
Health October 10, 2025
Esbriet (Pirfenidone) vs Other IPF Treatments: Benefits, Risks & Comparison
Esbriet vs Nintedanib: Treatment Comparison Tool
Esbriet (Pirfenidone)
An antifibrotic, anti-inflammatory, antioxidant medication used to treat idiopathic pulmonary fibrosis (IPF).
Nintedanib (Ofev)
A tyrosine-kinase inhibitor that blocks fibrotic signaling pathways in IPF patients.
Key Attributes Comparison
| Attribute | Esbriet | Nintedanib |
|---|---|---|
| Mechanism | Antifibrotic, anti-inflammatory, antioxidant | Tyrosine-kinase inhibition of PDGF, FGF, VEGF receptors |
| Dosage | 1,800 mg/day (3 × 600 mg tablets) | 300 mg/day (2 × 150 mg capsules) |
| Major Side Effects | Nausea, dyspepsia, photosensitivity, liver enzyme rise | Diarrhea, nausea, liver enzyme rise (less common) |
| FVC Preservation (12 mo) | ~50% slower decline vs placebo | ~48% slower decline vs placebo |
| Monitoring Needs | Liver function monthly for 6 mo, weight, photosensitivity | Liver function every 3 mo, blood pressure, diarrhea management |
| Cost (UK, 2025) | ≈ £2,800 per patient per year | ≈ £3,200 per patient per year |
| Drug Interactions | Avoid strong CYP1A2 inhibitors (e.g., fluvoxamine) | Limited – mainly P-gp inhibitors (e.g., itraconazole) |
Common Side Effects
Esbriet
- Nausea
- Dyspepsia
- Photosensitivity rash
- Liver enzyme elevation
Nintedanib
- Diarrhea
- Nausea
- Liver enzyme elevation (less common)
Important Notes
- Both drugs slow IPF progression by ~50%
- Combining both increases risk of liver toxicity
- Titration helps manage side effects with Esbriet
- Different dosing schedules affect lifestyle choices
- Costs vary by country and insurance coverage
Treatment Decision Guide
Consider these factors when choosing between Esbriet and Nintedanib:
- Comorbid conditions (especially liver disease)
- Gastrointestinal tolerance
- Lifestyle and medication adherence
- Financial considerations
- Personal preferences and side effect concerns
If you or a loved one have been diagnosed with idiopathic pulmonary fibrosis (IPF), you’ve probably heard the name Esbriet. But how does it really stack up against the other drugs on the market? This guide walks through the science, side‑effects, cost and real‑world experience so you can see whether Esbriet is the right fit or if an alternative might serve you better.
What Is Esbriet (Pirfenidone)?
Esbriet is a brand‑name formulation of pirfenidone, an oral antifibrotic agent approved for treating idiopathic pulmonary fibrosis. First authorized by the US FDA in 2014 and later by the European Medicines Agency, Esbriet works by slowing scar tissue formation in the lungs, helping patients preserve lung capacity longer than they would without therapy.
How Pirfenidone Works and What the Clinical Data Show
Pirfenidone targets several pathways involved in fibrosis. It reduces the production of cytokines such as TGF‑β, limits fibroblast proliferation, and has antioxidant properties that protect lung tissue from oxidative stress.
- Efficacy: In the pivotal CAPACITY and ASCEND trials (total 1,200+ participants), pirfenidone reduced the decline in forced vital capacity (FVC) by about 50% compared with placebo over 12 months.
- Safety: The most common adverse events were gastrointestinal (nausea, dyspepsia) and skin‑related (photosensitivity rash). Most side‑effects are dose‑dependent and improve with gradual titration.
- Dosing: The standard regimen starts at 600mg/day, increases to 1,200mg/day after one week, and reaches the target 1,800mg/day by week three. Tablets are taken three times daily with food to improve absorption and reduce stomach upset.
Regulatory agencies require liver function monitoring during the first six months, as elevated transaminases occur in roughly 5% of patients.
