
Health January 5, 2026
Pediatric Medication Safety: What Parents and Caregivers Need to Know Now
Pediatric Medication Dosing Calculator
Enter Child's Information
Important Safety Information
Recommended Dose:
Enter child's weight to calculate dose
Every year, 50,000 children under age 5 end up in emergency rooms because they got into medicine they shouldn’t have. Many of these cases aren’t accidents-they’re preventable mistakes. Parents aren’t careless. Doctors aren’t negligent. But when you’re dealing with tiny bodies, tiny doses, and tiny mouths, the margin for error is razor-thin. Medication safety for children isn’t just about giving the right pill at the right time. It’s about understanding how a child’s body works differently, how storage mistakes can be deadly in seconds, and how even well-intentioned habits can turn dangerous.
Why Kids Are So Vulnerable to Medication Errors
Children aren’t small adults. Their bodies process medicine in ways that change dramatically as they grow. An infant weighing 3 kilograms might need just 1 milliliter of a liquid antibiotic. A 12-year-old weighing 40 kilograms might need 10 times that. Get the weight wrong, and you could give a lethal dose. In fact, weight-based dosing errors are the leading cause of serious pediatric medication incidents, making up 42% of all reported events.
Even more troubling: children’s livers and kidneys are still developing. They can’t clear drugs as efficiently as adults. A dose that’s perfectly safe for a teenager might build up to toxic levels in a 6-month-old. And because young kids can’t tell you when they feel sick, side effects often go unnoticed until it’s too late. That’s why a child swallowing just one adult aspirin tablet can cause seizures or organ failure.
Home Mistakes That Can Be Deadly
Most pediatric poisonings happen at home-not in hospitals. And the most common culprit? Medicine left within reach.
Parents think they’re being careful. They put pills on the bathroom counter while brushing teeth. They leave vitamins on the nightstand. They store cough syrup in the kitchen cabinet where kids can reach it. But here’s the truth: 75% of poisonings happen because the medicine was stored in a place parents thought was “safe.”
Child-resistant caps aren’t foolproof. A 2013 study found that kids can open bottles that aren’t fully closed in under 30 seconds. And if you remove pills from their original packaging-say, to put them in a pill organizer-you’re making it easier for a child to grab them. In fact, 45% of pediatric pill ingestions involve medicine taken out of child-resistant containers.
And it’s not just pills. Diaper rash cream, eye drops, prenatal vitamins, even liquid vitamins can be deadly in small amounts. These aren’t “harmless supplements.” They’re active drugs. A single dose of iron supplement can kill a toddler.
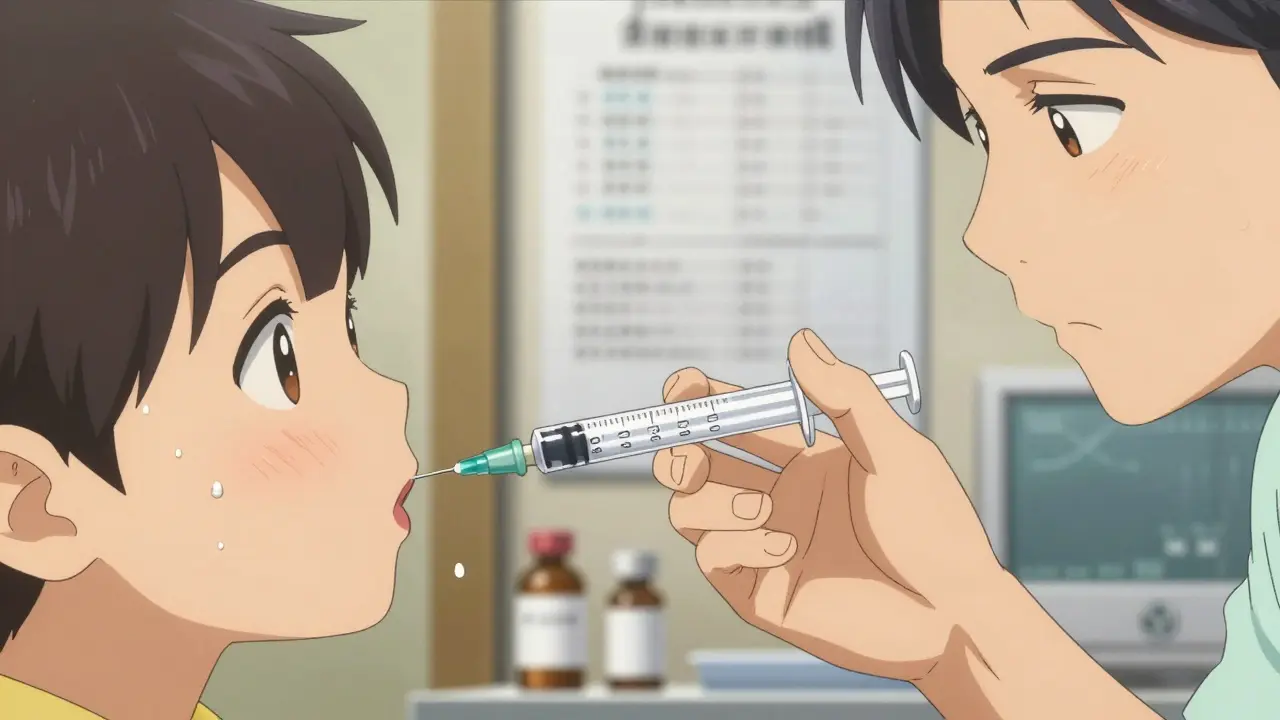
The Dangerous World of Liquid Dosing
One of the most common-and deadliest-mistakes? Using kitchen spoons to measure liquid medicine.
