
Health December 22, 2025
Hyperparathyroidism: High Calcium, Bone Loss, and When Surgery Is Needed
When your blood calcium stays too high for too long, your body starts breaking itself down-slowly, silently, and often without warning. This isn’t just a lab number out of range. It’s your bones thinning, your kidneys forming stones, your brain feeling foggy, and your energy vanishing. For many people, this is hyperparathyroidism.
What’s Really Going On Inside Your Body?
Your four tiny parathyroid glands, nestled behind your thyroid in the neck, are meant to keep calcium balanced. They release parathyroid hormone (PTH) when calcium drops. PTH tells your bones to release calcium, your intestines to absorb more from food, and your kidneys to hold onto it instead of peeing it out. In hyperparathyroidism, one or more of these glands go rogue. They keep pumping out PTH even when calcium is already high. That’s like having a faucet turned on full blast while the sink is already overflowing. The result? Blood calcium climbs above 10.5 mg/dL-well past the normal range of 8.5 to 10.2. At the same time, PTH levels stay elevated, often above 65 pg/mL. That’s the key diagnostic sign: calcium up, PTH up. Not down. Not normal. Up. This isn’t rare. About 100,000 Americans are diagnosed each year. Women are three times more likely to get it than men. And it’s more common in African-American populations. Many people live for years without knowing, their symptoms dismissed as aging, stress, or depression.How High Calcium Eats Away at Your Bones
Your bones aren’t just scaffolding-they’re storage units for calcium. When PTH stays high, your bones are constantly tapped. Osteoclasts, the cells that break down bone, go into overdrive. Over time, this leads to measurable bone loss. DXA scans show that people with untreated primary hyperparathyroidism lose 2-4% of bone density each year at the hip and spine. That’s faster than most postmenopausal women lose bone from estrogen drop. After five years, that’s a 10-20% loss. Your fracture risk jumps by 30-50% compared to someone your age without the condition. It’s not just about fragility. Many patients report deep, constant bone pain-especially in the back, hips, or legs. Some mistake it for arthritis or fibromyalgia. Others notice they’re losing height, or their posture is changing. These aren’t normal signs of aging. They’re red flags.Surgery Isn’t Just an Option-It’s the Only Cure
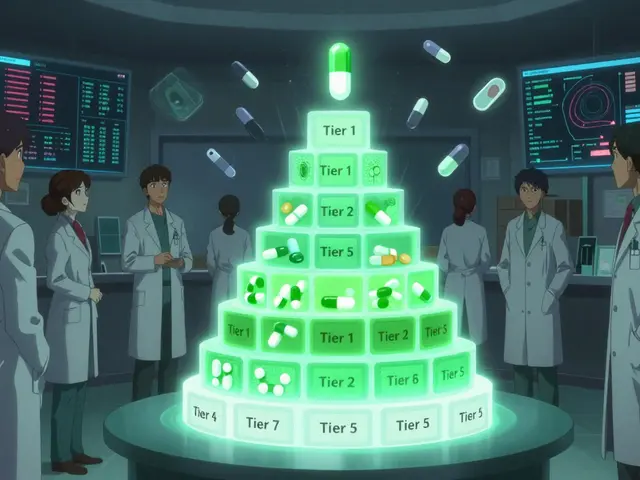
Medications can help manage symptoms, but they don’t fix the root problem. Cinacalcet lowers PTH a bit. Bisphosphonates slow bone loss. But neither stops the glands from overproducing hormone. The only cure? Removing the faulty gland(s). Parathyroidectomy. It’s a targeted, minimally invasive procedure that takes 1-2 hours. In experienced hands, success rates hit 95-98% for single-gland disease-the most common form. Preoperative imaging is critical. A sestamibi scan finds the bad gland in 90% of cases. Ultrasound adds another 85% accuracy. In complex cases, 4D-CT gives near-perfect detail. Surgeons don’t just open your neck and guess-they know exactly where to go. You don’t need to wait until you’re in crisis. The 2022 International Workshop guidelines say surgery should be considered if:- Your calcium is more than 1 mg/dL above normal
- Your kidney function is down (creatinine clearance under 60 mL/min)
- Your bone density is T-score -2.5 or worse (osteoporosis)
- You’re under 50 years old

What Happens After Surgery?
