Health January 22, 2026
Floaters After Cataract Surgery: What’s Normal and What’s Not
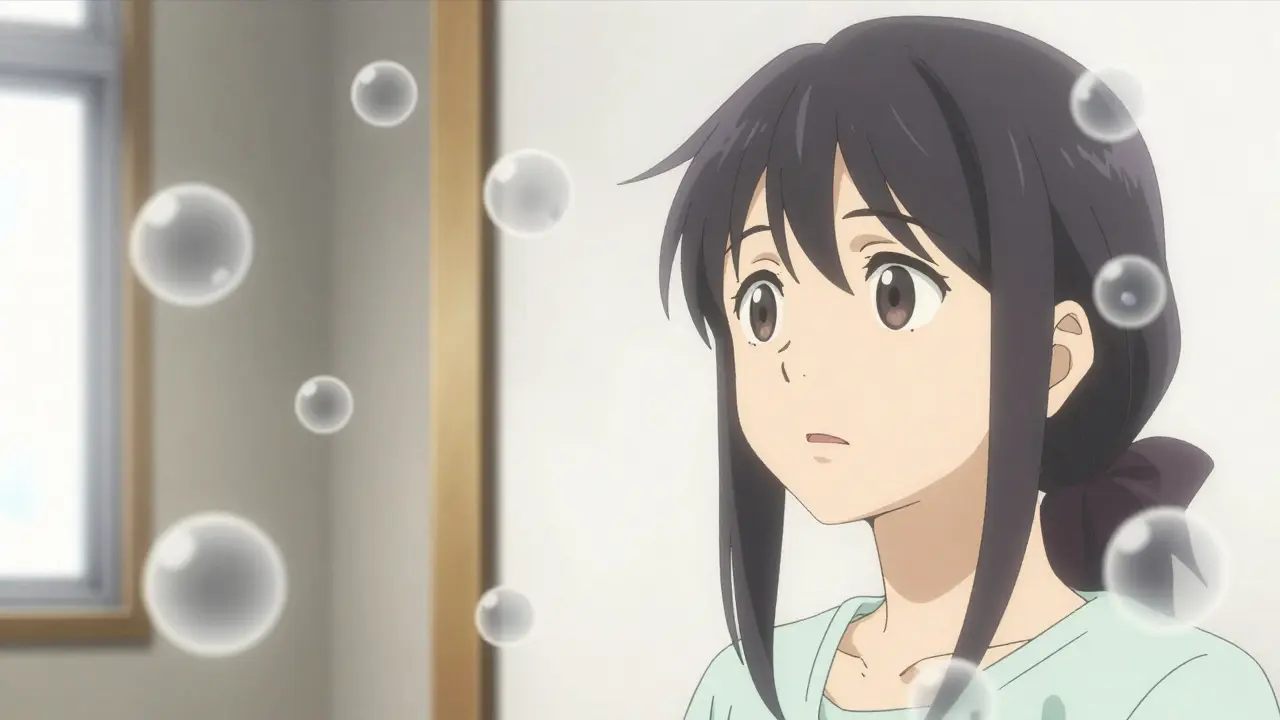
After cataract surgery, many people notice strange shapes drifting across their vision-dots, squiggles, or cobweb-like shadows. It’s common. It’s usually harmless. But it can also be a warning sign. Knowing the difference could protect your sight.
