Health January 20, 2026
Lithium Carbonate Generics: What You Need to Know About Serum Levels
When you’re managing bipolar disorder with lithium carbonate, it’s not just about taking a pill every day. The real challenge lies in keeping your blood levels just right-too low, and the mood-stabilizing effect fades; too high, and you risk serious side effects. This is especially true when switching between lithium carbonate generics. Even though these are labeled as "bioequivalent," small differences in how they release the drug can throw your levels off balance.
Why Serum Levels Matter More Than You Think
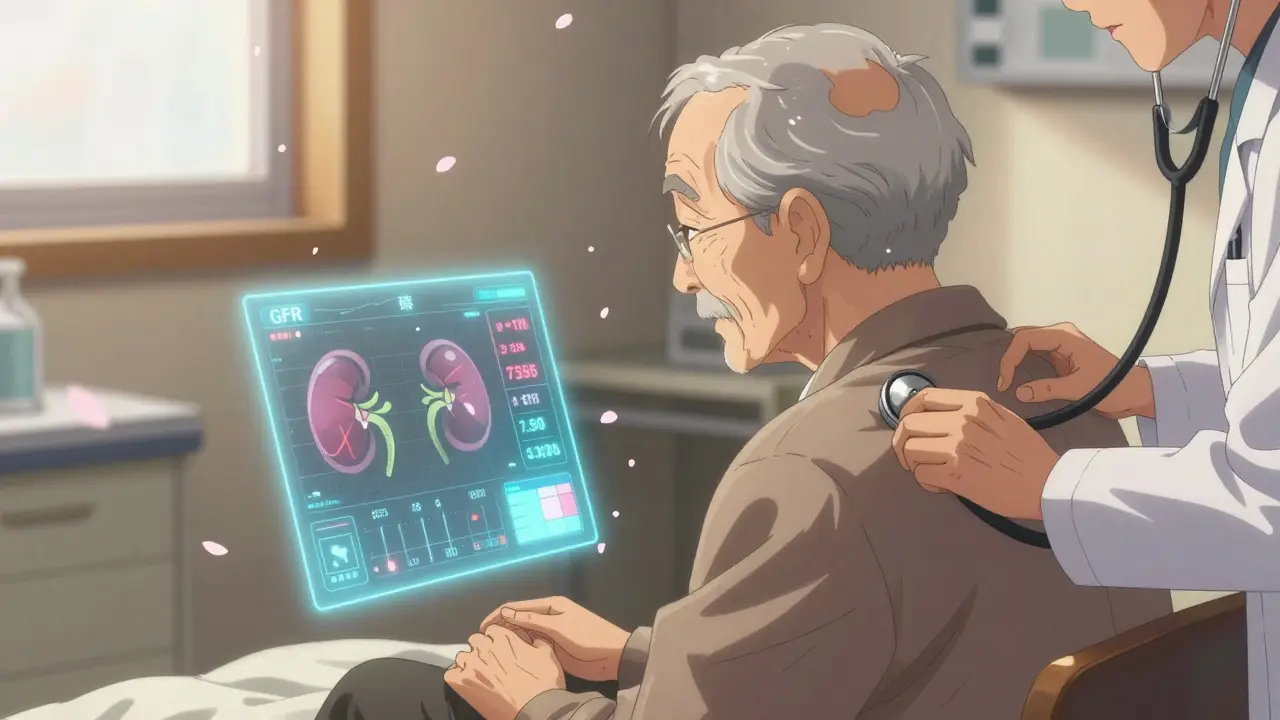
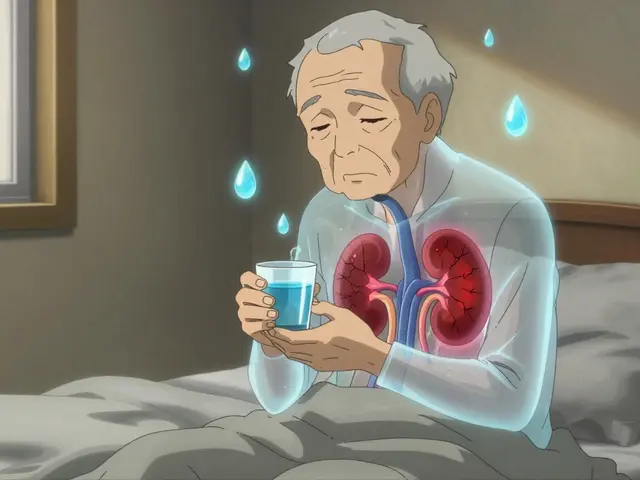
Lithium works by affecting how brain cells communicate, but it doesn’t stay in your body long. It’s cleared through your kidneys, and how fast that happens depends on your age, hydration, kidney function, and even salt intake. The window between effective and dangerous is narrow: 0.6 to 1.2 mmol/L is the standard therapeutic range. Above 1.5 mmol/L, toxicity becomes a real threat. At levels over 2.0 mmol/L, you could face seizures, irregular heart rhythms, or even coma.What most people don’t realize is that this range isn’t one-size-fits-all. For someone in the middle of a manic episode, doctors often aim for 0.8-1.0 mmol/L. Once things stabilize, many experts now recommend lowering it to 0.6-0.8 mmol/L to reduce long-term risks like thyroid damage or kidney strain. Older adults, especially those over 60, may need even lower targets-sometimes 20-25% less-because their kidneys don’t filter lithium as efficiently.