Most people go home the same day. Recovery is quick-3 to 7 days on average. Within weeks, energy returns. Brain fog lifts. Bone pain fades. Your calcium will drop after surgery. That’s normal. In fact, it’s a good sign. But it can cause temporary hypocalcemia-tingling, numbness, muscle cramps. About 30-40% of patients need calcium and vitamin D supplements for a few weeks. A few with multigland disease may need them longer. Bone density starts to recover. Within a year, lumbar spine density improves by 3-5%. By two years, it’s up 5-8%. That’s not just a number-it means you’re less likely to break a hip or spine. But not everyone feels 100% better. About 15-20% of patients still report fatigue or brain fog after surgery. Why? Because prolonged high calcium can damage nerves, kidneys, or even the brain itself. The earlier you act, the better your chance of full recovery.Why So Many People Are Diagnosed Too Late
One patient said it best: “I was misdiagnosed with depression for seven years.” Symptoms like fatigue, memory trouble, irritability, and frequent kidney stones are vague. Doctors often test for depression, anxiety, or chronic fatigue before checking calcium. It’s not negligence-it’s how common these symptoms are. A 2023 survey found 47% of patients waited 2-5 years between first symptoms and diagnosis. One in three saw three or more doctors. That delay is costly. Every extra year with high calcium means more bone loss, more kidney damage, more risk. Routine blood work can catch this early. If you’re over 50, or have a family history, ask your doctor to check your calcium and PTH during your next annual visit. It’s a simple blood test. No fasting needed.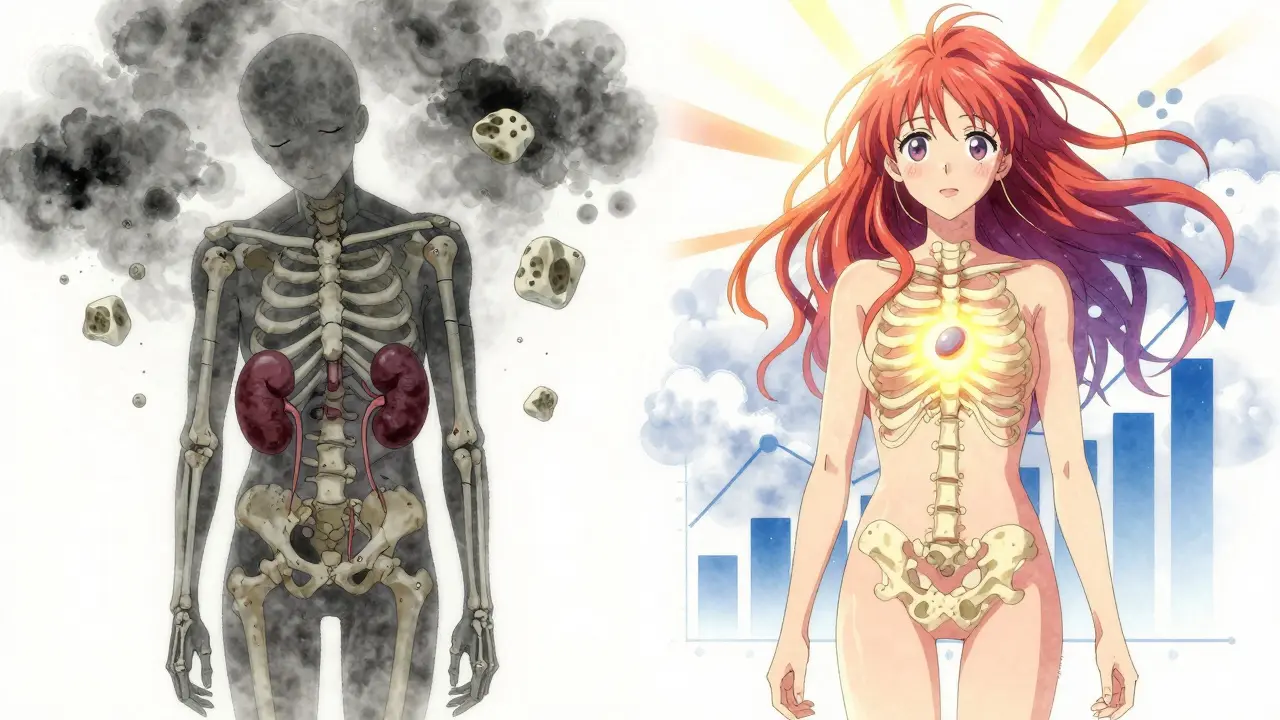
What You Can Do Right Now
If you’ve been told your calcium is high or you’re struggling with unexplained fatigue, bone pain, or kidney stones:- Get a second blood test. One high calcium reading isn’t enough. You need two elevated levels at least a week apart.
