Health November 19, 2025
Questions to Ask Your Pharmacist About Potential Drug Interactions
Why Drug Interactions Matter More Than You Think
Every year, over 1.3 million people in the U.S. end up in the emergency room because of drug interactions. That’s not a small number-it’s a preventable crisis. You might be taking your blood pressure pill, your cholesterol medicine, and a daily vitamin, but you don’t know if they’re working together-or fighting each other. A pharmacist isn’t just the person who hands you your prescription. They’re your safety net. And asking the right questions can stop a dangerous reaction before it starts.
What Exactly Is a Drug Interaction?
A drug interaction happens when something changes how a medicine works in your body. It could be another pill, a food, a supplement, or even a drink like grapefruit juice. These aren’t just minor annoyances. They can make your medicine less effective, cause bad side effects, or even lead to serious health problems like internal bleeding, heart rhythm issues, or dangerously high blood pressure.
There are three main types:
- Drug-drug interactions: Two or more medications react. For example, taking warfarin with certain antibiotics can increase your risk of bleeding.
- Drug-food/beverage interactions: Food or drinks interfere. Grapefruit juice can stop your body from breaking down statins, causing toxic levels to build up.
- Drug-condition interactions: Your health condition makes a drug risky. Decongestants like pseudoephedrine can spike blood pressure in people with hypertension.
What to Ask Your Pharmacist-The Essential Questions
Don’t wait until you feel sick. Bring your list and ask these questions every time you pick up a new prescription or add a supplement.
- Can this medicine interact with anything else I’m taking? This includes prescription drugs, over-the-counter pills, herbal supplements, and even vitamins. Many people forget that something like St. John’s wort or fish oil can interfere with antidepressants or blood thinners.
- Should I avoid certain foods, drinks, or products? Grapefruit juice is the most common culprit, but it’s not the only one. If you’re on a blood thinner like warfarin, leafy greens high in vitamin K can reduce its effect. Alcohol can worsen drowsiness with painkillers or anxiety meds. Ask specifically about your diet.
