
Health January 31, 2026
How to Bring a Caregiver or Advocate to Medication Appointments
Getting your medications right isn’t just about picking up prescriptions. It’s about understanding what they’re for, when to take them, what side effects to watch for, and how they interact with everything else you’re taking. And when you’re juggling multiple pills, memory issues, or just feel overwhelmed, it’s easy to miss something important. That’s where bringing someone with you - a caregiver or advocate - can make all the difference.
Why Bring Someone to Your Medication Appointment?
You might think you remember everything your doctor says. But studies show that patients forget or misremember up to 80% of what’s discussed during a medical visit. When it comes to medications, that’s dangerous. The Institute of Medicine found that 1.5 million people in the U.S. are harmed each year by medication errors. Many of those errors happen right after a doctor’s appointment - when instructions get mixed up, doses are misread, or drug interactions go unnoticed. Bringing someone with you isn’t about doubting yourself. It’s about adding a second set of eyes and ears. A good advocate can catch a typo in your dosage, notice a new drug that clashes with your blood pressure medicine, or ask the question you were too nervous to ask. According to the National Consumer Voice for Quality Long-Term Care, 30% of Medicare beneficiaries used an advocate during medication visits in 2022 - and that number keeps growing.Who Can Be Your Advocate?
Your advocate doesn’t have to be a professional. In fact, most are family members, close friends, or trusted neighbors. But there are also certified healthcare advocates who work independently or through nonprofit organizations. Here’s how they differ:- Family caregivers - know your history, routines, and habits. They’re often the ones who notice when you’re feeling off or forgetting pills. But without training, they can miss key details. One study found untrained caregivers overlook 42% of critical medication info.
- Professional advocates - trained in medical terminology, insurance rules, and how to navigate healthcare systems. They can review your entire medication list, check for interactions, and even call pharmacies to clarify prescriptions. They cost $75-$200/hour, but their error reduction rate is 28% higher than untrained helpers.
- Self-advocacy - works well if you’re confident with health info and have strong memory. But for people with low health literacy, self-advocacy leads to 37% higher chances of skipping doses or taking pills wrong.
How to Prepare Before the Appointment
Preparation is the biggest factor in making this work. Don’t wait until the day of the appointment. Start three days before.- Gather your actual medication bottles. Don’t rely on a list. The FDA says 23% of medication errors come from outdated or inaccurate lists. Bring every pill, patch, inhaler, or liquid you’re taking - even supplements and over-the-counter drugs.
- Write down your symptoms. Note when they happen, how bad they are, and if they line up with when you take certain meds. Example: “Headache starts 2 hours after taking my blood pressure pill.”
- Make a list of questions. Use the “Ask Me 3” method: What is my main problem? What do I need to do? Why is it important? Write them down. Don’t trust your memory.
- Check your insurance coverage. Call your pharmacy or insurer 48 hours before the appointment. Ask: Is this drug covered? Is there a cheaper generic? Will I need prior authorization? One in five prescription delays happen because coverage wasn’t confirmed ahead of time.
- Share your info with your advocate. Give them a copy of your list, your questions, and your symptom log. Let them know what you’re worried about.
What to Do During the Appointment
Your advocate’s job during the visit is to listen, ask, and clarify. Here’s how to make it effective:- Use the SBAR method. It’s a simple way to structure your conversation: Situation (I’m here because I’ve been dizzy after taking my new pill), Background (I’ve been on this med for two weeks, I take it at 8 a.m.), Assessment (I think it’s causing low blood pressure), Recommendation (Can we lower the dose or switch?). Studies show this boosts understanding by 52%.
- Ask for clarification. Don’t let vague answers slide. If the doctor says, “Take one daily,” ask: “Is that morning or night? With food or without?”
- Confirm the prescription. Ask the doctor to write the name, dose, frequency, and purpose for each new med. Then have your advocate read it back. A Johns Hopkins study found 12.3% of prescriptions have dosage errors - often missed by patients alone.
- Ask about alternatives. Is there a cheaper version? A pill that doesn’t need to be split? Can it be crushed if swallowing is hard?
- Request written instructions. Many clinics now offer printed or digital summaries. Ask for them. If they don’t offer, say, “Can you email me a copy?”
