Health December 1, 2025
Beta-Blockers and Calcium Channel Blockers: What You Need to Know About Combination Therapy
Beta-Blocker + Calcium Channel Blocker Safety Checker
Patient Assessment
Enter your key measurements to determine if this drug combination is safe for you.
Combining beta-blockers and calcium channel blockers might sound like a smart way to tackle high blood pressure or chest pain-after all, two drugs should work better than one, right? But in reality, this combo isn’t a one-size-fits-all solution. It’s a tightrope walk between effectiveness and danger, especially when it comes to your heart. Some patients see real benefits. Others end up in the hospital with dangerously slow heart rates or worsening heart failure. The difference? Knowing which drugs you’re taking, who you are as a patient, and what your heart can handle.
How These Drugs Work-And Why They’re Combined
Beta-blockers, like metoprolol or atenolol, slow your heart down. They block adrenaline’s effect on your heart, lowering your heart rate and blood pressure. They also reduce how hard your heart pumps, which helps if you’ve had a heart attack or have angina. Calcium channel blockers, such as amlodipine or diltiazem, relax your blood vessels. This lowers blood pressure too, but they also reduce the force of your heart’s contractions by limiting calcium flow into heart and blood vessel cells.
When used together, they can bring down blood pressure more than either drug alone. That’s why doctors sometimes reach for this combo-especially if you have both high blood pressure and chest pain (angina). In fact, the European Society of Cardiology guidelines recommend beta-blocker plus calcium channel blocker combinations specifically for patients with hypertension and stable angina, where other treatments haven’t worked well enough. The idea is simple: one drug targets heart rate, the other targets vessel stiffness. Together, they cover more ground.
Not All Calcium Channel Blockers Are the Same
This is where things get tricky. Calcium channel blockers fall into two big groups-and mixing them with beta-blockers has wildly different outcomes depending on which one you use.
Dihydropyridines (like amlodipine, nifedipine) mainly relax blood vessels. They barely touch your heart’s electrical system. That makes them safer to pair with beta-blockers. In fact, studies show that amlodipine combined with a beta-blocker reduces the risk of stroke and heart failure more than other dual therapies, with fewer dangerous side effects. Most doctors feel comfortable using this combo in older adults or those with isolated high blood pressure.
Non-dihydropyridines (like verapamil and diltiazem) are different. They slow your heart’s electrical signals and weaken its pumping power. Add a beta-blocker to this mix, and you’re stacking two drugs that both slow the heart. The result? A dangerous drop in heart rate, prolonged PR intervals on an ECG, and even full heart block.
A 2023 study of nearly 19,000 patients found that verapamil combined with a beta-blocker caused serious bradycardia or heart block in 10-15% of users. One Reddit post from a cardiologist described losing a patient to complete heart block after adding verapamil to metoprolol in an 82-year-old with a borderline PR interval. That’s not rare. It’s a known risk.
