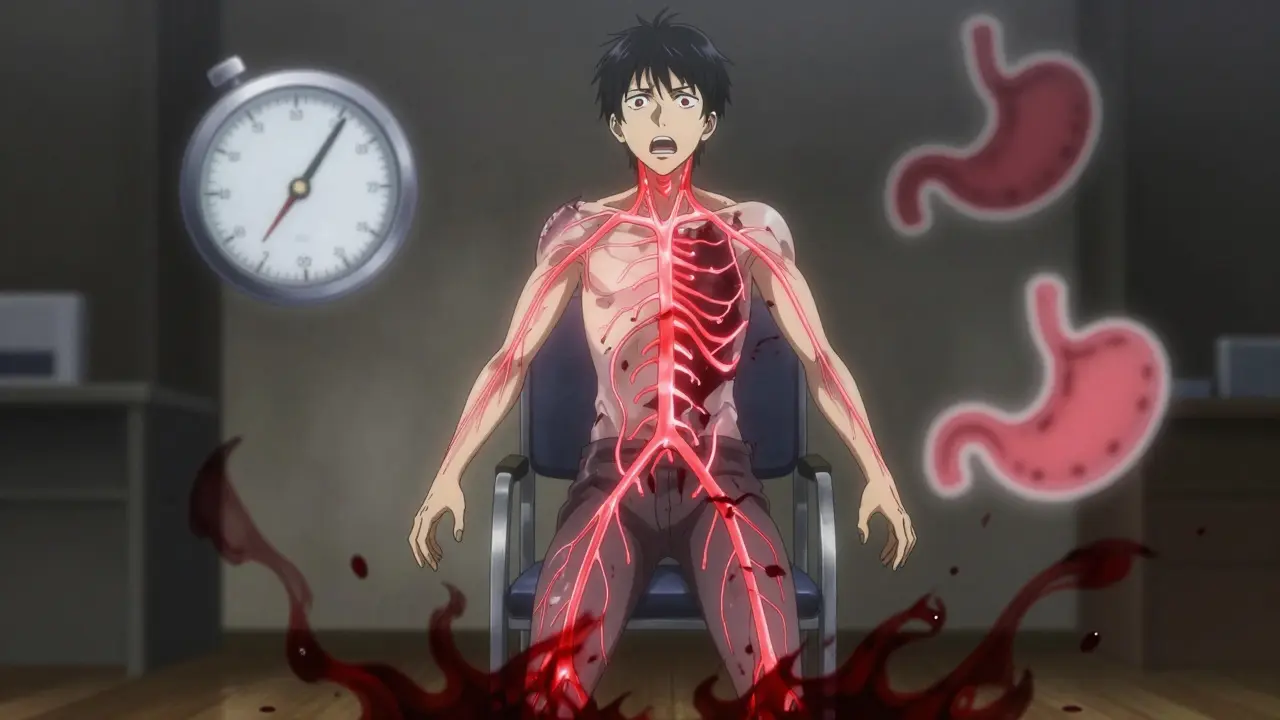
Autonomic neuropathy damages the nerves that control involuntary functions-things your body does without you thinking about it: heart rate, digestion, blood pressure, sweating, and bladder control. These nerves are part of the autonomic nervous system, and when they’re damaged, your body can’t respond to changes like standing up, eating, or even being in a hot room.
Most cases-85% to 90%-are linked to diabetes. High blood sugar over years slowly destroys the tiny blood vessels that feed these nerves. But it’s not just diabetes. Autoimmune diseases, chemotherapy, Parkinson’s, and even some viral infections can trigger it. The problem? Many people don’t know they have it until symptoms become severe. Doctors miss it because the signs look like normal aging or stress.
Why Your Blood Pressure Drops When You Stand Up
Standing up should trigger a reflex: your blood vessels tighten, your heart beats a little faster, and your blood pressure stays steady. In autonomic neuropathy, that reflex fails. The nerves telling your blood vessels to constrict are damaged, so blood pools in your legs. Your brain doesn’t get enough blood. That’s orthostatic hypotension.
It’s not just a quick dizzy spell. A true diagnosis means your systolic blood pressure drops by at least 20 mmHg or your diastolic drops by 10 mmHg within three minutes of standing. In severe cases, the drop can be 35 mmHg or more. One study found that 68% of people with confirmed autonomic neuropathy had systolic blood pressure below 90 mmHg when standing-enough to cause fainting or near-fainting episodes several times a week.