- Ask for your PTH level. If it’s normal or high while calcium is high, that’s hyperparathyroidism.
- Request a DXA scan if you’re over 50 or have risk factors.
- See an endocrine surgeon if surgery is recommended. Volume matters-surgeons who do 50+ parathyroidectomies a year have far better outcomes.
- Take vitamin D if you’re deficient. But don’t take extra calcium supplements unless told to. Too much can make things worse.
- Walk daily. Weight-bearing exercise helps protect bone density.
- Avoid thiazide diuretics (like hydrochlorothiazide) if you can. They raise calcium levels.
What’s Changing in 2025
New tools are making diagnosis faster and surgery safer. AI now helps interpret sestamibi scans with 98% accuracy, cutting down false positives. A new drug, etelcalcetide, is showing promise in early trials for primary hyperparathyroidism-though it’s not yet approved for this use. Intraoperative PTH testing is now standard. Surgeons check PTH levels 10 minutes after removing the gland. If it drops by more than 50%, they know they got it all. That’s why cure rates are so high in top centers. Genetic testing is now recommended for anyone diagnosed under 40 or with a family history. About 10% of cases are tied to inherited syndromes like MEN1, which also raise risk for tumors in the pancreas or pituitary. Still, the biggest barrier isn’t technology-it’s awareness. Too many people suffer for years because no one connects the dots.Real Stories, Real Outcomes
A 58-year-old teacher in Ohio had chronic fatigue and kidney stones for eight years. Her calcium was 11.8. PTH was 142. She was told she was “just stressed.” After surgery, her energy returned. Her kidney stones stopped. Her bone density improved by 6% in a year. A 45-year-old man in Texas had back pain and memory lapses. His DXA scan showed osteoporosis at age 45. He thought he was too young. Surgery fixed it. He’s now hiking again. One Reddit user wrote: “I felt like my brain was underwater. After surgery, it was like someone turned on the lights.” These aren’t outliers. They’re the rule-if you act in time.Can hyperparathyroidism go away on its own?
No. The overactive parathyroid gland won’t fix itself. Medications can lower calcium temporarily, but they don’t remove the source. Without surgery, the condition will continue to damage bones, kidneys, and possibly the nervous system. Waiting only increases long-term risk.
Is surgery dangerous? Will I lose my voice?
Voice changes are rare-less than 1% in experienced hands. The nerves controlling the voice run close to the parathyroid glands, but modern techniques and intraoperative monitoring make injury extremely unlikely. Most patients report no change in voice. The risks of untreated hyperparathyroidism-fractures, kidney failure, stroke-are far greater than the risks of surgery.
What if I don’t want surgery?
If you’re not a candidate or choose not to have surgery, you’ll need lifelong monitoring: blood calcium and PTH every 6-12 months, annual DXA scans, and kidney function checks. You’ll also need to avoid dehydration, thiazide diuretics, and excessive calcium supplements. You may need bone-strengthening drugs like bisphosphonates. But you’re still at higher risk for fractures and kidney stones, and symptoms may slowly worsen.
Can diet fix hyperparathyroidism?
No. Diet doesn’t cause or cure it. But what you eat matters. You need 1,200 mg of calcium daily from food (dairy, leafy greens, fortified foods), not supplements. Too much supplemental calcium can make high calcium worse. Vitamin D is important if you’re deficient, but don’t take extra unless your doctor says so. Avoid excessive salt and soda-they increase calcium loss.
How do I know if I have primary, secondary, or tertiary hyperparathyroidism?
It’s all about calcium and PTH levels together. Primary: calcium high, PTH high. Secondary: calcium low or normal, PTH high-common in kidney disease. Tertiary: calcium high, PTH high-but you’ve had kidney disease and a transplant. Your doctor will check your kidney function and medical history to tell the difference. Treatment varies by type.
Write a comment
Items marked with * are required.





11 Comments
Ajay Sangani December 22, 2025 AT 16:44
so like... if your body's just leaching calcium from your bones like it's a vending machine that never runs out, why do we still treat this like it's just 'a lab result'? i mean, we wouldn't ignore a leaky roof and say 'well, the house hasn't collapsed yet'. but we do this all the time with hyperparathyroidism. it's not just bones-it's your brain fog, your chronic tiredness, your kidney stones that feel like internal knives. why is the medical system so slow to connect the dots?