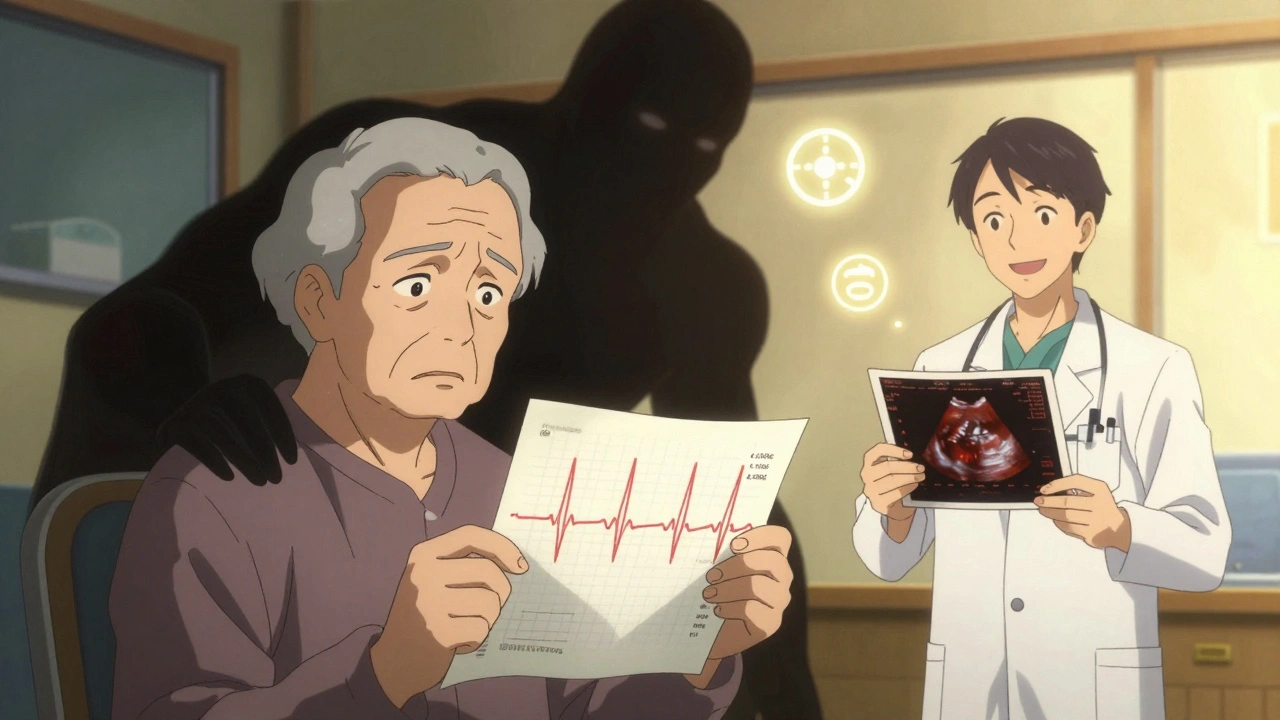
Who Should Avoid This Combo?
Some people simply shouldn’t get this combination at all. The guidelines are clear:
- Patients with sinus node dysfunction (a slow or unreliable natural pacemaker)
- Those with a PR interval over 200 milliseconds on their ECG
- Anyone with second- or third-degree heart block
- People with heart failure with reduced ejection fraction (HFrEF)
- Older adults (over 65) with borderline conduction issues
Even if you don’t know you have any of these, you might still be at risk. About 15% of people over 75 have undiagnosed conduction abnormalities. That’s why doctors are now required to check your ECG and heart function with an echocardiogram before starting this combo. Skipping these tests is like driving blindfolded.
What Happens When It Goes Wrong?
Side effects aren’t just annoying-they can be life-threatening.
With verapamil + beta-blocker combinations, heart rate can drop by 25-35 beats per minute-far more than with either drug alone. Your PR interval (the time it takes for an electrical signal to travel through your heart) can stretch by 40-80 milliseconds. That’s enough to cause dizziness, fainting, or sudden cardiac arrest.
Left ventricular function can tank too. In patients with existing heart weakness, combining these drugs can drop ejection fraction by 15-25%. That means your heart can’t pump blood as well. The result? More hospitalizations for heart failure. One study showed a 2.8-fold higher risk with verapamil versus amlodipine.
Even "safer" combos like amlodipine + beta-blocker aren’t perfect. About 22% of patients develop ankle swelling (peripheral edema). That’s 35% more than with other combinations. It’s not dangerous, but it’s uncomfortable-and often leads people to stop taking their meds.
Real-World Use: Who Gets This Therapy?
Despite the risks, this combo is still used. About 12% of dual therapy prescriptions in the U.S. are for beta-blockers plus calcium channel blockers, according to 2022 IQVIA data. But usage varies wildly by region. In China, it’s 22%. Why? Different guidelines. Different doctor habits.
