Health January 28, 2026
How to Request a Lower-Cost Therapeutic Alternative Medication
Every year, millions of Americans skip doses, cut pills in half, or don’t fill prescriptions at all because they can’t afford their meds. It’s not laziness or ignorance-it’s simple math. A $400 monthly pill for a chronic condition can eat up half a paycheck. But here’s the truth: you don’t have to accept that price. There’s often a therapeutic alternative-a different drug that works just as well, costs a fraction, and your doctor can prescribe instead.
What Is a Therapeutic Alternative?
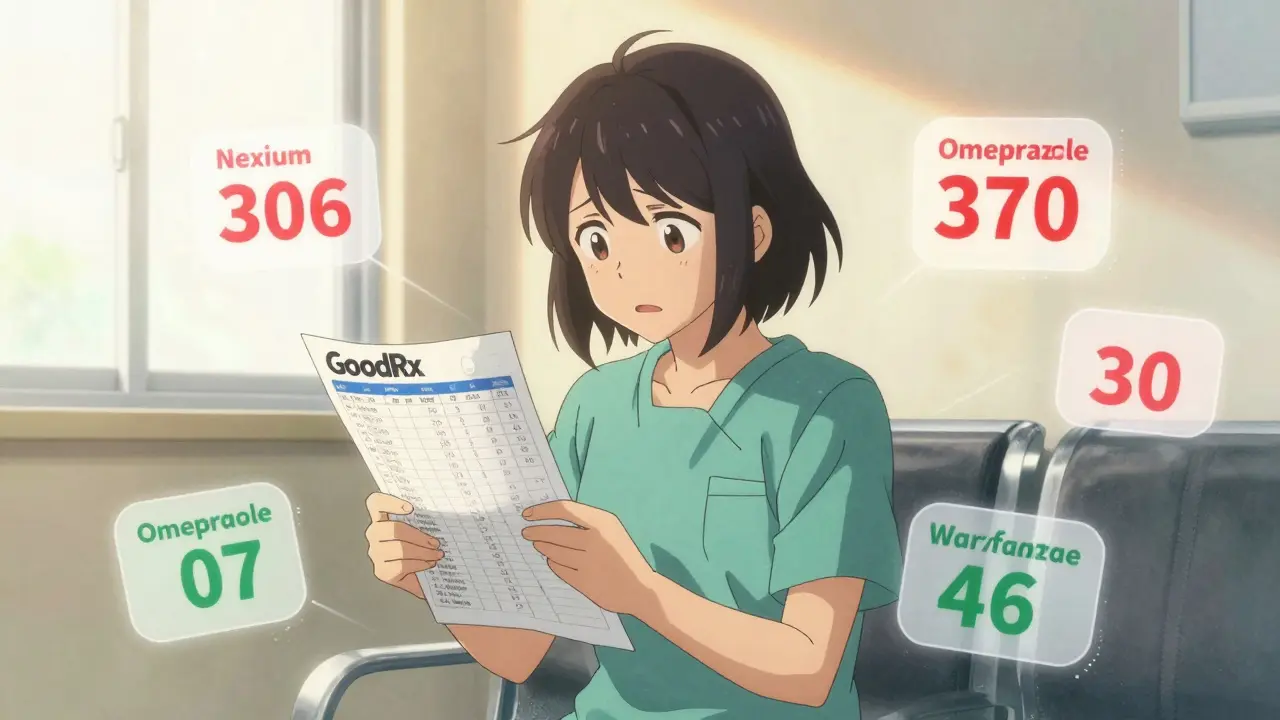
A therapeutic alternative isn’t a generic version of your current drug. It’s a different medication, chemically distinct, but proven to treat the same condition just as effectively. For example, if you’re on esomeprazole (Nexium) for acid reflux, your doctor could switch you to omeprazole, a generic that does the same job. The cost? From $365 a year down to $15. That’s not a guess. That’s real data from Healthgrades in 2023.Therapeutic interchange-this is what doctors call it-works for blood pressure, diabetes, depression, cholesterol, and many other long-term conditions. It’s not experimental. It’s backed by studies from Vanderbilt, the American Academy of Family Physicians, and the Congressional Budget Office. The goal? Keep you healthy without bankrupting you.