- What are the warning signs I should watch for? Don’t just take the medicine and hope for the best. Know what to look for: unusual bruising, dizziness, rapid heartbeat, nausea, confusion, or swelling. These could mean your body is reacting badly.
- How should I take this with food or other meds? Some drugs need to be taken on an empty stomach. Others work better with food. Timing matters. Taking your thyroid pill with calcium or iron supplements can block absorption. Ask if you should space them out.
- Does this medicine affect my existing health conditions? If you have kidney disease, liver problems, diabetes, or heart failure, some drugs can make those worse. A common example: NSAIDs like ibuprofen can raise blood pressure and strain kidneys, especially in older adults.
- Is there a safer alternative if this one has too many risks? Sometimes there’s another option with fewer interactions. Your pharmacist can check if a different brand or class of drug would work just as well without the danger.
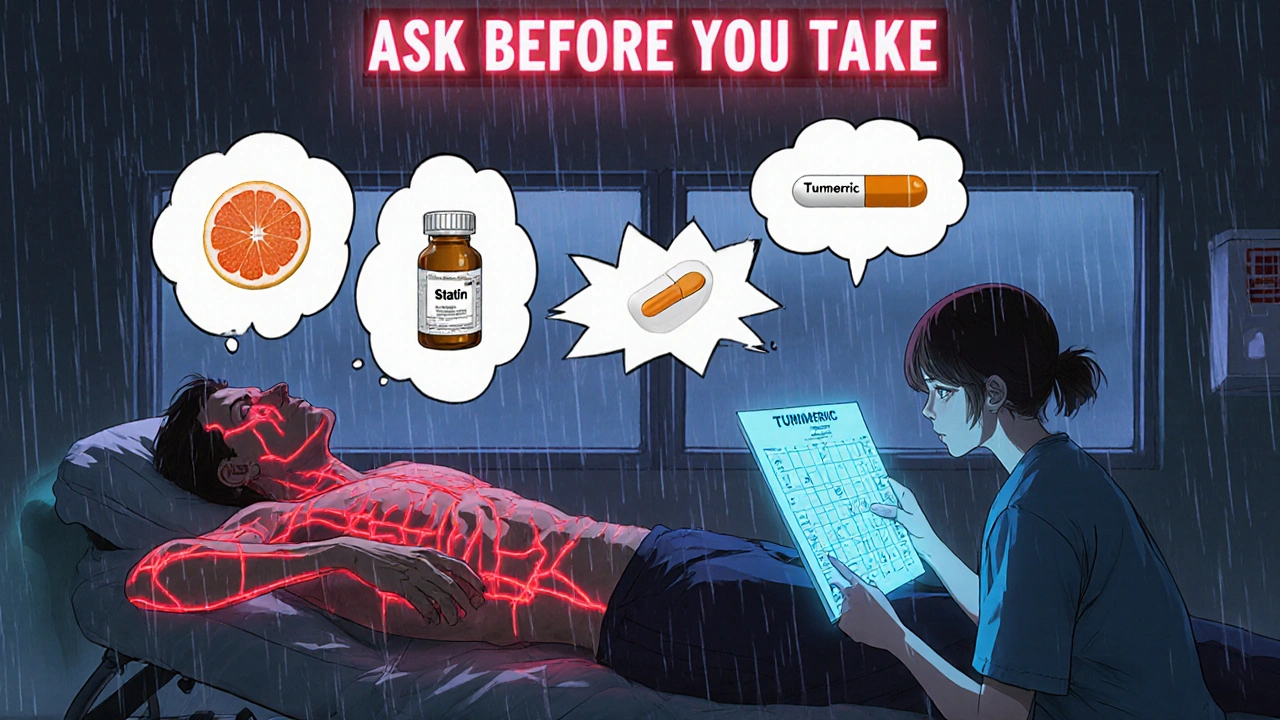
- Do I need to tell you about my supplements? Yes. Seriously. Over 77% of U.S. adults take supplements, and most don’t realize they can interact. Turmeric, ginkgo, garlic pills-they all have blood-thinning effects. Even magnesium can interfere with antibiotics.
How to Prepare Before Your Visit
Pharmacists can’t help if they don’t have the full picture. Bring this with you:
- A written list of every medication: name, dose, and how often you take it. Don’t rely on memory.
- All your supplements and vitamins, even if you think they’re harmless. Bring the bottles.
- Your current diet habits: Do you drink grapefruit juice daily? Eat a lot of cheese? Drink alcohol regularly?
- Your medical history: Especially heart disease, liver or kidney issues, diabetes, or allergies.
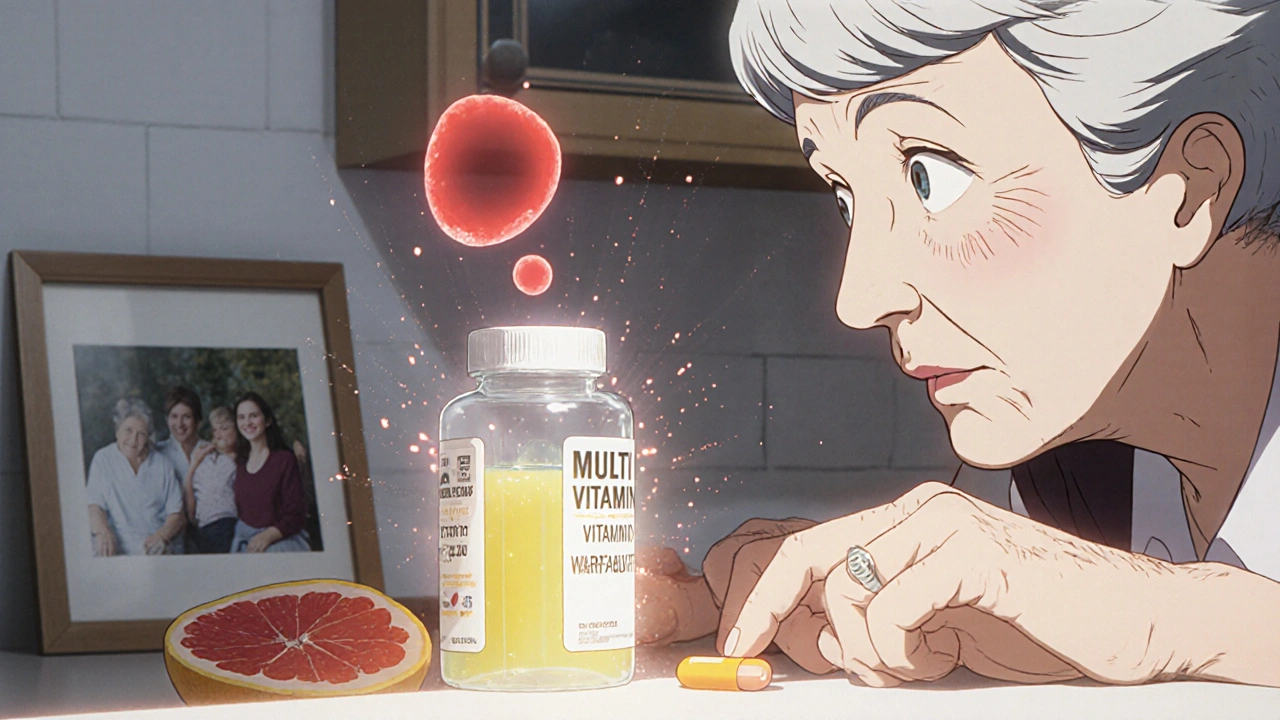
Many people think, “I only take one thing.” But if you’re over 65, you’re likely on five or more medications. The National Center for Health Statistics says 57% of women in that age group take five or more daily. That’s a recipe for hidden risks.