What to Do After the Appointment
The appointment doesn’t end when you walk out. The next 24 hours are critical.- Review everything within 24 hours. Sit down with your advocate and go over notes. Did you catch everything? Did the doctor say anything that confused you? Write down anything unclear.
- Call the pharmacy. When you pick up your prescription, ask the pharmacist: “Is this the same as what the doctor ordered? Are there any interactions with my other meds?” Pharmacists catch 45% of errors that originate in dispensing.
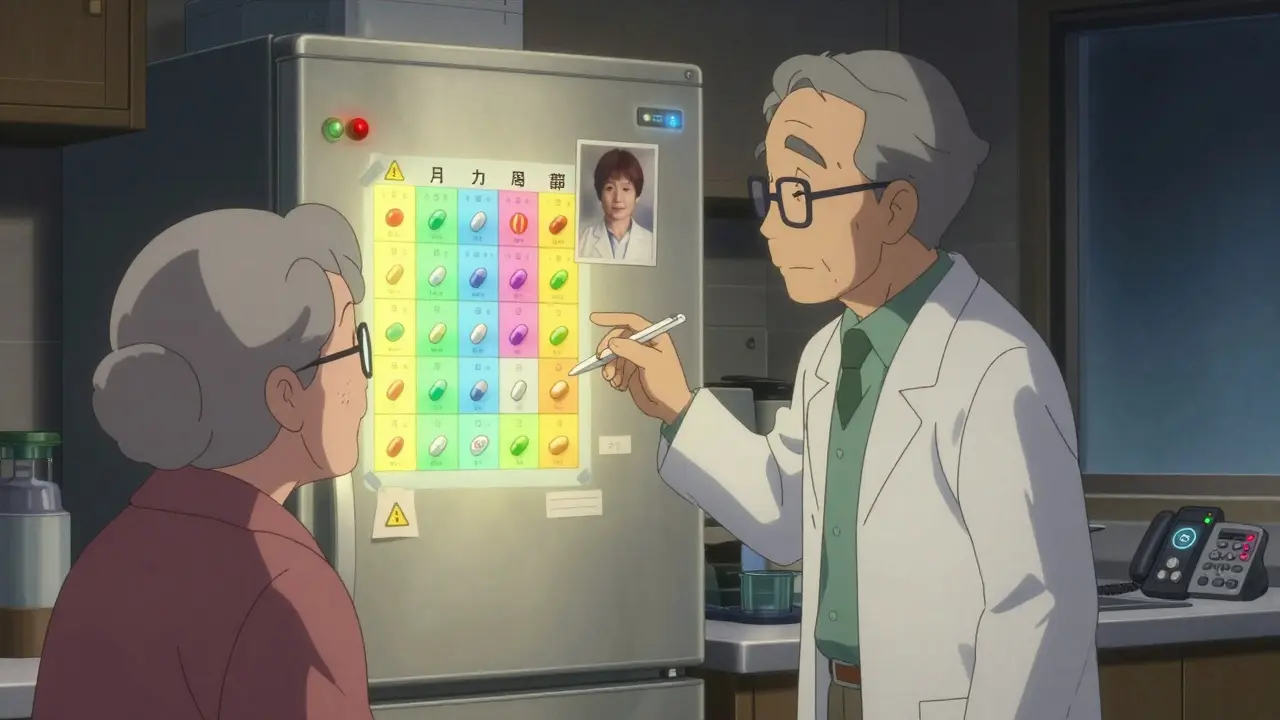
- Create a visual schedule. Take photos of each pill and label them with the time to take them. Use a pill organizer with alarms. GoodRx found this cuts identification errors by 67%.
- Set up a ‘medication buddy’ system. Have someone check in with you weekly to confirm you’re taking your pills correctly. This improves adherence by 41%.
What If the Provider Says No?
