
Health November 26, 2025
Muscle Aches from Statins: What Really Happens and What to Do Next
Statin Muscle Pain Risk Assessment Tool
Personal Risk Assessment
Answer a few simple questions to estimate your risk of developing muscle pain while taking statins.
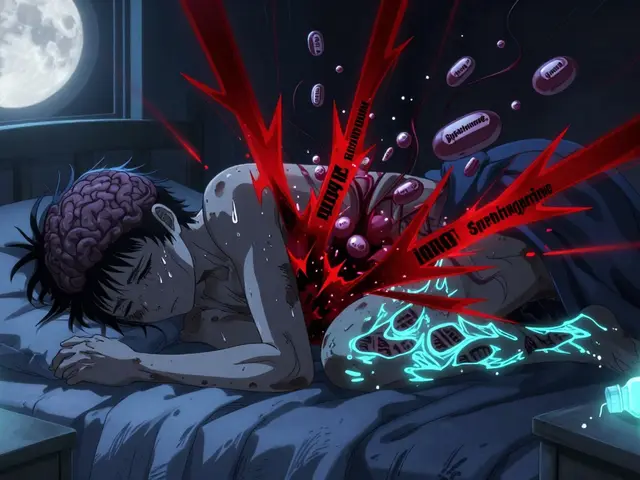
Millions of people take statins every year to lower their cholesterol and protect their heart. But for a lot of them, the side effect they notice first isn’t a lab result-it’s muscle aches. It starts as a dull soreness in the thighs or calves. Then it becomes stiffness when you get out of bed. Soon, walking up the stairs feels like a chore. You might even start wondering if the medicine is doing more harm than good.
The truth is, muscle pain from statins is real-but it’s also often misunderstood. Many people assume their aches are definitely caused by the drug. But the science says something more complicated. About 5% to 10% of people on statins have muscle symptoms that are truly linked to the medication. The rest? Their pain might be from aging, inactivity, another health issue, or even the way they’ve been told to expect side effects. That’s called the nocebo effect-and it’s powerful.
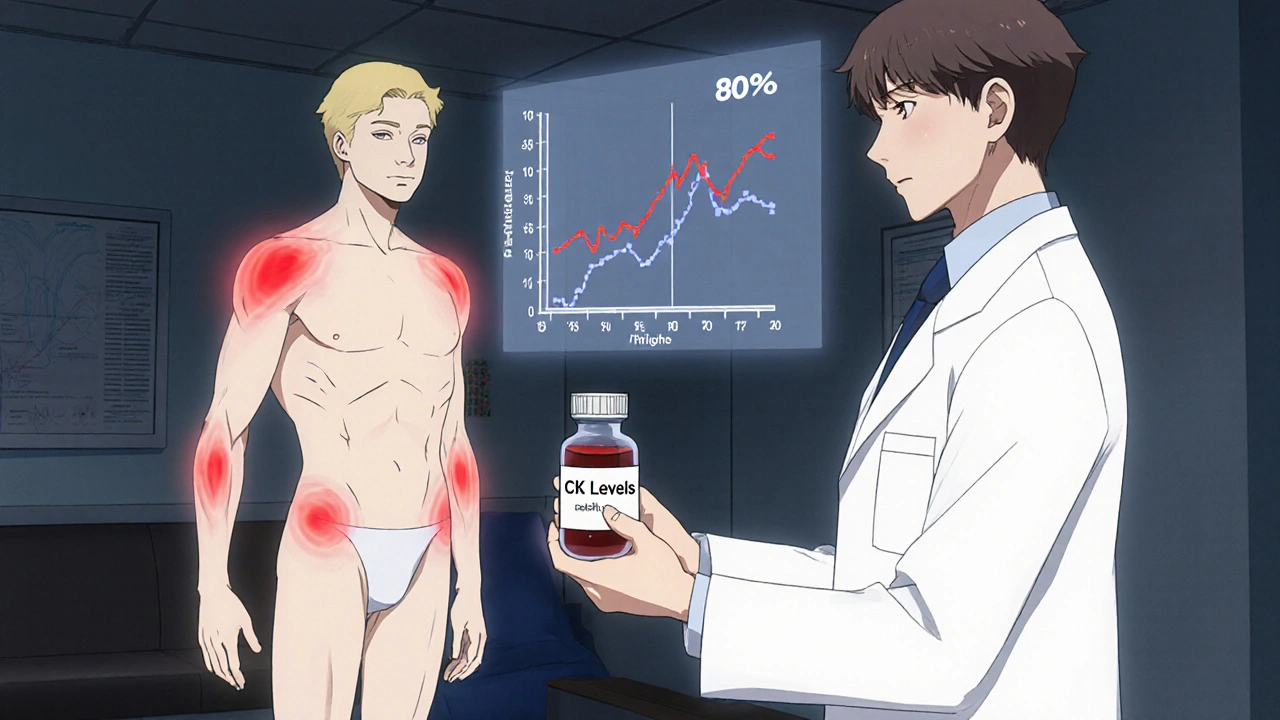
What Does Statin-Related Muscle Pain Actually Feel Like?
