Health November 21, 2025
Common Cold vs Flu: Symptoms, Risks, and When Antivirals Actually Help
What’s the Real Difference Between a Cold and the Flu?
You wake up with a sore throat, a stuffy nose, and a headache. Is it just a cold-or could it be the flu? It’s a question millions ask every fall and winter. The truth is, common cold and influenza feel similar at first, but they’re not the same illness. One might leave you feeling lousy for a week. The other can land you in the hospital-or worse.
Rhinoviruses cause most colds. There are over 160 types, which is why you keep getting them. Flu? That’s always influenza virus-types A or B. These aren’t just different bugs. They behave differently, hit harder, and demand different responses.
How Symptoms Start and Progress
With a cold, things creep up. You might feel a tickle in your throat on Monday. By Wednesday, your nose is running, your ears feel plugged, and you’re sneezing nonstop. Fever? Rare in adults-only 15-20% get even a low-grade one. Most colds fade in 7 to 10 days. Sometimes they drag on to two weeks, but you’re usually not bedridden.
Flu hits like a truck. One minute you’re fine. The next, you’re shivering, aching, and burning up. Fever hits fast-often above 102°F. Muscle pain is severe. Headaches are pounding. Fatigue doesn’t just make you tired-it crushes you. People say they feel like they’ve been hit by a bus. And it doesn’t just go away in a few days. Exhaustion can last two to three weeks.
Here’s the kicker: extreme tiredness? That’s never part of a cold. Chest tightness? Common in flu, rare in colds. If you’re dizzy, weak, and can’t get out of bed, it’s not a cold. It’s flu.
When a Cold or Flu Turns Dangerous
Colds rarely cause serious problems. Maybe you get a sinus infection-about 5% of cases. Kids might get ear infections. That’s it.
Flu? That’s where things get scary. About 15-30% of people hospitalized with flu develop pneumonia. In 2023, the CDC estimated 140,000 to 710,000 flu hospitalizations in the U.S. alone. Between 12,000 and 52,000 people died from flu each year between 2010 and 2020. That’s not a number you ignore.
Who’s most at risk? People over 65. They make up 70-85% of flu deaths. Pregnant women are three times more likely to be hospitalized. People with asthma, diabetes, or weakened immune systems are also in danger. Even healthy young adults can get severely ill. Don’t assume you’re safe just because you’re young.

Antivirals for Flu-What Works and When
There are four FDA-approved antivirals for flu: oseltamivir (Tamiflu), zanamivir (Relenza), peramivir (Rapivab), and baloxavir (Xofluza). None of them work for colds. That’s critical. Taking antivirals for a cold is useless-and a waste of money.
These drugs target the flu virus’s ability to spread. Oseltamivir and zanamivir block neuraminidase. Baloxavir shuts down viral replication at the source. When taken within 48 hours of symptoms starting, they can cut illness duration by 1 to 2 days. For high-risk people, they can cut hospitalization risk by 35%.
Timing matters more than anything. If you wait 72 hours, the benefit drops sharply. One patient story from a CDC case report: waited three days for antivirals. By day five, had pneumonia. Another: started Tamiflu 12 hours after fever hit. Back to work in three days instead of seven.
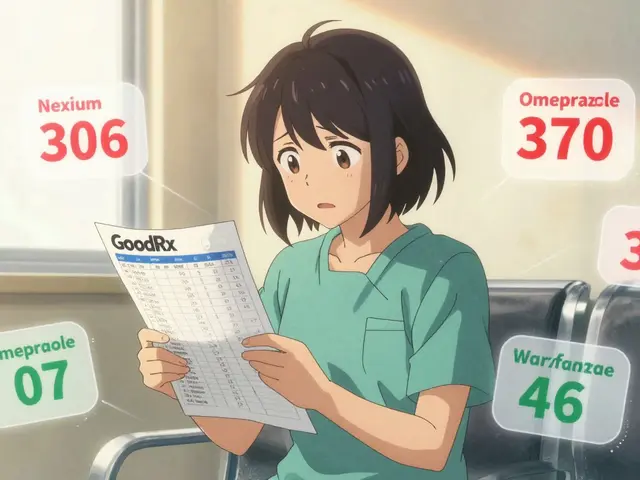
Costs vary. Generic oseltamivir runs $15 to $30 for a full course. Brand-name Tamiflu? $105 to $160 without insurance. Xofluza is a single dose but costs $150 to $200. Insurance helps, but not always enough.
What About Cold Treatments?
No antivirals exist for colds. Not because scientists haven’t tried. Rhinoviruses have over 160 strains. Making one drug to stop them all is nearly impossible.