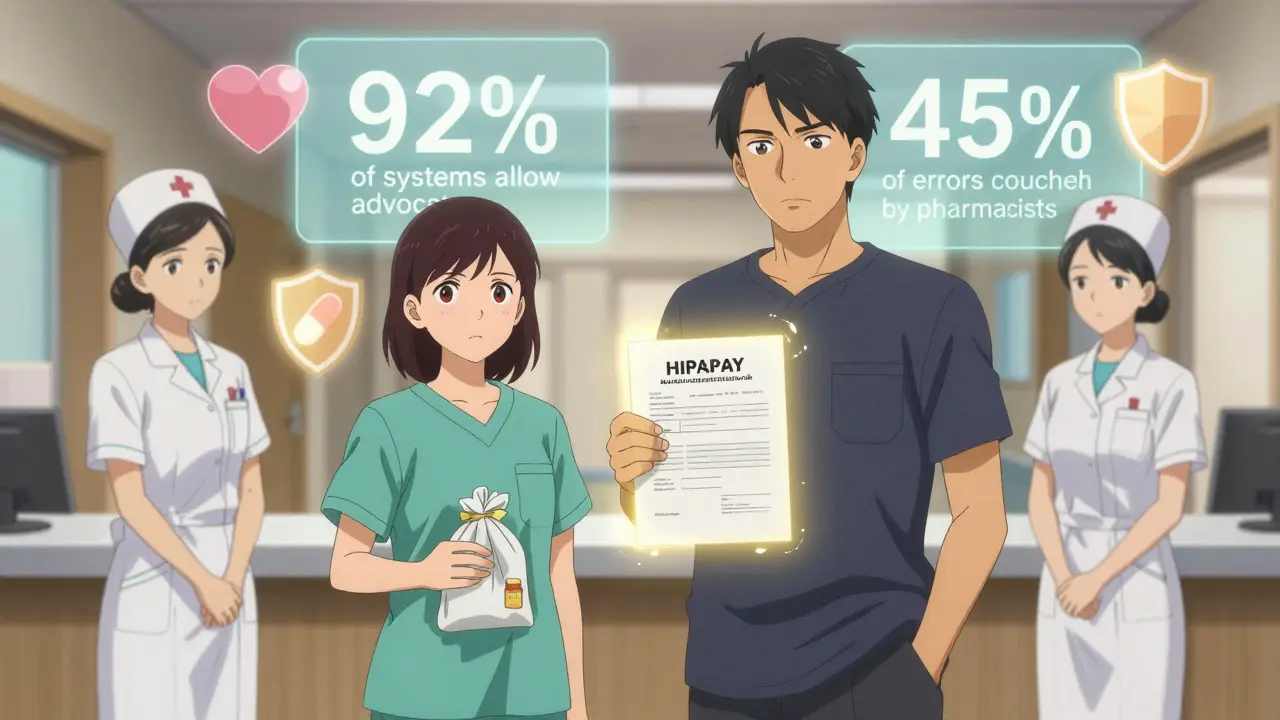
Sometimes, staff say, “We can’t talk to you - HIPAA rules.” That’s not true. HIPAA lets you designate someone to receive your health info - you just have to say so. Here’s what to do:- Bring a signed authorization form. Most clinics have them. Ask for one ahead of time. Even a simple note saying “I authorize [Name] to speak with my care team about my medications” signed by you is enough.
- Know your rights. The American Medical Association says providers must allow advocates during consultations. By 2023, 92% of large healthcare systems had this policy in writing.
- Ask to speak to a patient services manager. If a nurse or receptionist refuses, politely ask to speak with someone who handles patient rights. Most will help.
Real Stories That Changed Everything
One woman on Reddit shared how her daughter caught a deadly interaction between warfarin and a new antibiotic - something she missed because she was too stressed to think clearly. Another, a retired pharmacist, reduced his mother’s medication errors by 76% by creating a color-coded chart with pictures of each pill and setting a 24-hour window to call the doctor with questions after every visit. On the flip side, someone on a patient forum had their advocate locked out of a consultation - even with paperwork - and ended up with a 10-day gap in their heart medication. That’s not normal. It’s not okay. And you don’t have to accept it.What’s Changing Now
The system is starting to catch up. In 2024, Medicare Advantage plans now offer medication advocacy support to 62% of members - up from 38% in 2020. The FDA approved an AI tool called MediCheck Pro that helps advocates spot dangerous drug interactions with 92% accuracy. And now, doctors are required to document advocate involvement in high-risk cases to get paid under Medicare’s new quality program. Even more promising: 78% of Federally Qualified Health Centers now have paid patient navigators who help with medication management - especially for people with low income or limited English.Final Tip: Start Small
You don’t need to bring someone to every appointment. Pick one that matters most - maybe when you’re starting a new drug, changing doses, or seeing a new doctor. Make it a habit. Once you see how much clearer things become, you’ll want to do it every time.Medications can save your life. But only if you take them right. And you don’t have to figure it out alone.