Generics Aren’t All the Same-Here’s Why
You might assume that if two pills are both called "lithium carbonate 300 mg," they’re interchangeable. But that’s not always true. Different manufacturers use different release technologies. Some are immediate-release, meaning the lithium hits your bloodstream fast-within 1 to 2 hours. Others are sustained-release, like Priadel or Camcolit, which slowly leak the drug over 4 to 5 hours.A 2024 study in the Journal of Psychopharmacology found that patients switched from one sustained-release brand to another ended up with 11% higher blood levels-even when the daily dose stayed the same. Four patients in that study saw their lithium levels jump above 1.3 mmol/L after a simple brand switch, with one hitting 1.88 mmol/L. That’s dangerously close to toxic territory.
Why does this happen? Even though generic manufacturers must prove their product is 80-125% as bioavailable as the brand, that’s a wide margin. One pill might release 90% of its lithium in the first 4 hours, while another releases only 60%. That difference might seem small, but for someone on the edge of toxicity, it’s enough to cause problems.
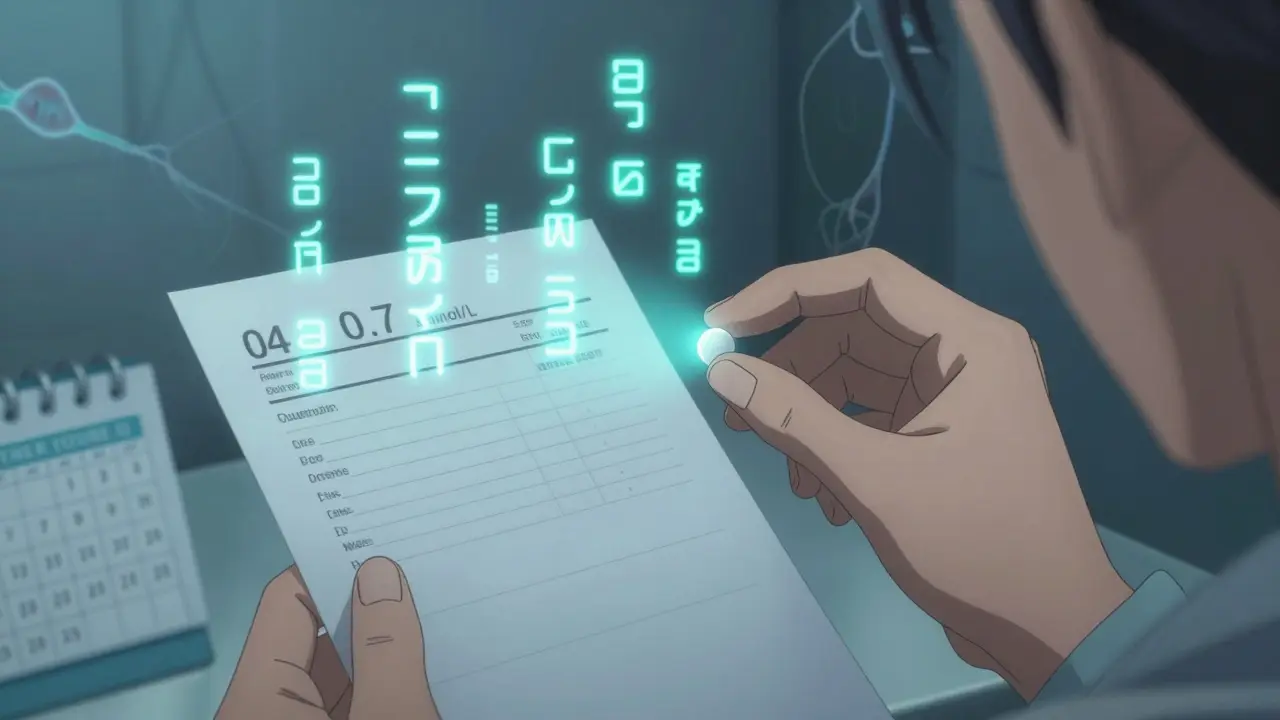
When and How to Check Your Levels
Timing matters. If you’re on a standard-release lithium tablet taken twice or three times a day, your blood test should be done 12 hours after your last dose. That’s when levels stabilize and reflect your true steady-state concentration. If you’re on a once-daily sustained-release formulation, the test should be taken 24 hours after your last dose.Don’t wait until you feel off. Routine monitoring is key. Once you’re stable, check your levels every 3 to 6 months. But if you’ve just started lithium, changed doses, switched brands, or had a major life change (like starting a new medication or losing weight), test weekly or monthly until things settle.