A teaspoon isn’t 5 milliliters? Actually, it is. But a tablespoon is 15 milliliters. That means if you accidentally give a child a tablespoon instead of a teaspoon, you’ve given them three times the dose. If you confuse a teaspoon with a milliliter? That’s a five-fold overdose.
That’s why the American Academy of Pediatrics now recommends: always use milliliter-only dosing devices-oral syringes or dosing cups marked in mL. Never use kitchen spoons. Never guess. Always read the label. And if the medicine comes with a syringe, use it. Even if it’s messy.
Also, never tell a child medicine is “candy.” That’s a common trick to get them to swallow it. But it teaches them that pills are treats. And guess what happens when they’re left unsupervised? They go looking for more. Poison Control data shows this practice contributes to 15% of accidental ingestions.
What Hospitals Are Doing Right
In hospitals, pediatric medication errors are down-because systems have changed.
Children’s hospitals now use kilogram-only dosing in their electronic systems. No pounds. No conversions. Just kilograms. That alone has cut calculation errors by more than half.
High-risk medications-like morphine, insulin, or sedatives-are now given only after a two-provider independent check. One nurse prepares it. Another double-checks the weight, the dose, and the calculation. No shortcuts.
They’ve also created “distraction-free zones” for preparing meds. No phones. No talking. No rushing. Just focus. And they’ve standardized concentrations. Instead of different strengths of the same drug from different manufacturers, they now use one standard concentration. That reduces confusion.
And they train everyone-nurses, doctors, even respiratory therapists-in pediatric dosing. Facilities that did this saw an 85% drop in medication errors.
What You Can Do at Home
Here’s a simple, actionable checklist for every caregiver:
- Store all medicine up and away-not on counters, nightstands, or in purses. Use a locked cabinet or high shelf.
- Always relock child-resistant caps-even if you think you’re just going to the next room.
- Use only milliliter (mL) dosing tools-never spoons. Buy a dosing syringe at the pharmacy if one isn’t included.
- Never call medicine candy. Say “this is medicine, it’s not food.”
- Dispose of expired or unused meds. Don’t keep “just in case” bottles. Take them to a drug take-back program.
- Program 800-222-1222 into your phone as “Poison Help.” Save it in your contacts. Know it by heart.
- Use pictogram instructions-if your pharmacist gives you a sheet with pictures showing when and how to give the medicine, use it. Studies show it improves accuracy by 47%.
- Ask for the teach-back method. After your doctor or pharmacist explains the dose, say, “Can you show me how you’d give this to my child?” Then do it yourself. If you’re unsure, ask again.

What You Should Never Give Your Child
Some medicines have no place in a child’s medicine cabinet.