Why Your Doctor Might Hesitate
You ask your doctor for a cheaper option, and they say, “This one’s best for you.” That’s frustrating. But here’s why it happens: most doctors weren’t trained to think about cost. They’re trained to think about efficacy and safety. And while most therapeutic alternatives are clinically equivalent, some doctors worry about small differences in how patients respond.For example, two different GLP-1 drugs for diabetes might lower blood sugar by 1.2% versus 1.5%. That 0.3% difference matters to some patients. Others don’t notice it at all. The problem? Doctors don’t always have time to check formularies, compare prices, or dig into the latest clinical guidelines. They rely on what’s familiar.
That’s where you come in. You’re not just a patient-you’re a partner. If you bring specific data, you make it easier for them to say yes.
How to Ask for a Lower-Cost Option
Start with this simple phrase: “I’m having trouble affording my medication. Is there another drug that works the same way but costs less?”That’s it. No jargon. No pressure. Just honesty. Studies show that when doctors hear this one question during a routine visit, they’re 40% more likely to consider alternatives. But don’t stop there. Here’s how to make your request stronger:
- Know your drug class. If you’re on Eliquis for blood clots, you’re in the anticoagulant class. Other options include warfarin, rivaroxaban, or apixaban. Warfarin costs about $10 a month. Eliquis? Around $500.
- Check GoodRx. Go to GoodRx.com and type in your drug. It shows prices at nearby pharmacies and lists cheaper alternatives. Print or screenshot the page. Bring it to your appointment.
- Look at the $4 list. Walmart, CVS, and Walgreens all have a $4 generic list. Common meds on it: lisinopril (blood pressure), metformin (diabetes), atorvastatin (cholesterol), and sertraline (depression). If your drug isn’t on it, ask if a similar one is.
- Ask about copay cards. Many brand-name drugs have manufacturer programs that cut your cost to $0 for the first few months. Sites like NeedyMeds and RxAssist list them. Don’t assume you don’t qualify-many programs accept incomes up to $60,000/year.
- Request a 90-day supply. Even if the drug doesn’t change, getting a 3-month supply often cuts your copay by 25%. It’s free money.
Real Examples That Worked
People aren’t imagining this. Real patients have saved hundreds-sometimes thousands-by switching:
- One patient switched from Lyrica (pregabalin) to generic gabapentin for nerve pain. Monthly cost dropped from $450 to $15.
- Another traded brand-name Crestor for generic atorvastatin. Saved $380 a month.
- A woman on Xarelto (blood thinner) switched to warfarin. Her monthly bill went from $450 to $12. She stopped skipping doses entirely.
But not every switch works. One person switched from Jardiance to metformin for diabetes and ended up with uncontrolled blood sugar. They had to go back. That’s why it’s not a DIY decision. It’s a conversation.
What to Do If Your Doctor Says No
If your doctor says, “There’s no alternative,” ask for proof. Say: “Can you show me the clinical guidelines that say this drug is the only option?”Chances are, they don’t have them handy. You can point them to resources like the Institute for Clinical Systems Improvement, which has free, evidence-based therapeutic interchange guidelines for over 125 conditions. Or mention that the American College of Physicians supports therapeutic interchange when two drugs have proven equivalent efficacy and safety.
If they still refuse, ask for a referral to a pharmacist. Many hospitals and clinics now have clinical pharmacists who specialize in cost-saving strategies. They can review your whole list of meds and suggest alternatives you didn’t even know existed.
And if you’re on Medicare Part D? You have rights. You can file a tiering exception request. If your current drug is on a high tier and a cheaper alternative exists, you can ask your plan to cover your current drug at a lower cost. They must respond within 72 hours for urgent cases or 14 days otherwise.

When It Won’t Work
Therapeutic interchange isn’t magic. It doesn’t work for everything. About 15% of specialty drugs-like biologics for rheumatoid arthritis, multiple sclerosis, or cancer-have no therapeutic alternatives. These are complex, targeted treatments. You can’t swap one for another like you can with blood pressure pills.Also, if you’ve tried multiple drugs in a class and only one worked for you, switching might not be safe. Your body responded to that specific chemical structure. That’s not failure. That’s individual biology.
But for the majority of common chronic conditions-high blood pressure, diabetes, high cholesterol, acid reflux, depression, anxiety-therapeutic alternatives exist. And they’re often dramatically cheaper.