Some people develop POTS instead-Postural Orthostatic Tachycardia Syndrome. Here, blood pressure doesn’t drop much, but the heart races. It jumps by 30 beats per minute or hits over 120 bpm within 10 minutes of standing. It’s exhausting. People describe it as feeling like they’ve run a marathon just by walking to the bathroom.
And it’s not just standing. Even mild activity like walking for six minutes can only get you to 55-65% of your expected heart rate, compared to 85-90% in healthy people. Your body just can’t keep up.
What’s Going On in Your Gut?
While blood pressure issues grab attention, gastrointestinal symptoms are just as common-and often more disruptive. About one in three people with autonomic neuropathy develop gastroparesis: a condition where the stomach empties too slowly. Food sits there for hours. You feel full after a few bites. Nausea comes and goes. Vomiting, especially at night, happens in 78% of those with severe cases.
It’s not just the stomach. The whole digestive tract slows down. Constipation affects 60% of patients. Bowel movements drop from a normal 4-5 times a week to just 1-2. But then, paradoxically, 25% get diarrhea-often at night. It’s not infection. It’s because food sits too long in the small intestine, letting bacteria overgrow. That’s SIBO-small intestinal bacterial overgrowth-and it’s found in over half of autonomic neuropathy patients with GI symptoms.
Swallowing can become hard too. The esophagus doesn’t contract properly. About 40-60% of patients show abnormal muscle movements on testing. That leads to choking, regurgitation, or a feeling that food is stuck.
These aren’t minor inconveniences. People avoid restaurants, skip family dinners, cancel plans because they don’t know if they’ll be sick or bloated. One patient on a support forum said, “I used to love pizza nights with my kids. Now I eat broth and mashed potatoes in silence while they eat in the other room.”
How Doctors Diagnose It
There’s no single blood test. Diagnosis relies on a mix of symptom tracking and physical tests. The most common starting point is the 10-minute active stand test: you lie down, then stand up while your blood pressure and heart rate are monitored every few minutes. A drop of 20/10 mmHg confirms orthostatic hypotension.
Heart rate variability testing during deep breathing is another key tool. Healthy people’s heart rate increases when they breathe in and drops when they breathe out. In autonomic neuropathy, that difference shrinks to near zero. The Valsalva maneuver-forcing air out against a closed airway-also checks how well your nerves regulate blood pressure. If your body can’t recover properly, that’s a red flag.
For GI issues, gastric emptying scintigraphy is the gold standard. You eat a meal with a tiny radioactive tracer, and a camera tracks how fast it leaves your stomach. If more than 10% remains after four hours, you have gastroparesis. Newer tests like wireless motility capsules are just as accurate and less invasive.
Doctors also use questionnaires like the COMPASS-31, which scores autonomic symptoms from 0 to 100. A score above 30 means significant dysfunction. It’s not perfect, but it’s reliable-and it helps patients explain what they’re feeling when doctors don’t believe them.
Treatment: What Actually Works
There’s no cure, but there are ways to manage symptoms. For blood pressure drops, fludrocortisone helps by increasing fluid volume, but it can cause high blood pressure when lying down. Midodrine tightens blood vessels and helps 70% of people, but you have to take it at the right times-never before bed-or you’ll wake up with a pounding headache from supine hypertension.
For POTS, ivabradine can slow a racing heart without lowering blood pressure. In studies, it reduces heart rate by 15-25 beats per minute in two-thirds of users. That’s life-changing for someone who can’t walk across a room without their heart racing out of control.
For the gut, metoclopramide was once the go-to, but it carries a serious risk of permanent movement disorders after just 12 weeks. Erythromycin works short-term, but your body gets used to it fast. The newer recommendation? Pyridostigmine. It improves symptoms in over half of patients with minimal side effects.
But the most effective treatments aren’t pills. They’re lifestyle changes. Wearing compression stockings (30-40 mmHg) reduces orthostatic symptoms by 35%. Abdominal compression garments help with bloating and nausea. Eating six small meals a day instead of three big ones cuts vomiting episodes in half. Avoiding fat and fiber makes digestion easier. Drinking more water and adding salt (under medical supervision) helps maintain blood volume.