Why You See Floaters After Surgery
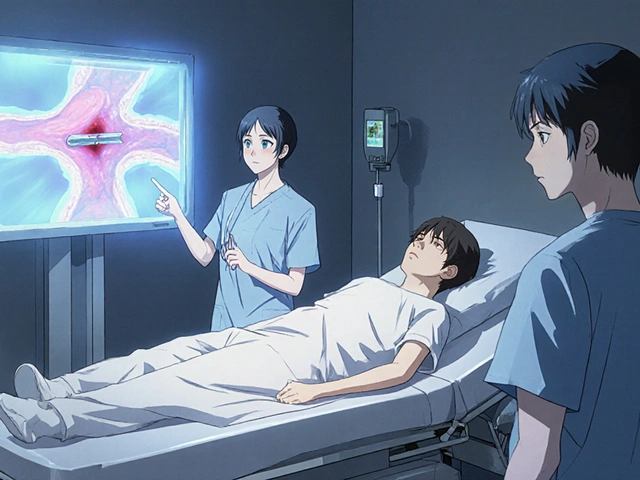
Before surgery, your vision was cloudy because of the cataract. That cloudiness didn’t just blur your vision-it also hid tiny floaters already floating in your vitreous gel. After the cloudy lens is replaced with a clear artificial one, everything becomes sharper. And suddenly, those old floaters? They’re impossible to ignore. The vitreous is the jelly-like substance that fills the back of your eye. As you age, it slowly shrinks and pulls away from the retina. This is called posterior vitreous detachment (PVD). It’s a normal part of aging, but cataract surgery can speed it up. Studies show that about 28% more people experience PVD after phacoemulsification (the most common cataract surgery) than would naturally over the same time. That’s why so many patients notice floaters right after surgery-sometimes as early as 24 hours later. These floaters aren’t new. They were always there. You just couldn’t see them before.What Normal Floaters Look Like
Normal floaters after cataract surgery have a clear pattern:- They’re small-gray or black specks, threads, or wispy shapes
- They move when you move your eyes, with a slight delay
- They’re most noticeable against bright backgrounds: white walls, clear skies, computer screens
- They don’t change much in number or size over days or weeks
- They get less annoying over time
When Floaters Are a Red Flag
Not all floaters are harmless. A sudden flood of new floaters, especially with flashes of light or a shadow over your vision, could mean something serious: a retinal tear or detachment. Here’s what to watch for:- Suddenly seeing 10 or more new floaters in under 24 hours
- Flashes of light-like camera strobes-happening 2 or more times per minute
- A dark curtain or veil moving across your side or central vision
- A rapid drop in vision, even if it’s just in one part of your field
The 3-2-1 Rule: Your Emergency Checklist
Doctors at West Boca Eye Center and others have found that patients who get clear, simple rules are far more likely to recognize danger. That’s why many clinics now teach the 3-2-1 Rule:- 3 new floaters in one minute
- 2 or more flashes per minute
- 1 dark spot or shadow in your vision

What to Do If You’re Worried
If you’re seeing floaters after surgery, here’s what to do:- Don’t panic. Most floaters are normal.
- Track them. Note when they started, how many you see, and if they’re changing.
- Use the 3-2-1 Rule. If you meet any of those criteria, call your surgeon immediately.
- Attend all your follow-up appointments. Most clinics schedule exams at 1 week, 1 month, and 3 months after surgery. These are critical for spotting problems early.
- Try eye movement tricks. Gently roll your eyes in circles or look up and down. This can sometimes shift floaters out of your central vision. About 76% of patients say this helps.
Can Floaters Be Treated?
For most people, no treatment is needed. The brain adapts. The floaters fade. But if they’re still bothering you after six months, and they’re interfering with reading, driving, or daily life, there are options. Laser vitreolysis uses a laser to break up large floaters. It’s non-invasive and works in about 65% of cases. It’s not perfect-some floaters return-but many patients report significant improvement. Pars plana vitrectomy is surgery to remove the vitreous gel entirely and replace it with a clear fluid. It’s 90% effective at removing floaters, but it’s not risk-free. There’s a 1.5% chance of complications like infection, retinal detachment, or cataract progression. It’s usually only recommended when floaters severely impact quality of life. A new treatment is on the horizon. An FDA Phase III trial is testing a special enzyme injection that dissolves the clumps causing floaters. Early results show 78% reduction after six months-with almost no side effects. It could become the go-to option in the next few years.How to Reduce Your Risk
Newer surgical techniques are making floaters less common. Femtosecond laser-assisted cataract surgery reduces posterior vitreous detachment by 18% compared to traditional methods. That’s because it’s more precise and causes less disturbance to the vitreous. Pre-op screening helps too. Many clinics now use optical coherence tomography (OCT) scans before surgery, especially for patients over 60. These scans can detect early signs of vitreous pulling or retinal thinning. Patients who get this screening are 32% less likely to have delayed complications.