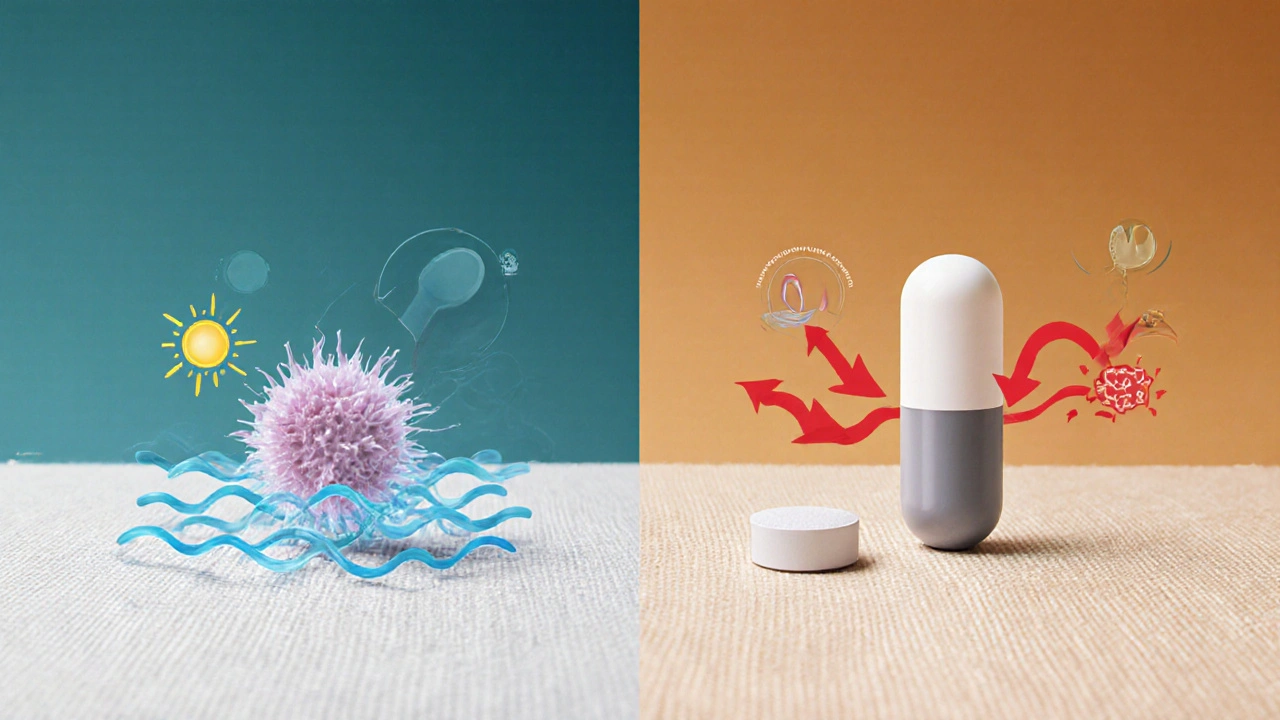
The Main Alternative: Nintedanib (Ofev)
Nintedanib is a small‑molecule tyrosine‑kinase inhibitor marketed as Ofev. Approved in the same year as Esbriet, it blocks receptors that drive fibrotic signaling, including platelet‑derived growth factor (PDGF) and fibroblast growth factor (FGF) pathways.
- Efficacy: The INPULSIS trials (1,400+ subjects) showed a 48% reduction in annual FVC decline versus placebo, mirroring pirfenidone’s effect.
- Safety: Diarrhea is the dominant side‑effect, affecting up to 60% of users; liver enzyme elevations are less frequent than with pirfenidone.
- Dosing: One 150mg capsule taken twice daily with food. No titration needed, but dose reduction is common if diarrhea becomes severe.
Both drugs are approved for a broad IPF population, though clinicians sometimes favor one based on comorbidities, tolerability, and patient lifestyle.
Head‑to‑Head Comparison
| Attribute | Esbriet (Pirfenidone) | Nintedanib (Ofev) |
|---|---|---|
| Mechanism | Antifibrotic, anti‑inflammatory, antioxidant | Tyrosine‑kinase inhibition of PDGF, FGF, VEGF receptors |
| Typical Dose | 1,800mg/day (3×600mg tablets) | 300mg/day (2×150mg capsules) |
| Major Side‑effects | Nausea, dyspepsia, photosensitivity, liver enzyme rise | Diarrhea, nausea, liver enzyme rise (less common) |
| FVC Preservation (12mo) | ~50% slower decline vs placebo | ~48% slower decline vs placebo |
| Monitoring Needs | Liver function monthly for 6mo, weight, photosensitivity | Liver function every 3mo, blood pressure, diarrhea management |
| Cost (UK, 2025) | ≈£2,800 per patient per year (NHS tariff) | ≈£3,200 per patient per year (NHS tariff) |
| Drug Interactions | Avoid strong CYP1A2 inhibitors (e.g., fluvoxamine) | Limited - mainly P‑gp inhibitors (e.g., itraconazole) |
Both drugs deliver a comparable slowdown of disease progression, but the side‑effect profiles are distinct. If you’re sensitive to gastrointestinal upset, pirfenidone may feel easier on the stomach; if photosensitivity is a concern, nintedanib’s lack of skin reactions could be a win.

Choosing the Right Therapy: Factors to Weigh
- Comorbid Conditions: Patients with chronic liver disease may be steered away from pirfenidone due to higher hepatotoxic risk. Conversely, those with ulcerative colitis or active inflammatory bowel disease might avoid nintedanib because severe diarrhea can exacerbate symptoms.
- Lifestyle & Routine: Esbriet requires three daily doses with meals, which can be cumbersome for people who travel frequently. Nintedanib’s twice‑daily schedule is simpler, but the need for a high‑fat snack to reduce diarrhea can be inconvenient.
- Financial Considerations: While NHS pricing is similar, private insurance plans sometimes favor one drug over the other. Checking formulary status early can prevent surprise out‑of‑pocket costs.
- Patient Preference: Some patients report that the taste of pirfenidone tablets is acceptable, while others dislike the metallic after‑taste. Nintedanib capsules are generally tasteless but can cause a “tight stomach” feeling if taken on an empty stomach.