Statin-induced muscle discomfort doesn’t usually feel like a pulled muscle or a sports injury. It’s not sharp or localized. Instead, it’s a deep, constant soreness or weakness that shows up on both sides of your body at once. You’ll feel it most often in your shoulders, thighs, hips, or calves. It doesn’t come and go with movement. It’s there when you’re resting too. Some people describe it as feeling like they’ve run a marathon without ever leaving the house.
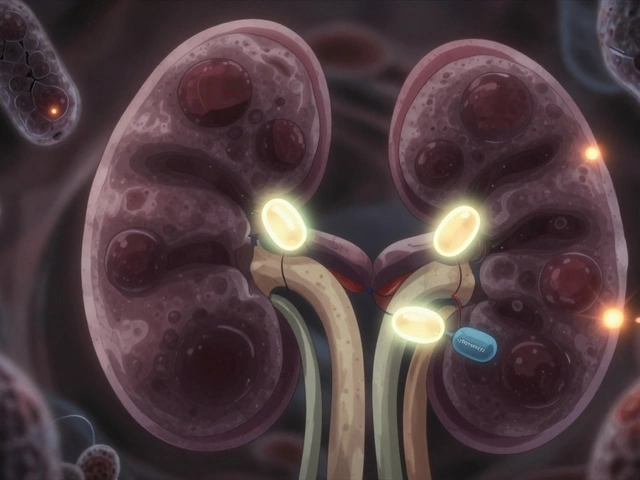
There’s a spectrum. Most cases are mild-just annoying. But in rare cases, it can turn serious. Myositis means inflammation of the muscle tissue. Rhabdomyolysis is the extreme version: muscle cells break down so badly they leak into your bloodstream, which can damage your kidneys. That’s extremely rare-about 3 to 5 cases per million statin prescriptions. But it’s why you should never ignore severe pain, dark urine, or extreme weakness.
Why Do Some People Get It and Others Don’t?
Not everyone on statins gets muscle pain. And it’s not random. Certain factors make it more likely:
- Age: People over 80 are about 30% more likely to experience muscle symptoms.
- Body size: Smaller individuals, especially women under 100 lbs, have higher risk.
- Gender: Women report muscle pain more often than men-partly because they’re often older when they start statins, have more other health conditions, and are more likely to have undiagnosed hypothyroidism, which doubles the risk.
- Other meds: Taking statins with drugs like fibrates, cyclosporine, or certain antibiotics (like erythromycin) increases muscle side effects.
- Health conditions: Kidney disease, liver problems, or an underactive thyroid can make your body process statins differently, raising your risk.
- Dosage: High-intensity statins (like 80 mg atorvastatin or 40 mg rosuvastatin) carry about 15% more risk than moderate doses.
One big surprise? The type of statin matters. Some, like pravastatin and fluvastatin, are much less likely to cause muscle pain than others. If you’ve had trouble with one statin, switching to another might solve the problem-about 60% of people find relief this way.
Is It Really the Statin? The Rechallenge Test
This is where things get tricky. In clinical trials, people who took a sugar pill (placebo) reported muscle pain at almost the same rate as those taking statins. Why? Because they were told muscle pain was a possible side effect. That’s the nocebo effect in action.
Here’s what doctors know from real-world testing: Only about 20% to 25% of people who think their muscle pain is from statins actually get it back when they take the same drug again under controlled conditions. That means most people who quit statins over muscle pain might not have needed to.
That’s why the gold standard for diagnosis is the rechallenge test. If you’re having symptoms:
- Your doctor checks your creatine kinase (CK) levels. If they’re more than 10 times the normal limit, stop the statin immediately.
- If CK is normal or only slightly high, you stop the statin for 4 to 6 weeks.
- If your pain goes away, you restart the same statin at a lower dose.
- If the pain comes back, it’s likely the statin.
- If it doesn’t, the pain was probably something else.