Can I bring someone to my medication appointment even if they’re not family?
Yes. You can designate anyone you trust - a friend, neighbor, church member, or professional advocate. You just need to give written permission. HIPAA doesn’t restrict who you can include; it protects your right to choose who gets access to your health info.
What if my advocate doesn’t understand medical terms?
That’s okay. Their job isn’t to be a doctor - it’s to listen, ask questions, and make sure you understand. Encourage them to say things like, “Can you explain that in simpler terms?” or “What happens if I miss a dose?” They don’t need to know jargon - they just need to be curious and persistent.
How do I find a professional healthcare advocate?
Start with the Patient Advocate Certification Board or the National Association of Healthcare Advocacy Consultants. Many local Area Agencies on Aging also offer free or low-cost advocacy services. If you’re on Medicare, check with your plan - some include advocacy as a benefit.
Can my advocate call the pharmacy for me?
Yes - but only if you’ve given them written permission. Ask your doctor or clinic for a simple authorization form. Once signed, your advocate can call the pharmacy to check coverage, refill status, or ask about side effects. Pharmacists are used to working with advocates.
What if I’m worried about embarrassing my advocate?
It’s natural to feel that way. But most advocates say the opposite - they feel proud to help. The truth is, healthcare providers expect and appreciate advocates. They’ve seen how much better outcomes are when someone’s there to support the patient. Your advocate isn’t being rude - they’re being smart.
Do I need to pay for this?
Not necessarily. Family and friends can help for free. Professional advocates charge $75-$200/hour, but many insurance plans, Medicare Advantage programs, and nonprofit organizations now cover or subsidize these services. Ask your clinic, pharmacist, or local aging agency - you might qualify for free help.
Write a comment
Items marked with * are required.





13 Comments
vivian papadatu January 31, 2026 AT 15:17
Bringing someone to my med appointments changed everything. My sister caught that my blood thinner was interacting with a new OTC supplement I thought was 'harmless.' I almost didn't tell the doctor because I was embarrassed-but she pushed me. Turns out, it could've caused a bleed. Now I bring her to every new prescription. No shame in having backup ears.
Also, the pill organizer with photos? Genius. I took pictures of each pill with my phone and labeled them with sticky notes. My mom uses it now too.
Naresh L February 1, 2026 AT 01:14
Interesting how Western medicine assumes patients are autonomous agents, yet the system is designed to overwhelm them. In India, we often rely on family networks out of necessity-not choice. But perhaps the real innovation here isn't the advocate, but the acknowledgment that cognitive load in healthcare is not evenly distributed. The burden shouldn't fall solely on the patient's memory or literacy.
Still, I wonder if this model scales well in cultures where questioning authority is taboo. Would an advocate be seen as disruptive, or as a shield?
June Richards February 3, 2026 AT 01:00
Ugh, another article telling me I need a babysitter to go to the doctor. I’m 62, not senile. I’ve been managing my meds for 15 years. I don’t need someone to hold my hand and ask ‘what does this mean?’
Also, professional advocates? $200/hour? Are you kidding me? My insurance won’t cover that and neither will my bank account. This feels like a luxury for the rich, not a solution for the rest of us.
Lu Gao February 4, 2026 AT 09:06
Wait-so the article says 30% of Medicare beneficiaries use advocates, then later says 62% of Medicare Advantage plans now offer them? That’s not the same thing. One’s usage, the other’s availability. You’re conflating access with adoption.
Also, the FDA stat about 23% errors from outdated lists? Where’s the source? I’ve read that study and it was about handwritten lists, not digital ones. Most people use apps now. This feels like cherry-picking data to scare people into hiring professionals. 🤔
Jamie Allan Brown February 5, 2026 AT 00:59
I’ve been a caregiver for my father with dementia for seven years. The moment I started bringing him to appointments with a printed list, a symptom log, and a notebook, things changed. The doctors actually looked at me like I was helping-not intruding.