One patient shared: “The low-fat, low-residue diet cut my vomiting from five times a day to once every three days. Worth every social sacrifice.”

The Hidden Cost of Being Undiagnosed
Most people wait years before getting a diagnosis. The average is 4.7 years. During that time, they’re told they’re anxious, depressed, or just “getting older.” They see three, four, even five doctors. By the time they’re diagnosed, their nerves are already badly damaged.
And the consequences are serious. Autonomic neuropathy increases the risk of sudden cardiac death by 5.5 times. People with severe cases live 8.2 years less than those with diabetes alone. It’s not just about quality of life-it’s about survival.
But awareness is growing. The American Diabetes Association now recommends screening all diabetics with more than seven years of disease using a simple three-minute stand test. That could catch half a million new cases a year.
And research is moving forward. Scientists are now measuring neurofilament light chain in blood-a protein that rises when nerves are damaged. It could become a simple blood test to catch autonomic neuropathy before symptoms even start.
What You Can Do Now
If you have diabetes and you’re dizzy when you stand up, or you’re always bloated, nauseous, or constipated, don’t brush it off. Ask your doctor for an autonomic screening. Bring up the COMPASS-31 questionnaire. Mention gastroparesis. Don’t wait until you faint at the grocery store.
And if you’re already diagnosed: you’re not alone. Support groups on Reddit and HealthUnlocked have tens of thousands of people sharing what works. Compression gear, dietary tweaks, pacing yourself-these aren’t just tips. They’re lifelines.
Autonomic neuropathy doesn’t have to mean giving up your life. It means learning how to live differently. And with the right tools, that’s possible.
Can autonomic neuropathy be reversed?
In early stages, strict blood sugar control in diabetics can slow or even partially reverse nerve damage. But once nerves are severely damaged, the changes are usually permanent. The goal shifts from reversal to symptom management. Early diagnosis is critical.
Is orthostatic hypotension the same as POTS?
No. Orthostatic hypotension means your blood pressure drops when you stand. POTS means your heart rate spikes dramatically, but your blood pressure stays normal or only drops slightly. Both are forms of autonomic dysfunction, but they have different causes and treatments. Some people have both.
Can diet really help with gastroparesis?
Yes. A low-fat, low-fiber diet with six small meals a day improves symptoms in 60% of patients. Fat and fiber slow digestion, so reducing them helps food move through the stomach faster. Liquid meals and pureed foods are often better tolerated than solid ones.
Why do I feel brain fog when my blood pressure drops?
When blood pressure drops too low, your brain doesn’t get enough oxygen. This causes mental confusion, difficulty focusing, and memory lapses-often called brain fog. It’s not psychological; it’s a direct result of reduced blood flow. Lying down or sitting with your head between your knees usually helps quickly.
Are there new treatments on the horizon?
Yes. Fecal microbiota transplantation (FMT) is being tested for GI symptoms, with early results showing 40% improvement in quality of life. Blood tests measuring neurofilament light chain may soon allow earlier diagnosis before symptoms appear. New drugs targeting nerve repair are also in early trials.
Write a comment
Items marked with * are required.



11 Comments
shivam utkresth January 25, 2026 AT 15:55
Man, this post hit different. I’ve been living with this for 6 years and no one ever told me it wasn’t just ‘being out of shape.’ The way they explained SIBO and how it ties to gastroparesis? That’s the first time I’ve seen it laid out like that. I used to think my bloating was just bad food choices. Turns out it’s my nerves throwing a tantrum. Compression socks saved my life. Also, pyridostigmine? Game changer. No more vomiting after every meal. Just wish I’d known this sooner.
Joanna Domżalska January 27, 2026 AT 00:18
So let me get this straight - you’re saying diabetes causes nerve damage, and that’s why people can’t stand up? Wow. So basically, if you eat too much pizza, your body just… gives up? That’s it? No other explanation? I mean, I’ve seen people with no diabetes have the same symptoms. Maybe it’s just laziness. Or bad posture. Or maybe people are just too soft now.