Why Pharmacists Are Your Best Defense
Pharmacists are trained to spot interactions that doctors might miss. Why? Because they see your full medication list-not just the latest prescription. They use systems that flag risks in real time, like CYP450 enzyme conflicts. For example, if you’re on Camzyos (mavacamten), taking St. John’s wort or rifampin can cause dangerous drops in blood pressure.
Studies show that when pharmacists do full medication reviews, drug interaction incidents drop by nearly 24% in Medicare patients. That’s not a small win. That’s life-saving work.
And it’s not just about pills. The FDA requires interaction warnings on every prescription label since 2006. But labels are hard to read. Pharmacists explain them in plain language. They know what matters for you.
What Happens When You Don’t Ask
In 2022, over 112,000 adverse events in the U.S. were linked to drug interactions. Most involved blood thinners, diabetes meds, and heart drugs. These weren’t rare cases. They were preventable.
One real example: A 72-year-old man took simvastatin (a cholesterol drug) with grapefruit juice every morning. He didn’t know it could cause muscle damage. He ended up in the hospital with rhabdomyolysis-a condition where muscle breaks down and floods the kidneys. He survived, but he could have avoided it with one question.
Another: A woman on warfarin started taking a new multivitamin with vitamin K. Her INR dropped. She didn’t know why she started clotting. Her pharmacist caught it during a routine check-up.
What’s Changing in Drug Safety
Technology is helping. CVS and Walgreens now use electronic systems that flag interactions in real time. But here’s the catch: those systems only work if your full medication list is entered. If you forget to mention your turmeric capsules or your neighbor’s leftover antibiotics, the system won’t catch it.
Future tools are even smarter. The FDA approved the first pharmacogenetic test for warfarin dosing in 2021. This looks at your genes to predict how you’ll process certain drugs. In a few years, your pharmacist might know your interaction risk before you even walk in.
But for now, the best tool is still you-asking the right questions.
When to Talk to Your Pharmacist
Don’t wait for a crisis. Talk to your pharmacist:
- Every time you get a new prescription
- When you start or stop a supplement
- After a hospital stay or doctor visit
- At least once every three months, even if nothing changed
The most recent drug added is often the one causing the problem. That’s why regular check-ins matter.
Final Thought: Your Health Is Your Responsibility
You wouldn’t drive a car without checking the oil. Why take medicine without checking for risks? Pharmacists are trained to help you. But they need you to speak up. Write down your questions. Bring your list. Don’t assume it’s fine. A simple conversation can prevent a hospital visit-or worse.
Can I take my supplements with my prescription drugs?
Not always. Many supplements can interfere with medications. For example, St. John’s wort can reduce the effectiveness of birth control pills, antidepressants, and blood thinners. Turmeric and garlic can increase bleeding risk when taken with warfarin. Always list every supplement you take-even if you think it’s "natural" or "safe." Your pharmacist can check for hidden risks.
Does grapefruit juice really interact with all my meds?
No, but it interacts with many common ones. Statins like simvastatin and atorvastatin, blood pressure drugs like felodipine, and some anti-anxiety medications like buspirone can all be affected. Grapefruit blocks an enzyme in your gut that breaks down these drugs, causing too much to build up in your blood. Even one glass a day can be risky. Ask your pharmacist if your meds are on the list.
Can I just skip a dose if I’m worried about an interaction?