Over-the-counter cough and cold medicines are not recommended for children under 6-and absolutely forbidden under 2. They don’t work. And they can cause seizures, rapid heart rates, or even death.
Aspirin should never be given to children or teens. It can trigger Reye’s syndrome, a rare but deadly condition that causes liver and brain swelling.
Adult painkillers like ibuprofen or acetaminophen in adult formulations? Only use pediatric versions with clear dosing. Don’t split pills. Don’t guess. Use a syringe.
And don’t assume “natural” means safe. Herbal remedies, essential oils, or homeopathic drops? Many aren’t regulated. Some contain hidden drugs. One child died after being given a “natural” teething gel containing benzocaine.
The Future Is Getting Safer
Change is happening. The FDA now requires drug makers to use standardized concentrations for new pediatric medications. That means less confusion between brands. Less room for error.
More hospitals are adopting the 15 evidence-based safety practices from the American Academy of Pediatrics. And 78% of children’s hospitals already use at least 12 of them.
But the biggest change isn’t in the hospital. It’s in your home. The most effective tool for preventing pediatric medication errors isn’t a new app or a fancy device. It’s awareness. It’s habits. It’s knowing that a child’s body doesn’t handle medicine like yours does-and that safety isn’t optional. It’s non-negotiable.
If you remember one thing: medicines are not toys. They’re powerful tools. And in the wrong hands-or the wrong dose-they can be deadly. Keep them locked. Measure them right. And never, ever assume your child won’t get into them.
Can I use a kitchen spoon to give my child liquid medicine?
No. Kitchen spoons vary in size and aren’t accurate. A teaspoon is 5 milliliters, but a tablespoon is 15 milliliters. Giving a tablespoon instead of a teaspoon means a 3-fold overdose. Always use a dosing syringe or cup marked in milliliters (mL), not teaspoons or tablespoons.
Is it safe to store medicine in the bathroom?
Not recommended. Bathrooms are humid, which can degrade medicine, and they’re often easily accessible to children. Store medicine in a cool, dry place out of reach and sight-like a high cabinet in a bedroom or living room. Never leave medicine on counters or sinks.
What should I do if my child swallows medicine they shouldn’t have?
Call Poison Help at 800-222-1222 immediately. Don’t wait for symptoms. Don’t try to make them vomit. Have the medicine container ready when you call-this helps them identify the substance and dose. If your child is unconscious, having seizures, or having trouble breathing, call 911 right away.
Are child-resistant caps enough to keep kids safe?
No. Child-resistant caps are designed to slow kids down, not stop them. Studies show children can open improperly closed caps in under 30 seconds. Always relock them fully after each use. And never rely on them alone-store medicine up and away, out of sight.
Can I give my 4-year-old adult cough medicine if I cut the dose in half?
Never. Adult cough and cold medicines contain ingredients that can be dangerous-even deadly-to young children. They don’t work better in kids-they work worse and carry higher risks. The FDA and American Academy of Pediatrics strongly advise against using them in children under 6. Use only pediatric-formulated medicines with clear dosing instructions.
Why do hospitals use kilograms instead of pounds for dosing?
Because pound-to-kilogram conversions are one of the most common and dangerous errors in pediatric care. A simple mistake-like thinking 20 pounds is 10 kilograms when it’s actually 9.1-can lead to a 10% overdose. Hospitals use kilograms only to eliminate that risk. Always ask for your child’s weight in kilograms when getting medication instructions.
Are vitamins safe for children to take without supervision?
No. Many vitamins, especially those with iron or vitamin D, can be toxic in small amounts. A single adult iron pill can poison a toddler. Treat vitamins like medicine: store them locked up, give them only as directed, and never let children take them unsupervised.
Final Thought: It’s Not About Being Perfect-It’s About Being Consistent
You don’t have to be a pharmacist to keep your child safe. You just have to be consistent. Lock it up. Measure it right. Don’t guess. Don’t rush. Don’t assume. Every time.
Because in pediatric medication safety, one mistake doesn’t mean you’re a bad parent. It just means you didn’t know. Now you do. And that’s the first step to keeping your child safe.
Write a comment
Items marked with * are required.