SWAPNIL SIDAM January 27, 2026 AT 12:12
Bro, I had a cousin who went through this. He was diabetic for 12 years, never checked his feet, never checked his BP when standing. One day he passed out in the grocery store. They found out he had autonomic neuropathy. He’s on meds now, wears compression gear, eats tiny meals like a bird. But man - he used to love biryani. Now he eats boiled rice and chicken broth. It’s sad. But he’s alive. That’s what matters.
Sally Dalton January 28, 2026 AT 17:45
omg this is so important!! i had no idea about the compas-31 thing!! i’ve been telling my dr for years that i get dizzy when i stand up and she just said ‘you’re stressed’ 😭 i printed out this whole post and handed it to her last week. she actually listened!! we’re scheduling the stand test tomorrow!! thank you thank you thank you 🙏❤️
Betty Bomber January 30, 2026 AT 05:13
Interesting. I’ve got POTS and gastroparesis. I don’t have diabetes. I had Lyme disease 8 years ago. No one connected it until now. Guess my body just decided to break down slowly. The brain fog is the worst. Feels like my thoughts are underwater. I just sit there and stare at my phone for 20 minutes trying to remember what I was going to say. Anyway - thanks for posting this. Feels less lonely now.
Mohammed Rizvi January 30, 2026 AT 21:45
Midodrine before bed? That’s like giving yourself a caffeine IV while you’re trying to sleep. I tried that. Woke up at 3 AM with my heart trying to punch its way out of my chest. Also, ‘low-fat, low-residue’? That’s just bland prison food. But hey - if it stops you from projectile vomiting at 2 AM, I guess I’ll eat mashed potatoes in silence too. Still, someone should invent a pill that makes your nerves stop being jerks.
Allie Lehto January 31, 2026 AT 01:58
People think this is just ‘medical stuff’ but really it’s a moral failure. If you just ate better, exercised more, didn’t drink soda, you wouldn’t be this sick. It’s not the nerves - it’s your choices. You’re letting your body rot. And now you want sympathy? No. You need discipline. Stop blaming science. Start blaming yourself.
Henry Jenkins January 31, 2026 AT 07:03
There’s a lot here, and I appreciate the depth. But I’m curious - what’s the actual prevalence of autonomic neuropathy in non-diabetic populations? The post says 10-15% of cases are non-diabetic, but with autoimmune, chemo, Parkinson’s, and viral triggers, that number might be higher. Also, the COMPASS-31 score above 30 indicates dysfunction - but is that validated across ethnic groups? Most studies are on Western populations. I’d love to see data from South Asian or African cohorts. Also, how does age interact with this? Are older non-diabetics being misdiagnosed as ‘just aging’? There’s a lot of clinical bias here that needs unpacking.
TONY ADAMS January 31, 2026 AT 20:36
Wait so you’re saying I’m not just lazy? I thought I was just bad at life. I’ve been sitting on the couch for 3 years because I get dizzy walking to the fridge. My wife says I’m depressed. But now I think it’s my nerves? I’m gonna go get tested. Thanks? I guess?
Karen Droege February 1, 2026 AT 04:29
Let me tell you - I’m a nurse who’s seen this in 30+ patients. The worst part isn’t the dizziness or the vomiting - it’s the loneliness. People stop inviting you out. Friends ghost you. Your kids think you’re ‘being dramatic.’ I’ve had patients cry because their grandkids don’t understand why they can’t eat birthday cake. And then there’s the medical gaslighting - ‘it’s anxiety,’ ‘you’re just old,’ ‘try yoga.’ It’s brutal. But here’s the hope: early detection works. Compression stockings, salt, small meals - they’re not glamorous, but they’re weapons. And if you’re reading this? You’re not broken. You’re fighting. And you’re not alone. I’ve got your back.
Napoleon Huere February 1, 2026 AT 05:10
Think about it - your body is a symphony. The autonomic nervous system is the conductor. When it’s damaged, the instruments play out of sync. The heart drums too fast, the stomach hums in silence, the blood vessels forget their notes. We treat symptoms like broken strings - but the real issue is the conductor’s silence. What if we could repair the conductor? Not just patch the violin? That’s the future. Not drugs. Not diets. Not compression socks. But neuroregeneration. We’re getting there. The neurofilament light chain test? That’s the first note of a new movement. We’re not just managing death anymore. We’re learning how to bring life back.