Doctors who use it most often are targeting specific patients:
- Those with high blood pressure and angina
- Patients with resting heart rates above 80 bpm (beta-blockers help here)
- People who can’t tolerate ACE inhibitors or ARBs
But even then, they’re careful. A 2022 survey of 1,247 U.S. clinicians found that 78% prefer beta-blocker + amlodipine over any other combination for hypertension. Only 12% would consider verapamil, even in select cases. And 63% said their biggest fear is bradycardia.
One cardiologist from Massachusetts General Hospital reported treating over 200 patients with beta-blocker + amlodipine. Only 3% developed ankle swelling-and that was easily fixed by lowering the dose. No serious heart rhythm problems. That’s the kind of experience that builds confidence.
How to Use This Combo Safely
If your doctor recommends this combination, don’t panic-but don’t skip the steps either.
- Get an ECG first. Check your PR interval. If it’s over 200 ms, this combo is off the table.
- Do an echocardiogram. Know your ejection fraction. If it’s below 45%, avoid non-dihydropyridine CCBs entirely.
- Start low, go slow. Begin with half the usual dose of each drug. Wait a week before increasing.
- Monitor weekly for the first month. Track your heart rate and blood pressure at home. If your pulse drops below 50 bpm or you feel lightheaded, call your doctor.
- Know the red flags. Fainting, chest pain, sudden fatigue, or swelling in your legs aren’t normal. They mean stop and seek help.
Tools like the European Society of Cardiology’s online bradycardia risk calculator (validated in over 4,500 patients) can help doctors decide if you’re a good candidate. It’s not perfect-but it’s better than guessing.
The Future of This Combo
Is this therapy here to stay? Yes-but it’s getting more selective.
As of 2023, the American College of Cardiology is reviewing its guidelines after new data showed clear benefits of beta-blocker + amlodipine in reducing stroke and heart failure. Meanwhile, verapamil combinations are declining. The FDA added a boxed warning in 2021. The EMA now requires heart function tests before prescribing.
Industry analysts predict a 5.7% annual increase in beta-blocker + dihydropyridine prescriptions through 2028. Why? Aging populations, more hypertension, and smarter prescribing. The combo isn’t disappearing-it’s being refined.
What’s clear now is this: beta-blockers and calcium channel blockers can work together beautifully-if you pick the right ones and screen patients carefully. But when you mix the wrong ones, or skip the checks, the risks aren’t theoretical. They’re written in hospital records, Reddit threads, and obituaries.
Can beta-blockers and calcium channel blockers be taken together safely?
Yes-but only under strict conditions. The combination is safe when using a dihydropyridine calcium channel blocker like amlodipine with a beta-blocker, and only if you don’t have heart block, slow heart rate, or weakened heart muscle. Always get an ECG and echocardiogram before starting. Avoid verapamil or diltiazem with beta-blockers unless under close specialist supervision.
Which calcium channel blocker is safest with beta-blockers?
Amlodipine is the safest choice. It works mainly on blood vessels and has minimal effect on heart rhythm or pumping strength. Studies show it reduces stroke and heart failure risk when paired with beta-blockers, with far fewer dangerous side effects than verapamil or diltiazem.
What are the signs that this combo is too strong for me?
Watch for a pulse below 50 bpm, dizziness, fainting, extreme fatigue, chest pain, or swelling in your ankles and legs. If your PR interval on an ECG is over 200 milliseconds, that’s a red flag. Any of these symptoms mean you need to contact your doctor immediately-don’t wait.
Why is verapamil dangerous with beta-blockers?
Verapamil slows the heart’s electrical system and reduces pumping force. Beta-blockers do the same. Together, they can cause severe bradycardia, heart block, or even cardiac arrest. Studies show 10-15% of patients on this combo develop dangerous heart rhythm problems. The FDA has issued a boxed warning for this reason.
Do I need blood tests before starting this combo?
You don’t need routine blood tests, but you absolutely need an ECG and an echocardiogram. These aren’t optional-they’re essential. The ECG checks your heart’s electrical timing, and the echo measures how well your heart pumps. Skipping these increases your risk of serious complications.