So you treat symptoms. Decongestants like pseudoephedrine reduce nasal stuffiness by 30-40%. Acetaminophen or ibuprofen brings down fever and eases aches. Zinc lozenges? Some studies say they can shorten a cold by 1.6 days-if you start within 24 hours of symptoms and take 75mg daily. But many people report a terrible metallic taste. One WebMD review gave it 2.4 out of 5 stars for that reason.
Rest and fluids are still the best tools. No magic pill. Just time.
Flu vs. COVID-19: How to Tell Them Apart
It’s 2025. You’re sick. Is it flu? Is it COVID? The symptoms overlap so much-cough, fever, fatigue, sore throat.
But there’s one big clue: loss of taste or smell. That was a hallmark of early COVID-19. Around 80% of people with early infection lost these senses. It’s rare in flu. If you can’t taste your coffee or smell your shampoo, think COVID.
Flu doesn’t usually cause diarrhea or vomiting in adults. But in the 2022-2023 season, 45% of flu patients reported GI symptoms-nausea, stomach pain, even vomiting. That’s new. Doctors are updating their mental checklists.
Bottom line: if you’re unsure, get tested. Rapid flu tests give results in 15 minutes. They’re 95% accurate. Don’t guess. Know.
Why So Many People Get It Wrong
Doctors misdiagnose flu as a cold 30-40% of the time, especially early on. Symptom checklists only work about 60-70% of the time. People assume, “I’ve had the flu before, this doesn’t feel that bad.” They wait. They take antibiotics-useless against viruses-and make antibiotic resistance worse.
Only 18% of high-risk patients get antivirals within the critical 48-hour window, according to Dr. William Schaffner of Vanderbilt. That’s a failure of awareness, not medicine.
And then there’s the myth: “I don’t need to see a doctor for the flu.” You do-if you’re in a high-risk group, or if you’re getting worse after day three. Fever returning after it went away? That’s a red flag for secondary infection.
What You Can Do Right Now
- If you feel flu symptoms-fever, body aches, sudden fatigue-call your doctor today. Don’t wait.
- Ask about rapid flu testing. It’s fast, accurate, and worth it.
- If you’re over 65, pregnant, or have a chronic illness, keep a prescription for oseltamivir or baloxavir on hand. Have it filled before flu season hits.
- For colds, skip the antibiotics. Use zinc lozenges if you tolerate them. Rest. Hydrate.
- Get your flu shot every year. Even at 40-60% effectiveness, it cuts hospitalizations and deaths.
What’s Coming Next
Flu vaccines are improving. The 2023-2024 shot covers four strains, including new ones from Australia and Europe. Moderna is testing an mRNA flu vaccine-like the ones for COVID-with Phase III results expected in early 2024.
Scientists are also chasing a universal flu vaccine. One targeting the stem of the flu virus’s hemagglutinin protein has shown 70% cross-strain protection in monkeys. If it works in humans, we might not need a yearly shot anymore.
Antivirals are getting better too. New drugs in trials aim to work even after the 48-hour window. Resistance is still a problem-1.5% of H1N1 strains are now resistant to oseltamivir-but the pipeline is active.
Climate change is extending flu season by about 12 days each year. More time for spread. More pressure on the system. That’s why knowing the difference-and acting fast-is more important than ever.
Can you get the flu from the flu shot?
No. Flu shots use inactivated or recombinant viruses-they can’t cause infection. Some people feel sore at the injection site, or get a low-grade fever or muscle aches for a day. That’s your immune system responding, not the flu. If you get sick after the shot, you were likely exposed before vaccination or caught another virus.
Do antivirals work if you’ve had symptoms for more than 48 hours?
They’re less effective, but not useless. For high-risk patients-those over 65, with asthma, diabetes, or heart disease-antivirals can still reduce complications and hospitalization risk even after 48 hours. The CDC recommends considering treatment up to 5 days after symptom onset for those at risk. But the sooner, the better.
Is zinc really effective for colds?
Some studies show zinc lozenges can shorten a cold by about 1.6 days if taken within 24 hours of symptoms and at a dose of 75mg per day. But results are mixed. Many people can’t tolerate the metallic taste. Long-term use may cause copper deficiency. The CDC says evidence is inconsistent. It’s a possible tool, not a guaranteed fix.
How do I know if my child has the flu and not just a cold?
Kids often get higher fevers with flu-sometimes over 104°F. They may also have vomiting, diarrhea, or extreme tiredness. Cold symptoms in children are usually just runny nose, cough, and mild fever. If your child is lethargic, breathing fast, not drinking fluids, or seems unusually irritable, get them checked. Flu can progress quickly in kids.
Can you have flu and a cold at the same time?
Yes. It’s rare but possible. You could be infected with a rhinovirus (cold) and influenza virus at the same time. That can make symptoms worse and recovery longer. Testing is the only way to know for sure. If you’re getting worse instead of better after a few days, see a doctor.