And don’t forget the other tests. Lithium can mess with your thyroid-up to 15% of users develop hypothyroidism. It can also harm your kidneys over time. That’s why doctors check your creatinine and eGFR (estimated glomerular filtration rate) every few months. New guidelines now recommend adding cystatin C to the mix-it’s a more accurate marker of kidney function in older adults or those with muscle loss.

Who’s at Higher Risk?
Some people are naturally more sensitive to lithium’s effects. Women tend to need lower doses than men-even after adjusting for body weight. People over 60 often require 30-40% less lithium than younger adults. In one study, patients over 80 received, on average, 437 mg less per day than those under 30.People with kidney disease, heart conditions, or Brugada syndrome should avoid lithium altogether. Dehydration is another silent danger. If you’re sick with the flu, sweating a lot in hot weather, or cutting back on salt, your lithium levels can spike. Always tell your doctor if you’ve had diarrhea, vomiting, or a fever.
What to Do If You’re Switching Brands
If your pharmacy switches your prescription from Priadel to a generic version-or vice versa-don’t assume everything’s fine. Many patients don’t even know they’ve been switched. Pharmacists are allowed to substitute generics unless the doctor writes "dispense as written."Here’s what you should do:
- Ask your pharmacist: "Is this the same brand I was on before?"
- If it’s different, schedule a serum lithium test within 1-2 weeks.
- Keep track of any new side effects: tremors, frequent urination, nausea, confusion, or muscle weakness.
- Don’t change your dose yourself. Let your doctor adjust based on lab results.
Some clinics now use AI tools that pull data from your electronic health record-your age, weight, kidney function, and past lithium levels-to predict the right dose. These aren’t mainstream yet, but they’re coming. Until then, vigilance is your best tool.
The Bigger Picture: Why Lithium Still Matters
Despite newer drugs like lamotrigine or quetiapine, lithium remains the gold standard for preventing suicide in bipolar disorder. Studies from the 1980s still hold up: people on lithium are half as likely to die by suicide as those on other treatments. It also cuts relapse rates by nearly two-thirds.That’s why, even with all the complexity, over 60% of long-term bipolar patients in the U.S. still take it. The market for lithium is small compared to newer mood stabilizers, but it’s steady-projected to hit $1.2 billion by 2028. And while generics make up most prescriptions today, their variability means you can’t treat them like interchangeable pills.
Final Takeaway: Know Your Numbers
Lithium carbonate isn’t like taking an aspirin. It’s a precision tool. The brand name matters less than the serum level you end up with. Whether you’re on a generic or brand, your job is to know your number. Keep a log of your doses, your blood test results, and any changes in how you feel. Bring that log to every appointment.If you’ve ever been switched to a new generic and suddenly felt foggy, shaky, or unusually tired, don’t brush it off. Ask for a lithium level check. It’s simple, it’s safe, and it could prevent a hospital visit.
Therapy isn’t just about taking pills. It’s about understanding how your body responds to them-and staying in control of the numbers that keep you stable.
Can I switch between lithium carbonate generics without checking my blood levels?