This isn’t always done in busy clinics-but it’s the only way to know for sure. Don’t assume your pain is from statins unless it’s confirmed.
What to Do If You’re Having Muscle Pain
If you’re experiencing muscle aches and you’re on a statin, don’t just quit. Stopping without medical guidance can raise your risk of heart attack or stroke by 25% to 50% within two years. Instead, follow these steps:
- Call your doctor. Don’t wait. Describe exactly where the pain is, how long it’s lasted, and whether it’s getting worse.
- Get a CK blood test. This checks for muscle damage. Normal levels don’t rule out discomfort, but high levels mean you need to stop the statin.
- Ask about switching statins. Pravastatin or fluvastatin are gentler on muscles. Rosuvastatin and atorvastatin are stronger but also more likely to cause issues.
- Try a lower dose. Sometimes half a tablet is enough to keep your cholesterol in check without the pain.
- Consider a statin holiday. Stop for 4 to 6 weeks. If your muscles feel better, you can try restarting at a lower dose.
Some people try coenzyme Q10 supplements, hoping it helps. The science is mixed. A 2015 review found no real benefit over placebo. But a 2018 study showed 30% of people who took it reported less pain. It’s not a cure, but if your doctor says it’s safe, it might be worth a try.
What If You Can’t Tolerate Any Statin?
Some people truly can’t take statins-even at low doses, even after switching. That’s when alternatives come in.
- Ezetimibe: This pill blocks cholesterol absorption in the gut. It’s not as powerful as statins, but it lowers LDL by about 15-20%. It’s cheap-generic versions cost under $10 a month.
- PCSK9 inhibitors: These are injectables (alirocumab, evolocumab) that slash LDL by 50-60%. They’re very effective but cost about $5,000 a year. Most insurance covers them only if you’ve tried everything else.
- Lifestyle changes: Diet, exercise, weight loss, and quitting smoking can lower LDL by 20-30% on their own. That’s not a replacement for medication in high-risk patients-but it helps.
Here’s the hard truth: For most people, the benefits of statins far outweigh the risks. A 2023 analysis of 21 studies showed that for every 1 mmol/L drop in LDL cholesterol, major heart events drop by 29%. That’s huge. If you’ve had a heart attack, stroke, or have diabetes, skipping statins because of muscle pain could cost you your life.

Don’t Give Up-There’s a Way Forward
Statin muscle pain is frustrating. It’s real for some, exaggerated for others. But it’s not a dead end. With the right approach, 80% to 90% of people who report muscle symptoms can get back on statins safely.
Work with your doctor. Get the right tests. Try different statins. Lower the dose. Be patient. Your heart is worth it. You don’t have to live with pain-or risk a heart attack.
Can statins cause permanent muscle damage?
No, statins don’t cause permanent muscle damage in the vast majority of cases. Muscle pain and weakness usually go away within days or weeks after stopping the medication. The only exception is rhabdomyolysis, which is extremely rare and requires immediate medical care. Even in those cases, most patients recover fully with proper treatment.
Is it safe to take CoQ10 with statins?
Yes, CoQ10 is generally safe to take with statins. Some people report less muscle discomfort when using it, but studies haven’t proven it works consistently. It’s not a substitute for medical advice, but if your doctor approves, it’s low-risk and might help you feel better while you figure out the best treatment plan.
Why do women report more muscle pain from statins than men?
Women are more likely to report muscle pain from statins because they often start taking them at an older age, tend to have smaller body sizes, and are more likely to have other conditions like hypothyroidism, which increases side effect risk. They also report symptoms more openly than men, which may play a role in the data.
Can I just stop taking statins if my muscles hurt?
No. Stopping statins without medical supervision increases your risk of heart attack or stroke by 25% to 50% within two years. Always talk to your doctor first. They can help you figure out if the pain is really from the statin-and how to manage it safely.
Are there natural ways to lower cholesterol without statins?
Yes, diet, exercise, weight loss, and quitting smoking can lower LDL cholesterol by 20% to 30%. But for people with high cardiovascular risk-like those with diabetes, past heart disease, or very high LDL-these changes alone aren’t enough. Statins reduce risk by 25% to 35%. Natural methods help, but they don’t replace medication when it’s medically needed.
What Comes Next?
If you’re struggling with muscle pain and statins, the next step is simple: schedule a chat with your doctor. Bring your symptoms, your concerns, and your questions. Ask about your CK levels. Ask about switching statins. Ask about alternatives. Don’t let fear or frustration lead you to quit without a plan.
Statins save lives. But they shouldn’t make you miserable. With the right strategy, you can have both: a healthy heart and pain-free muscles.