Can I switch from verapamil to amlodipine if I’m on a beta-blocker?
Yes, and it’s often recommended if you’re experiencing side effects. But don’t switch on your own. Your doctor will gradually reduce the verapamil while introducing amlodipine, monitoring your heart rate and blood pressure closely. This transition needs supervision to avoid sudden drops in blood pressure or rebound angina.
What Comes Next?
If you’re on this combo, keep track of your symptoms. Use a simple notebook or phone app to log your morning heart rate and blood pressure. Share it with your doctor at every visit. If you’re not on it yet but your doctor suggests it, ask: "Which calcium channel blocker are you prescribing? Why this one? Have you checked my ECG and heart function?" If they haven’t done those tests, push back. Your heart isn’t a gamble.
The future of heart medication isn’t about piling on more drugs. It’s about matching the right drugs to the right people. Beta-blockers and calcium channel blockers can be powerful allies-but only if you understand the rules. And in this case, the rules aren’t suggestions. They’re lifesavers.
Write a comment
Items marked with * are required.





14 Comments
Matt Dean December 1, 2025 AT 19:36
This combo is a ticking time bomb if your doctor isn't paying attention. I've seen too many elderly patients get prescribed verapamil with metoprolol and end up in the ER with a pulse of 38. No one checks their PR interval anymore. It's like prescribing insulin without checking blood sugar first.
Kay Lam December 2, 2025 AT 10:27
I've been managing hypertension for over a decade and this is the first time I've seen someone lay out the real risks of this combination so clearly. Most doctors just say 'take these two pills' and move on. The distinction between dihydropyridines and non-dihydropyridines is critical and almost never explained. Amlodipine is fine with beta-blockers, but verapamil? That's like stacking two anchors on your heart. I'm going to ask my cardiologist for my last ECG before my next refill. If they haven't checked it, I'm not taking it.
And yes, ankle swelling from amlodipine is annoying, but it's a small price compared to sudden cardiac arrest. I'd rather have puffy ankles than a pacemaker.
Also, the 15% of people over 75 with undiagnosed conduction issues? That number haunts me. We're not talking about rare edge cases here. We're talking about a silent epidemic. Why isn't every primary care doctor running an ECG before prescribing this combo? Insurance won't cover it? That's not an excuse. It's malpractice waiting to happen.
I've had patients who thought 'it's just a slow heart rate' until they fainted while walking to the mailbox. That's not aging. That's iatrogenic harm. We need mandatory ECG protocols for this combination. Period.
And the FDA warning? It's not enough. We need public awareness campaigns. This isn't just a medical issue-it's a public health failure. People deserve to know what they're swallowing.
Thank you for writing this. It's the kind of post that makes me feel like I'm not crazy for asking questions.
Louise Girvan December 3, 2025 AT 13:12
They're hiding the truth. Big Pharma doesn't want you to know how dangerous this combo is. Look at the stats-10-15% heart block? That's not a side effect, that's a massacre. And they're still prescribing it? Who profits? Who's getting paid? Someone's making millions off these dead bodies.
Walker Alvey December 3, 2025 AT 17:30
Wow. Someone actually read the guidelines. How quaint. I thought we'd all just be taking whatever the rep handed us with a free coffee mug and a smile. Next you'll tell me we should wash our hands before surgery.
Declan Flynn Fitness December 4, 2025 AT 16:29
Good post. I'm a physio in Dublin and I see patients on this combo all the time. Amlodipine + beta-blocker? Usually fine. Verapamil + beta-blocker? Red flag. I always tell them: if you feel like you're about to pass out when you stand up, stop and call your doc. No shame. Better safe than sorry. And yeah, ankle swelling sucks-but it's not life-threatening. Heart block is. Stay sharp.
Michelle Smyth December 5, 2025 AT 14:03
How pedestrian. You're reducing a complex pharmacodynamic interaction to a binary of 'safe' and 'dangerous.' The reality is far more nuanced-dose-response curves, genetic polymorphisms in CYP3A4, renal clearance variations, and epigenetic modulation of calcium channel expression all play a role. Your ECG-centric approach is reductive and ignores the biopsychosocial framework of modern cardiology.