No. Even though generics are required to be bioequivalent, small differences in how they release lithium can cause your blood levels to rise or fall. Studies show that switching brands can lead to clinically significant changes in serum concentration, sometimes pushing levels into the toxic range. Always check your lithium level 1-2 weeks after any brand change.
What’s the safest lithium level for long-term use?
For most adults in maintenance treatment, the safest target is 0.6-0.8 mmol/L. Higher levels (0.8-1.0 mmol/L) may be used during acute episodes but increase long-term risks to the kidneys and thyroid. Older adults and those with reduced kidney function should aim for the lower end of this range. Always follow your doctor’s guidance based on your individual needs.
How often should I get my lithium levels checked?
Once you’re stable, check every 3-6 months. But if you’ve changed doses, switched brands, become ill, started a new medication, or changed your fluid or salt intake, check weekly or monthly until levels stabilize. More frequent monitoring is especially important for people over 60 or with kidney issues.
Does taking lithium affect my kidneys or thyroid?
Yes. Long-term lithium use can reduce kidney function and cause hypothyroidism in 5-15% of users. That’s why regular blood tests for creatinine, eGFR, and thyroid hormones (TSH, free T4) are essential. New guidelines recommend adding cystatin C to kidney monitoring for more accurate results, especially in older adults.
Are there any foods or medications I should avoid with lithium?
Avoid drastic changes in salt intake-low-salt diets can raise lithium levels. Diuretics (water pills), NSAIDs like ibuprofen, and some blood pressure meds (ACE inhibitors, ARBs) can also increase lithium toxicity risk. Always tell your doctor about every medication or supplement you take, including over-the-counter ones.
Is lithium still the best option for bipolar disorder?
For preventing suicide and long-term relapse, yes. No other mood stabilizer has as strong a track record. While newer drugs may have fewer side effects, lithium remains first-line for bipolar I disorder, especially when mood swings are severe. Its effectiveness, low cost, and proven safety over decades make it irreplaceable for many patients-when managed carefully.
Write a comment
Items marked with * are required.





13 Comments
Andrew Rinaldi January 21, 2026 AT 05:31
It's wild how something so simple-taking a pill-can be this delicate. I’ve been on lithium for over a decade, and I still check my levels religiously. Even when I feel fine, I don’t trust the feeling. The body doesn’t lie, but it doesn’t always tell you the truth until it’s too late.
My doc switched me from Priadel to a generic once, and I didn’t notice anything until I started having hand tremors at 3 a.m. Turns out, my level jumped to 1.3. Scary stuff. Now I always ask the pharmacist. Always.
It’s not just about the drug. It’s about knowing your own rhythm-how you sleep, how much water you drink, whether you skipped breakfast. Lithium doesn’t care if you’re having a good day. It just does its thing.
I keep a little notebook. Dose. Date. Level. How I felt. It’s boring, but it’s my lifeline. I’ve saved myself from hospital visits more than once just by catching the drift before it became a wave.
People think mental health meds are magic pills. They’re not. They’re tuning forks. You gotta know the right frequency, or you just get noise.
And yeah, generics? Don’t treat them like interchangeable Legos. Even if the label says the same thing, the story inside can be totally different.
Thanks for writing this. It’s the kind of info that doesn’t get talked about enough.
Gerard Jordan January 21, 2026 AT 21:39
Just wanted to say THANK YOU for this. 🙏 I’ve been on lithium for 8 years and never knew about the cystatin C thing. My doc still just checks creatinine. Gonna bring this up next visit.
Also, I switched generics last month and felt like I was underwater for a week. Foggy. Tired. Like my brain was wrapped in wet socks. Level was 1.28. Scary.
Now I screenshot my prescription every time I refill. No more guessing.
And yes-lithium still saves lives. No other med has ever kept me from ending it all. Period.
💙
lokesh prasanth January 23, 2026 AT 05:11
lithium is just a salt. why is it so hard? people overcomplicate everything. just take the pill. stop being so fragile.
Coral Bosley January 23, 2026 AT 06:49
I can’t believe how many people treat this like it’s just a vitamin. I was on a generic for three months and didn’t realize my levels were creeping up until I had a panic attack so bad I thought I was dying. Turned out I was one point away from toxicity. My therapist said I looked like a ghost.
Now I have a spreadsheet. I track my water intake, my sodium, my sleep, my mood, my level. I cry sometimes just thinking about how much I had to learn just to stay alive.