8 Comments
Wesley Pereira January 7, 2026 AT 02:38
Man, I thought I was being careful-left the cough syrup on the counter ‘cause I was rushing to answer a call. Then I saw my 3yo holding it like a juice box. Holy shit. This post? 10/10. Weight-based dosing errors? Yeah, I didn’t even know that was a thing. Now I’m using the damn syringe. No more ‘teaspoon’ guesses. Also, locked the cabinet. Even the vitamins. Even the damn iron gummies. 😅
Lily Lilyy January 8, 2026 AT 17:20
Dear friends, every child deserves to grow up safe and healthy. Let us all take a moment to store medicines properly, to measure with care, and to speak gently but firmly to our little ones about what medicine is and what it is not. A locked cabinet is an act of love. A dosing syringe is a promise kept. Thank you for sharing this vital knowledge. We are all in this together. 🌸
Susan Arlene January 9, 2026 AT 12:12
so i used to think ‘child resistant’ meant ‘kid proof’ turns out nope
my cousin’s kid opened a bottle in like 12 seconds
and that was with the cap clicked all the way
now i just keep everything in the closet on the top shelf
and yes i know vitamins can kill
iron is basically poison in a pretty bottle
also never say medicine is candy
my nephew now thinks my inhaler is a snack
we’re working on it
Joann Absi January 11, 2026 AT 01:18
THIS IS WHY AMERICA IS FAILING 😭
Parents are lazy. They leave meds out like it’s a snack drawer. You think your kid’s ‘just curious’? Nah. They’re little predators. And you’re the enabler. 🚫💊
And don’t even get me started on ‘natural’ teething gels. Benzocaine? That’s not herbal. That’s a death wish with a label. 🇺🇸 We need mandatory parenting tests before you get a baby. No joke. #ParentingFail #MedicineIsNotCandy
Jeane Hendrix January 11, 2026 AT 03:55
Just to clarify-when they say ‘kilogram-only dosing,’ does that mean the EHR auto-converts weight from lbs to kg? Or are providers actually required to input kg? Because I’ve seen cases where the system auto-converted 18 lbs to 9 kg (it’s 8.16) and the nurse didn’t catch it. Also, is there a standardized concentration for liquid acetaminophen now? I thought it was still 160mg/5mL vs 80mg/0.8mL depending on the brand. And what about the ‘teach-back’ method? Is that actually being implemented in pediatric clinics, or just the fancy hospitals? Asking for a friend who’s a nurse. 🤔
Gabrielle Panchev January 12, 2026 AT 04:29
Let me just say-this entire post is, frankly, a masterclass in condescension wrapped in a safety pamphlet. You assume that all parents are clueless, that all caregivers are negligent, that all medicine cabinets are chaos zones. But let’s not pretend that the medical-industrial complex isn’t complicit. Why are there still multiple concentrations of pediatric acetaminophen? Why do we still use ‘teaspoon’ on labels when the FDA has known for decades that it’s ambiguous? Why is it still legal to sell liquid ibuprofen in 100mL bottles with no calibrated syringe? And why, in 2024, are we still telling parents to ‘just lock it up’ when the average American household has no lockable cabinet? This isn’t about parenting. It’s about systemic failure dressed up as personal responsibility. And you’re selling it like it’s a virtue.
Saylor Frye January 12, 2026 AT 21:02
Look, I get it. Kids + meds = bad. But let’s be real-most of this is common sense. You don’t leave pills on the counter. You don’t use spoons. You don’t call medicine candy. If you didn’t know that, maybe you shouldn’t be in charge of a child. Also, ‘child-resistant caps’? That’s a marketing term. Like ‘light beer.’ It’s not actually resistant. Just slower. And the 800 number? Yeah, save it. But also, maybe learn CPR. Just saying.
Matt Beck January 14, 2026 AT 11:33
It’s not about the medicine… it’s about the soul. 🌌
Every pill is a whisper from the universe: ‘you are responsible.’
When you leave a bottle on the counter, you’re not just being careless-you’re rejecting the sacred contract of parenthood.
The child doesn’t know the difference between candy and medicine… because you taught them to see the world as a buffet.
Lock it up? Yes. But also… lock your fear. Lock your guilt. Lock your exhaustion.
Because safety isn’t a checklist.
It’s a meditation.
And if you’re not meditating on every dose…
you’re not parenting.
You’re just… existing.
🪷💊