Declan O Reilly December 6, 2025 AT 00:50
Man I just got prescribed amlodipine with metoprolol last week and I was worried as hell. This post literally saved me from quitting my meds. I've been checking my pulse every morning and my BP with my home monitor. 62 bpm, 128/82. Felt like a champ. Also, the ankle swelling? Yeah, it's there-but I just elevate my legs while watching Netflix. No biggie. Thanks for the real talk.
Grant Hurley December 6, 2025 AT 10:01
So if I'm on amlodipine and metoprolol and my legs are puffing up, is that normal? I thought I was just getting old. Also, should I be worried if my heart rate drops to 55 at night?
patrick sui December 6, 2025 AT 11:06
Great breakdown. One thing I'd add: even with amlodipine, if you're over 70 and have borderline conduction issues, start at half-dose. I've seen patients on 5mg amlodipine + 25mg metoprolol and still get dizziness. Slow titration is non-negotiable. Also, check potassium levels-hypokalemia can worsen conduction delays. Not always in the ECG, but it's a silent amplifier of risk.
And for those asking about ankle swelling-compression socks help. Not magic, but they reduce the edema by 40-60% in most cases. Also, avoid standing for long periods. Your veins aren't what they used to be.
Thanks for highlighting the ECG. Too many docs skip it because 'it's just a routine script.' But routine doesn't mean risk-free.
Adrian Barnes December 8, 2025 AT 10:05
The assertion that amlodipine is 'safe' in combination with beta-blockers is empirically unsound. While it is true that dihydropyridines exert less negative inotropic effect, the cumulative reduction in cardiac output, particularly in the context of age-related arterial stiffness and diminished baroreceptor sensitivity, creates a physiological vulnerability that is neither quantified nor acknowledged in this discourse. The statistical reduction in stroke risk is confounded by increased incidence of orthostatic hypotension and falls, which are underreported in clinical trials. The notion that 'watching your pulse' constitutes adequate monitoring is a dangerous oversimplification of autonomic dysregulation in the elderly. This is not medicine. It is algorithmic triage disguised as clinical guidance.
Patrick Smyth December 9, 2025 AT 04:47
My uncle died from this. They gave him verapamil and metoprolol. He was 78. He didn't even know he had a slow heart. One morning he just didn't wake up. The coroner said complete heart block. No warning. No ECG. No echo. Just pills. I'm still mad. Don't let this happen to you.
Dennis Jesuyon Balogun December 9, 2025 AT 12:09
As a Nigerian cardiologist working in Lagos, I can tell you this is not just a Western problem. We see this every day. Patients come in with dizziness after starting verapamil + metoprolol. No ECG. No history. Just 'doctor gave me these.' We're training more nurses to do basic ECGs in clinics. We're pushing for policy change. This isn't just about drugs-it's about access to diagnostics. You can't manage what you can't measure.
And yes, amlodipine is our go-to. Cheap, effective, safer. But we still need better screening. We need more machines. We need more training. This post? It's the same battle we're fighting here.
Conor Forde December 10, 2025 AT 01:22
Oh wow. So now we're supposed to be scared of amlodipine? Next you'll tell me oxygen is dangerous because some people died from it. This post is basically a fear-mongering pamphlet from 1987. People are living longer, not dying from pills. My grandma's on this combo and she hikes 5K every weekend. She's 84. Your 'danger' is just your anxiety dressed up as science.
Matt Dean December 10, 2025 AT 03:37
@5367 Your grandma’s hiking 5K? That’s great. But she’s the exception, not the rule. Most people on this combo aren’t hiking-they’re sitting on the toilet because they’re dizzy. And if she’s on verapamil, she’s lucky. If she’s on diltiazem? She’s one missed ECG away from a pacemaker. Don’t turn anecdote into protocol.