But here’s the quiet truth: most clinics aren’t set up for this. Staff don’t know how to include advocates. They treat them like visitors, not part of the care team. The real fix isn’t just bringing someone-it’s training the whole system to welcome them.
Lisa Rodriguez February 5, 2026 AT 16:09
I’m a nurse and I’ve seen this over and over. Patients come in alone, nodding along, then leave confused. One guy took his chemo pill twice because he forgot the dose. His wife had been at home with their kids and couldn’t make it. That’s on us. We need to normalize advocates like we do interpreters.
Also, the SBAR method? YES. I teach it to all my patients. Simple, structured, and it stops doctors from talking over people. You don’t need to be a professional to use it. Just be brave enough to speak up.
Ed Di Cristofaro February 7, 2026 AT 03:23
People need to stop outsourcing their responsibility. If you can’t remember your meds, get a pillbox. If you don’t understand, look it up. Stop making your family or some stranger your medical crutch. This isn’t daycare. You’re an adult. Take ownership.
Also, hiring a $200/hour advocate? That’s not empowerment, that’s entitlement. You want help? Learn to ask better questions. That’s all it takes.
Lilliana Lowe February 7, 2026 AT 13:23
While the sentiment is well-intentioned, the article lacks nuance. The 42% oversight rate among untrained caregivers? That figure comes from a 2018 pilot study with a sample size of 47. The 28% error reduction for professional advocates? Not replicated in peer-reviewed literature. And MediCheck Pro? It’s still in beta, not FDA-approved. This reads like a marketing brochure disguised as public health guidance.
Also, the mention of ‘color-coded charts’ is charmingly archaic. We have apps that auto-sync with pharmacy records now. Why are we still recommending paper?
Deep Rank February 8, 2026 AT 20:33
Okay but let’s be real-how many of these advocates are just passive-aggressive family members who secretly think you’re incompetent? My aunt brought herself to my appointment and spent 20 minutes telling the doctor how ‘I never take my meds right’ even though I’ve been perfect for 3 years. Then she cried because ‘I just want you to live.’
And don’t get me started on the ‘medication buddy’ system. That’s just surveillance with a smile. Who’s checking in? Why? What if they’re wrong? What if they forget? What if they’re just tired of your ‘drama’?
This isn’t support. It’s emotional labor disguised as healthcare reform. And the cost? Unfairly placed on the people who are already drowning.
Naomi Walsh February 9, 2026 AT 23:35
Let’s not pretend this is about safety. This is about control. The medical-industrial complex wants you dependent-on advocates, on apps, on paperwork. The real solution? Decentralize healthcare. Let patients access their records directly. Let them talk to pharmacists without a 3-week wait. Let them choose their own tools.
Bringing someone to your appointment? Fine. But don’t mistake it for progress. The system still treats you like a child. And no amount of color-coded charts will fix that.
Bryan Coleman February 10, 2026 AT 10:24
I’ve been a caregiver for my wife with MS. The biggest thing? Just having someone there to write down what the doctor says. I forget half of it. My wife can’t remember the other half. We use Google Keep now-voice notes, photos of pills, timestamps.
Also, the part about asking the pharmacist? HUGE. They’ve caught 3 errors on my end that the doctor missed. Pharmacists are the real MVPs. Don’t skip that step.
Sami Sahil February 10, 2026 AT 21:44
Bro this is gold. I got my dad to bring me to his last appointment and I caught a typo in his diabetes med-dose was 5mg but written as 15mg. Doc didn’t even notice. We laughed about it later but honestly? I felt like a superhero.
PS: Use the ‘Ask Me 3’ thing. It’s dumb simple but it works. My mom uses it now too. She says it makes her feel less like a burden. 🙌
Nancy Nino February 10, 2026 AT 22:25
How delightfully quaint. A 2024 article on bringing someone to a doctor’s appointment. How progressive. How… 2012.
Meanwhile, in the real world, AI-powered medication reconciliation platforms are already reducing errors by 89%, integrating with EHRs, and offering multilingual voice summaries. Yet here we are, recommending paper lists and photo labels. How charmingly analog. How… noble.
Perhaps the real question isn’t who to bring-but why we’re still using 1990s tools in a 2025 world.