Wilton Holliday December 23, 2025 AT 16:03
THIS. 😊 I had a friend go through this and no one believed her until she collapsed from a stress fracture. She was 42. Thought it was 'just aging' or 'too much coffee'. Turned out her calcium was 12.1 and PTH was 180. Surgery was a miracle-she started hiking again in 3 weeks. Don't wait for a crisis. Get tested. Seriously. 🙏
Abby Polhill December 23, 2025 AT 17:23
Let’s be real-primary hyperparathyroidism is the silent epidemic that gets buried under 'anxiety' or 'chronic fatigue syndrome' because the symptoms are so nonspecific. The jargon-heavy diagnostic criteria (PTH >65 pg/mL + Ca >10.5 mg/dL) are gold standard, but clinicians skip them because they’re not 'sexy' enough. We need more awareness, not just more scans. And yes, the 2022 guidelines are a game-changer-especially for under-50s. This isn’t 'old person disease'. It’s systemic.
Rachel Cericola December 24, 2025 AT 01:44
I’ve been an endocrine nurse for 18 years, and I can tell you this: the single biggest tragedy isn’t the misdiagnosis-it’s the delay. Patients come in with T-scores of -4.2, kidney calcifications, and a history of 7 ER visits for 'migraines'-when it was just brain fog from hypercalcemia. Surgery isn’t risky-it’s restorative. The 95% cure rate? That’s not hype. That’s data. And yes, vitamin D matters-but only if you’re deficient. Taking extra calcium supplements while your glands are overactive is like pouring gasoline on a fire. Don’t self-treat. Get the labs. Then get the surgeon. Period.
Blow Job December 25, 2025 AT 01:03
My cousin had this. She was told she was 'just tired' for five years. Then she broke her wrist lifting a grocery bag. That’s when they checked her calcium. She had a single adenoma. Surgery took 90 minutes. She came home with a Band-Aid and a new life. No more brain fog. No more bone pain. Just… normal. If you’re reading this and you’ve been feeling 'off' for years-get your calcium and PTH checked. It’s a two-minute blood test. Don’t wait for your body to break before you listen.
Christine Détraz December 26, 2025 AT 14:15
I appreciate how this breaks it down without fearmongering. But I also wonder-what about people who can’t afford surgery? Or those without access to endocrine surgeons? The guidelines say 'consider surgery'-but what if you can’t? Lifelong monitoring is exhausting. And bisphosphonates? They come with their own side effects. We need more than just medical advice-we need policy changes too.
EMMANUEL EMEKAOGBOR December 27, 2025 AT 06:04
Esteemed colleagues, I must express my profound appreciation for the clarity and scientific rigor of this exposition. In my homeland of Nigeria, such conditions are frequently misattributed to spiritual afflictions or nutritional deficiencies. The diagnostic criteria you have outlined are not merely clinical-they are emancipatory. May this knowledge reach the rural clinics where patients suffer in silence. The parathyroid glands, though minute, wield immense power over human vitality. Let us not underestimate their significance.
CHETAN MANDLECHA December 27, 2025 AT 09:23
bro this is wild. i had this. didn't know. just thought i was getting old. calcium was 11.9. pth 130. felt like my bones were made of chalk. surgery was quick. now i can run. no more kidney stones. why isn't this on every annual blood panel? someone should make a viral video about this.
Pankaj Chaudhary IPS December 28, 2025 AT 20:44
As a public health advocate, I commend the depth of this post. However, let us not forget the systemic inequities in diagnosis. In India, rural women often present with advanced disease due to lack of screening. We must integrate calcium and PTH testing into primary care protocols, especially for postmenopausal women and those with recurrent nephrolithiasis. Education is not optional-it is a human right. Let us turn awareness into action.
Steven Mayer December 29, 2025 AT 06:46
Interesting. I’ve seen this in my practice. The data is solid. But the emotional toll on patients is rarely discussed. The fatigue isn’t laziness. The brain fog isn’t ADHD. The bone pain isn’t fibromyalgia. And yet, patients are gaslit for years. The real tragedy isn’t the disease-it’s the disbelief. I’ve had patients cry when they finally get a diagnosis. They’ve been told they’re crazy. Or dramatic. Or just stressed. The cure exists. But the validation? That’s still rare.
suhani mathur December 29, 2025 AT 21:11
sooo... you’re telling me that my 7 years of being told 'it's just menopause' was actually my bones dissolving? cool. thanks for the diagnosis, doctor. guess i’ll just go ahead and get surgery now. no biggie. 🙃