Don’t skip doses on your own. Stopping a medicine suddenly can be dangerous. For example, stopping blood pressure or antidepressant meds abruptly can cause rebound effects like high blood pressure or severe anxiety. Instead, call your pharmacist. They can advise if it’s safe to pause, adjust timing, or switch to a different option.
Do over-the-counter cold medicines interact with my prescriptions?
Yes, often. Decongestants like pseudoephedrine can raise blood pressure-dangerous if you have hypertension. Antihistamines like diphenhydramine can cause drowsiness or confusion, especially when combined with sleep aids or painkillers. Even cough syrups with dextromethorphan can interact with antidepressants. Always check with your pharmacist before taking OTC meds.
Why does my pharmacist ask about my diet?
Because food changes how drugs work. Vitamin K in spinach and kale can make warfarin less effective. High-sodium foods can worsen blood pressure meds. Alcohol can increase liver damage from acetaminophen. Your pharmacist needs to know what you eat to give you accurate advice. It’s not just about pills-it’s about your whole lifestyle.
What if I’m taking more than five medications?
You’re at higher risk. People taking five or more drugs have a 100% chance of at least one potential interaction, according to research. That’s why regular medication reviews with your pharmacist are essential. They can spot redundancies, unnecessary drugs, or dangerous combinations you might not notice. Don’t wait until something goes wrong-schedule a review now.
Write a comment
Items marked with * are required.




9 Comments
Ron and Gill Day November 21, 2025 AT 02:31
Wow, another ‘ask your pharmacist’ PSA. So helpful. I’m sure the 1.3 million ER visits last year were all because people didn’t read the tiny print on the bottle. Meanwhile, my pharmacist still can’t tell me why my prescription costs $400 but the guy at the gas station sells the same pill for $12. 🤡
Alyssa Torres November 22, 2025 AT 17:17
THIS. I had no idea grapefruit juice could mess with my blood pressure med until my pharmacist pulled me aside last month. I used to drink it every morning like it was water. Now I drink orange juice and feel like a wellness warrior. 🙌 Your pharmacist is literally your health superhero-don’t be shy. Bring your supplements. Bring your questions. Bring your weird food habits. They’ve seen it all.
Summer Joy November 24, 2025 AT 09:19
OMG I just realized I’ve been taking turmeric with my blood thinner for 3 years 😭 I’m literally one step away from a stroke. Why didn’t anyone tell me? My pharmacist probably thinks I’m a walking medical disaster. I’m gonna go cry in the aisle next to the probiotics. 🥲💊 #PharmacistTherapy
Aruna Urban Planner November 25, 2025 AT 01:11
The pharmacogenetic testing mentioned is a significant step forward in personalized pharmacotherapy. However, its scalability remains constrained by socioeconomic and infrastructural disparities. The CYP450 enzyme profiling, while clinically validated, is not universally accessible. Until systemic equity in pharmaceutical care is addressed, the burden of risk mitigation continues to fall disproportionately on the individual.
Nicole Ziegler November 26, 2025 AT 18:08
I just took a photo of all my meds + supplements and sent it to my pharmacist. She replied within 10 mins with a color-coded chart. Like... I cried. 🥺💊 #PharmacistIsMyHero
Bharat Alasandi November 28, 2025 AT 03:48
Bro I’m 68 and on 7 meds. My pharmacist knows my meds better than my daughter. Last week she caught that my calcium supplement was blocking my thyroid pill. I was taking them together for years. She gave me a little schedule card. Now I’m like a clock. 🕒💯
Kristi Bennardo November 29, 2025 AT 16:21
This article is dangerously naive. Pharmacists are not medical doctors. They are not qualified to override prescribing decisions or independently assess polypharmacy risk without clinical oversight. Relying on them as a ‘safety net’ is a regulatory failure. The real issue is fragmented electronic health records and physician oversight gaps-not patient ignorance.
Shiv Karan Singh November 30, 2025 AT 02:36
LMAO. So you want us to trust the same people who gave us OxyContin in the 90s? 😂 And now they’re our ‘safety net’? My pharmacist once told me to ‘take it with food’ when I asked about the liver damage warning. He didn’t even look at my bloodwork. These people are glorified cashiers. Don’t be fooled.
Ravi boy December 1, 2025 AT 16:37
yep i just asked my pharma guy about my fish oil and blood thinners he said oh yeah that aint good but dont worry its prob fine 🤷♂️ but i brought my whole bottle list next time and he actually looked at it. good people out there just gotta ask