Should I go to work or school if I have cold or flu symptoms?
If you have a cold, stay home if you’re sneezing, coughing, or feeling unwell-you can still spread it. But if you have flu symptoms-fever, body aches, extreme fatigue-stay home. Flu is highly contagious. You’re most infectious the first 3-4 days. Going to work or school risks spreading it to others, especially vulnerable people. Employers and schools should encourage sick leave for flu.
Write a comment
Items marked with * are required.




12 Comments
Katy Bell November 23, 2025 AT 09:11
Just had the flu last month. Felt like my bones were melting. Took Tamiflu at 36 hours and honestly? Saved my job. Still tired for weeks, but didn’t end up in the ER. Don’t wait.
Olanrewaju Jeph November 23, 2025 AT 18:04
For those in Nigeria, access to antivirals is still a challenge. Many rely on herbal remedies or self-medicate with antibiotics. We need better public health education-not just for flu, but for distinguishing it from malaria and dengue, which present similarly. The WHO should prioritize this in low-resource settings.
Dalton Adams November 24, 2025 AT 18:50
Let’s be real-most people don’t know the difference between a rhinovirus and an orthomyxovirus. I’ve seen patients bring me OTC cold meds for flu and then get mad when I don’t prescribe antibiotics. 🤦♂️ The CDC data is solid, but public health literacy is a joke. Also, zinc lozenges? The only thing they’re good for is making you gag. Save your money and get the shot.
Suresh Ramaiyan November 25, 2025 AT 09:22
I used to think colds were just ‘mild flu’-until I watched my dad get hospitalized at 72. He had diabetes. He didn’t even think it was serious until he couldn’t breathe. That’s when I started keeping Tamiflu in the medicine cabinet. Not for me-for the people who can’t fight this alone. We need to stop normalizing viral illness as ‘just part of winter.’ It’s not.
And yes, the flu shot isn’t perfect. But it’s like wearing a seatbelt. You don’t need it every day, but when you need it? You’ll be glad you had it.
Also, climate change is making flu season longer. We’re not just dealing with winter anymore. It’s fall-to-spring now. That’s not a coincidence. It’s a warning.
And for the love of God, stop saying ‘I got the flu from the shot.’ No. You got it from your cousin who came over for Thanksgiving with a cough. The shot doesn’t give you the flu. It gives you a fighting chance.
People need to stop treating medicine like a buffet. You don’t get to pick and choose which science to believe. This isn’t politics. It’s biology.
I’m not mad. I’m just… tired of losing people who didn’t have to go.
JD Mette November 27, 2025 AT 08:48
My mom got the flu shot every year. She was 81. Last year she got sick anyway. But she didn’t go to the hospital. Didn’t need oxygen. Just stayed home for two weeks. I think the shot helped. I don’t know for sure. But I’m getting mine again this year.
Jennifer Skolney November 27, 2025 AT 13:05
Just got my flu shot today!! 🌡️💉 My grandma always said, ‘Better safe than sorry.’ And she was right. Also, I keep zinc lozenges in my purse now. Even if they taste like battery acid, I’ll swallow it. 🤢
Kane Ren November 27, 2025 AT 19:11
If you’re reading this and you’re under 30 and think you’re invincible-please stop. I was 24. Thought I was fine. Ended up in the ICU with viral pneumonia. Took 3 months to get back to normal. Your body isn’t a game. This isn’t a ‘tough it out’ situation. Get tested. Get help. Please.
Charmaine Barcelon November 28, 2025 AT 13:34
Ugh. I hate when people say ‘zinc helps.’ It doesn’t. It’s a scam. And Tamiflu? Overrated. I had the flu last year. Took it. Still felt awful. Just rest. Drink water. Stop listening to doctors.
Javier Rain November 30, 2025 AT 08:57
Hey-just wanted to say thank you for this post. I shared it with my whole family. My sister’s a nurse, my brother’s got asthma, my mom’s 70. We’re all getting tested early this year. No more guessing. No more waiting. We’re acting. That’s the win.
Laurie Sala December 1, 2025 AT 11:46
But what about the 40% of people who say the flu shot made them sick? And what about the mercury? And the autism link? I read it on a blog. It’s real. You’re just brainwashed.
Demi-Louise Brown December 3, 2025 AT 06:40
Universal flu vaccine research is promising. The hemagglutinin stem target shows real potential. If human trials replicate the 70% cross-strain protection seen in primates, we could see a paradigm shift in seasonal prevention. This is the future.
Karla Morales December 3, 2025 AT 14:33
Let’s be brutally honest: most people don’t care until someone they love dies. Then they post a tribute. Then they forget. We’re not a society that prepares. We’re a society that reacts. And that’s why we lose 50,000 people a year to something preventable. 😔