Write a comment
Items marked with * are required.


12 Comments
Asha Jijen November 27, 2025 AT 09:12
statins are just big pharma’s way of making money off scared people
my grandma took them for 10 years and still had a heart attack
why not just eat less bread and walk more
Emma louise November 27, 2025 AT 11:29
Oh wow another ‘trust your doctor’ sermon from the medical industrial complex
let me guess you also think fluoride in water is ‘safe’ and 5G isn’t spying on you
my cousin’s legs turned to jelly on statins and they told him it was ‘aging’
yeah right
they don’t want you to know the truth because pills are more profitable than lifestyle changes
Allison Turner November 29, 2025 AT 10:02
people who take statins are just lazy
if you can’t control your cholesterol with kale and willpower then you’re not trying
also why are you even on the internet if you can’t even walk up stairs
just quit already
Savakrit Singh November 30, 2025 AT 09:10
Based on the meta-analysis of 21 studies referenced, the risk-benefit ratio of statin therapy remains overwhelmingly favorable for primary and secondary prevention populations, particularly when LDL-C reduction exceeds 1.0 mmol/L. The incidence of myopathy is dose-dependent and correlates with pharmacokinetic variables including CYP3A4 metabolism and body mass index. Furthermore, the nocebo effect, as demonstrated in placebo-controlled trials, accounts for approximately 70% of self-reported myalgia. Therefore, clinical decision-making must be individualized, incorporating genetic screening (e.g., SLCO1B1 polymorphism), CK monitoring, and therapeutic rechallenge protocols. Failure to implement evidence-based diagnostics constitutes substandard care.
Jebari Lewis November 30, 2025 AT 12:32
you guys are missing the point
statins work
they save lives
my uncle had a stent at 52 and lived to 78 because of them
if you’re too scared to take a pill that lowers your risk by 30% then maybe you shouldn’t be driving a car either
the real danger is ignoring science because you read a blog post
get your numbers checked
don’t be a statistic
Aishwarya Sivaraj December 1, 2025 AT 11:41
i had muscle pain too and thought it was the statin
turned out i was dehydrated and had low vitamin d
after fixing those it went away
also switched to pravastatin and no issues since
don’t assume it’s the drug
check everything else first
your body is trying to tell you something
listen
Cecily Bogsprocket December 1, 2025 AT 18:17
it’s so easy to say ‘just take the pill’ when you’ve never felt like your legs are made of concrete
but for those of us who wake up and can’t lift our arms without groaning
it’s not just inconvenience
it’s losing pieces of yourself
the real tragedy isn’t the statin
it’s that we’re told to suffer silently because ‘the numbers say it’s worth it’
what if the numbers don’t include your quality of life
what if your heart is safe but your soul is tired
maybe the answer isn’t just more pills
maybe it’s more listening
Darrel Smith December 1, 2025 AT 23:24
if you’re complaining about muscle pain from statins you’re probably the same person who eats fast food every day and then wonders why you’re sick
you want the benefits without the responsibility
statins are not a magic bullet
but they’re one of the few tools we have that actually works
you want to live longer
then you have to make hard choices
no one said being healthy would be easy
but it’s better than the alternative
and if you’re not willing to try
then don’t be surprised when your kids are burying you at 60
Iives Perl December 2, 2025 AT 08:54
they’re watching your CK levels
they’re tracking your heart rate
they know when you skip your pill
they’re using this to build a health profile
next they’ll tell you when to breathe
don’t be fooled
it’s not about your heart
it’s about control
steve stofelano, jr. December 2, 2025 AT 12:19
as someone who grew up in a household where medicine was viewed with deep skepticism, I have come to appreciate the rigor of modern clinical guidelines. The data supporting statin use in cardiovascular risk reduction is among the most robust in all of medicine. That said, I recognize that individual experiences vary, and the psychological burden of perceived side effects is real. I encourage all patients to engage in collaborative dialogue with their physicians-not as adversaries, but as partners in health.
Lauren Zableckis December 2, 2025 AT 15:11
my mom was on statins for 15 years, never had pain, lived to 92
my dad quit because he thought it was ‘poison’
he had a stroke at 71
so yeah
talk to your doctor
not reddit
Alex Hess December 4, 2025 AT 11:49
you people are ridiculous
you think a 200-page medical article means anything
the real truth is that doctors don’t know anything
they just read what the drug companies pay them to believe
if statins were so great, why are people still dropping dead at 55?
it’s all a scam
and you’re all sheep