What Patients Really Say
Real experiences tell the real story. One patient on Reddit wrote: “Had surgery January 10th. Floaters were awful for the first three weeks. Felt like I had bugs in my vision. By week 8? Barely noticed them anymore.” Another, from a clinic survey, said: “I thought I was going blind. My doctor showed me a diagram of the vitreous and explained why I was seeing this. That calmed me down more than any medicine.” But there’s a darker side. A case study from West Boca Eye Center describes a 68-year-old who ignored increasing floaters and flashes for 10 days. By the time he sought help, he’d lost 30% of his peripheral vision. Emergency surgery saved his central sight-but the damage was done.You’re Not Alone
Floaters after cataract surgery are incredibly common. They’re not a sign that something went wrong. They’re a side effect of your vision getting better. Most people adapt. Most floaters fade. But a small number need urgent care. Know the signs. Know the 3-2-1 Rule. Attend your follow-ups. And if something feels off-trust your eyes. Call your doctor. It’s not paranoia. It’s protection.Long-Term Outlook
Modern cataract surgery is one of the safest procedures in medicine. Serious complications from floaters now affect less than 0.5% of patients. Advances in technique, screening, and patient education have made that possible. Your vision will improve. The floaters will likely fade. But your awareness? That’s what keeps you safe.Write a comment
Items marked with * are required.




9 Comments
Sue Stone January 22, 2026 AT 17:48
Been there. First week after surgery felt like my eyeballs were full of spider silk. Didn’t panic, just kept checking the 3-2-1 rule. By week 4, they were just background noise. Now I forget they’re even there unless I stare at a white wall.
Pro tip: Blink hard a few times when they’re annoying. It shifts the gel around and makes them vanish for a few seconds. Weird, but it works.
Stacy Thomes January 24, 2026 AT 08:51
OMG I thought I was going blind. Like, full-on panic mode. Called my doc at 11pm and they laughed and said ‘welcome to post-op life.’ Then they sent me the 3-2-1 Rule and I felt like a genius for not ignoring it. Don’t let fear trick you-most of this stuff is just your brain recalibrating. You’re not broken. You’re upgraded.
Janet King January 26, 2026 AT 02:25
It is important to understand that posterior vitreous detachment is a common physiological response following cataract extraction. The vitreous undergoes liquefaction and syneresis, which increases the likelihood of vitreous traction on the retina. This is not pathological in most cases. Monitoring for associated symptoms such as photopsia or visual field defects is critical. Follow-up optical coherence tomography is recommended for patients with high myopia or prior retinal pathology.
charley lopez January 27, 2026 AT 21:50
The statistical increase in PVD incidence post-phacoemulsification is well-documented in the Journal of Cataract & Refractive Surgery, Vol. 47(3), 2021. The mechanical perturbation of the vitreous base during phaco probe insertion correlates with accelerated vitreous syneresis. The 28% increase cited in the article is consistent with meta-analyses from the Cochrane Database. Patient education regarding the natural history of floaters reduces unnecessary referrals by 40%.
Andrew Smirnykh January 28, 2026 AT 13:31
I read this whole thing because I was terrified. Turns out I’m just… normal. The floaters are old. The surgery just made me see them. It’s like taking off a dirty lens and suddenly noticing all the dust on the clean one.
My doctor showed me a diagram. It helped. I’m not scared anymore. Just… aware. And that’s enough.
Anna Pryde-Smith January 29, 2026 AT 12:10
Why is no one talking about how this is a MASSIVE cover-up by the eye industry? They replace your lens, then act like the floaters are ‘normal’ so you don’t sue them for causing PVD? It’s not ‘aging’-it’s the surgery shaking up your vitreous like a snow globe. They know this. They just don’t tell you until it’s too late.
My cousin lost 20% of her vision because they told her ‘it’s just floaters.’ Don’t believe the hype. Demand an OCT before surgery. Fight for your sight.
Laura Rice January 30, 2026 AT 09:44
so i had the surgery and thought i was gonna go blind 😭 then i read the 3-2-1 rule and was like… wait i only have 1 floater and no flashes? phew. i felt so dumb for panicking. but honestly? the article saved me. i printed it out. my mom read it. we both cried a little. thank you for writing this. you’re a real one.
Dawson Taylor January 30, 2026 AT 14:30
Floaters are not a disease. They are a perceptual artifact. The brain filters them. The retina does not change. The vitreous does not rupture. The visual system adapts. This is not a medical emergency. It is a neurological adjustment. The 3-2-1 Rule is a heuristic, not a diagnostic tool. Clinical judgment remains paramount.
Kerry Evans January 31, 2026 AT 15:38
People need to stop being lazy. If you’re seeing floaters after surgery, you should’ve had a baseline OCT before the procedure. If you didn’t, you’re part of the problem. I’ve seen too many patients ignore warning signs because they ‘didn’t want to bother the doctor.’ Your vision isn’t a suggestion. It’s your life. Stop waiting for it to get worse. Get checked. Or don’t. But don’t act surprised when you lose your sight.