What’s Changing in 2026
The landscape is shifting. In January 2025, the American Medical Association updated its guidelines to include new drug classes like GLP-1 agonists for weight loss and diabetes. Epic and Cerner, the two biggest electronic health record systems, now have built-in tools that pop up during prescribing: “Consider switching to generic X for 85% lower cost.”Medicare Part D plans are now required to use standardized criteria for therapeutic interchange. And the proposed Lower Drug Costs Now Act could lower prices for 250 high-cost drugs by 2030. But even if that passes, experts say therapeutic interchange will still matter. Why? Because negotiated prices often still cost 20-40% more than a proven therapeutic alternative.
Artificial intelligence is helping too. A 2024 study showed an AI tool identified safe therapeutic swaps with 89% accuracy-better than most human doctors.
Your Next Steps
Don’t wait for your next appointment. Start now:- Write down every medication you take, including dose and frequency.
- Go to GoodRx.com and search each one. Note the price and any cheaper alternatives listed.
- Check if your meds are on the $4 list at Walmart or CVS.
- Look up your drug on NeedyMeds.org to see if there’s a copay card.
- Bring your notes to your doctor. Say: “I found these options. Can we talk about whether any of them might work for me?”
You’re not asking for a favor. You’re asking for a standard part of care. Cost should never be a barrier to treatment. And with the right information, you can make it happen.
Write a comment
Items marked with * are required.






9 Comments
paul walker January 28, 2026 AT 20:07
Just switched my dad from Eliquis to warfarin last month-his copay dropped from $420 to $8. He’s been on it for 30 years, no issues. Docs don’t tell you this stuff because they’re stuck in their little bubble. Thanks for the push.
Alex Flores Gomez January 30, 2026 AT 16:17
lol at people thinkin they can just swap meds like trading pokemon cards. You think your body’s a damn vending machine? One guy I know went from Jardiance to metformin and ended up in the ER. Don’t be that guy. Let the pros handle it.
Frank Declemij January 31, 2026 AT 13:09
This is exactly the kind of practical advice that’s missing from healthcare conversations. Most patients don’t know about the $4 list or copay cards. Simple steps like checking GoodRx before the appointment can save hundreds. Doctors appreciate when patients come prepared.
Pawan Kumar February 2, 2026 AT 10:14
Interesting how this article conveniently omits the fact that pharmaceutical lobbying has systematically dismantled price transparency for over two decades. The real issue isn’t therapeutic alternatives-it’s that the entire system is rigged to extract profit from illness. AI tools? They’re just another layer of corporate surveillance disguised as care.
Keith Oliver February 3, 2026 AT 10:51
Bro you’re telling people to go to GoodRx like it’s some secret hack? I’ve been using that since 2017. Also, warfarin? Please. INR monitoring is a nightmare. You’re trading $500 for a life of finger pricks and vitamin K restrictions. That’s not savings-that’s punishment.
Kristie Horst February 5, 2026 AT 01:39
How touching. A post that treats patients like rational actors in a perfectly functioning system. Meanwhile, millions are choosing between insulin and rent. You give them a checklist and call it empowerment. But what about the person who can’t afford the bus fare to the pharmacy? Or the one whose doctor won’t even open their chart? This isn’t advice. It’s a Band-Aid on a hemorrhage.
LOUIS YOUANES February 5, 2026 AT 13:03
I’ve been on 7 different antidepressants. Only one worked. The rest made me feel like a zombie trapped in a broken toaster. So yeah, I’m glad you’re telling people to swap meds like they’re swapping socks. I hope your mom’s blood pressure med doesn’t get swapped out while she’s sleeping.
kabir das February 6, 2026 AT 14:01
Wait, wait, wait-so you’re telling me that a $4 generic can replace a $500 brand-name drug... and it’s not dangerous? What about the side effects? The interactions? The fact that the FDA doesn’t regulate generics the same way? You’re playing Russian roulette with people’s lives here. This is reckless. And irresponsible. And dangerous. And unethical. And...
Andy Steenberge February 7, 2026 AT 14:37
Thank you for writing this. I’ve been a nurse for 18 years and I see this every day-people skipping doses because they can’t afford the copay. I’ve had patients cry because they’re choosing between meds and their kid’s school supplies. The $4 list? It’s real. Warfarin? It’s been used since the 1950s. Metformin? One of the safest drugs ever made. The problem isn’t the alternatives-it’s that doctors aren’t trained to talk about cost. You’re not asking for a favor. You’re asking for the standard of care that every patient deserves. And if your doctor resists? Take the list to the pharmacy. Ask the pharmacist. They know more about prices than your doctor does. You’re not being difficult. You’re being smart.