And yeah, I hate that pharmacists can swap my meds without telling me. It’s not just careless-it’s dangerous. This isn’t aspirin. This is a scalpel. And someone’s handing it to you blindfolded.
Jarrod Flesch January 24, 2026 AT 11:33
Man, I wish I’d known all this when I first started. I was 24, thought I was invincible, and switched generics because it was cheaper. Ended up in the ER with tremors and confusion. Took them 3 days to realize it was lithium. I was lucky.
Now I’m 37, stable, and I still get my levels checked every 3 months. No exceptions. Even if I feel great. Even if I’m on vacation. Even if I’m mad at my doctor.
And yeah, the kidney and thyroid stuff? Real. I’ve got mild hypothyroid now. Took them years to catch it. Don’t wait. Test early, test often.
Also-cystatin C? New to me too. Gonna ask my nephrologist next week. Thanks for the heads up.
Keep sharing this stuff. People need to hear it.
Barbara Mahone January 25, 2026 AT 13:45
There’s a quiet epidemic of undiagnosed lithium toxicity in older adults. My mother was switched to a generic at 72. She started stumbling, forgetting names, losing her appetite. They blamed it on ‘aging.’ It took six months and a fall to get her levels checked. She was at 1.7. She almost didn’t make it.
Doctors need to be more vigilant. And patients? You have to be your own advocate. No one else will do it for you.
This post should be required reading for anyone prescribed lithium. Period.
Kelly McRainey Moore January 27, 2026 AT 04:38
I just started lithium last month and this post is the first thing that actually made me feel less scared. I’ve been checking my levels every week like you said, and keeping notes. It feels weird to be so obsessive, but I’d rather be safe than sorry.
Also, I didn’t know about the salt thing. I’ve been eating a ton of pickles lately because I like them. Now I’m wondering if that’s helping or hurting. 😅
Amber Lane January 28, 2026 AT 07:04
Switched generics last year. Felt off for weeks. Level was 1.25. Doctor said ‘it’s fine.’ I didn’t believe them. Went to a second opinion. They lowered my dose. I felt human again.
Trust your gut. Always.
Ashok Sakra January 29, 2026 AT 02:11
you people are so dramatic. its just a pill. if you cant handle it then dont take it. stop making everything a crisis. lithium is not rocket science. just swallow it and shut up.
michelle Brownsea January 31, 2026 AT 01:09
Let me be perfectly clear: if you’re switching generics without monitoring your serum levels, you are not just being careless-you are endangering your life, and potentially the lives of those around you. This isn’t a ‘maybe’ or a ‘could.’ It’s a documented, preventable medical hazard.
Pharmacists are not trained psychiatrists. They are not responsible for your neurological stability. And yet, they’re being allowed to swap your life-sustaining medication like it’s a brand of toilet paper.
Where is the oversight? Where is the accountability? This is a systemic failure. And until we treat lithium like the precision instrument it is, people will keep ending up in emergency rooms-or worse.
And yes, I’m angry. Because I’ve seen it happen. And no one seems to care enough to fix it.
Kevin Narvaes February 1, 2026 AT 14:44
i used to take lithium back in college. i thought it made me numb. turned out i was just dehydrated and eating low-salt meals. i stopped taking it and felt better. guess i just wasn't meant for it.
but like... why do people make it so complicated? just drink water and don't eat kale all the time.
Philip Williams February 3, 2026 AT 03:35
Thank you for compiling this with such precision. The data on cystatin C as a superior marker for kidney function in elderly patients is particularly compelling. I’m a geriatric nurse practitioner, and I’ve been advocating for this change in our protocols for months. This post gives me the evidence I need to push harder.
Also, the 2024 study cited is critical. We need more real-world pharmacovigilance data like this. Generic substitution isn’t a cost-saving convenience-it’s a clinical variable that must be managed.
I’ll be sharing this with my entire team tomorrow.
Ben McKibbin February 3, 2026 AT 06:00
People act like lithium is some ancient relic. But here’s the truth-it’s still the most effective suicide prevention tool we have. No other drug comes close. Not lamotrigine. Not quetiapine. Not olanzapine.
It’s not perfect. It’s not easy. But it works. And if we keep treating it like a second-class option because it’s cheap and old, we’re abandoning the people who need it most.
Also, the fact that you can switch from Priadel to a generic and suddenly be at 1.88 mmol/L? That’s not a glitch. That’s a failure of regulation.
Let’s stop pretending generics are all the same. They’re not. And pretending they are is how people die.