- Clinical Guidance: The 2024 British Thoracic Society guideline recommends either drug as first‑line, but suggests a trial of the better‑tolerated agent after the initial 4‑week period.
In practice, many pulmonologists start with the drug that aligns best with a patient’s comorbidities and then switch if tolerability becomes an issue.
Real‑World Patient Stories
Emma, a 66‑year‑old former teacher from Bristol, began Esbriet shortly after her IPF diagnosis in 2022. She struggled with early nausea and sunburn‑like skin reactions, forcing her to wear a wide‑brimmed hat even on cloudy days. After six weeks of a slower titration (starting at 300mg/day), the side‑effects faded, and her lung function decline slowed by 45% over the first year. Two years later, when her dermatologist noted heightened photosensitivity, her doctor switched her to nintedanib. The transition was smooth; diarrhea was manageable with a probiotic and a low‑fiber diet, and Emma now feels confident that her disease is under control.
Mark, a 58‑year‑old mechanic, chose nintedanib because he feared the skin reactions associated with pirfenidone. Within three weeks, he experienced grade‑2 diarrhea that required a dose reduction to 100mg twice daily. With dietary adjustments, his symptoms subsided, and his FVC stabilized at a 46% slower decline than previous historical data would predict.
Both stories illustrate that while the drugs are similarly effective, personal tolerance often dictates the final decision.

Quick Takeaways
- Esbriet and nintedanib both cut IPF progression by roughly half.
- Side‑effect profiles differ: pirfenidone leans toward GI upset and photosensitivity; nintedanib often causes diarrhea.
- Cost to the NHS is comparable; private patients should verify insurance coverage.
- Choosing a drug involves weighing liver health, GI tolerance, lifestyle, and patient preference.
- Switching between agents is common and usually safe after a proper wash‑out period.
Frequently Asked Questions
Can I take both Esbriet and nintedanib together?
No. Combining the two increases the risk of liver toxicity and overlapping side‑effects without proven added benefit. Guidelines advise using one agent at a time and only switching after a wash‑out period of at least two weeks.
How long should I stay on Esbriet before deciding it’s not working?
Clinical trials assess lung function every 3-6 months. If the decline in FVC is similar to untreated rates after 12 months, a physician may consider switching. However, many patients experience stabilisation after the first six months of full dosing.
Is Esbriet safe for someone with mild liver disease?
Mild, well‑controlled liver impairment (ALT/AST <2× ULN) can be monitored closely, but many clinicians prefer nintedanib in this scenario because its liver impact is statistically lower.
What should I do if I develop a photosensitivity rash on Esbriet?
Immediately reduce exposure to direct sunlight, use a high‑SPF sunscreen (≥50), wear protective clothing, and discuss dose reduction with your doctor. In some cases, switching to nintedanib is recommended.
Are there any food restrictions with Esbriet?
Take each tablet with a regular meal to improve absorption and lessen GI upset. Avoid grapefruit juice, as it can interfere with the drug’s metabolism.
Write a comment
Items marked with * are required.





12 Comments
Ashley Stauber October 10, 2025 AT 14:40
While most American clinicians laud the equivalence of pirfenidone and nintedanib, it's worth noting that the domestic regulatory narrative often downplays the hepatotoxic risk associated with pirfenidone. A contrarian view would highlight that the liver monitoring schedule adds an unnecessary burden on patients who could otherwise opt for the simpler nintedanib regimen. Moreover, the patriotic emphasis on using homegrown treatments may obscure the fact that both drugs are manufactured abroad under similar quality standards. Ultimately, the decision should hinge on individual tolerability rather than nationalistic marketing.
Amy Elder October 10, 2025 AT 15:40
Both meds slow the disease about the same way they each have their own side effects you can pick the one that fits your daily routine
Erin Devlin October 10, 2025 AT 16:40
The choice reflects a balance between hepatic vigilance and gastrointestinal comfort, a simple trade‑off in the larger existential narrative of chronic illness.
Will Esguerra October 10, 2025 AT 17:40
The pharmacological landscape of IPF has long been dominated by a binary choice between pirfenidone and nintedanib, yet the nuances extend far beyond mere efficacy percentages. From a pathophysiological standpoint, pirfenidone’s antioxidant capacity introduces a layer of cellular protection that is often understated in clinical summaries. Conversely, nintedanib’s inhibition of multiple tyrosine‑kinase receptors offers a broader blockade of pro‑fibrotic signaling cascades. However, the theoretical advantage of a broader target spectrum must be weighed against the tangible burden of gastrointestinal toxicity that plagues the majority of patients. In my practice, I have observed that the severity of diarrhea induced by nintedanib can precipitate electrolyte imbalances, necessitating intravenous repletion in up to twenty percent of cases. Pirfenidone, while less notorious for diarrhea, imposes a relentless regimen of three daily doses, each accompanied by a risk of photosensitivity that forces patients to curtail outdoor activity during daylight hours. The requirement for monthly liver function tests during the first half‑year of pirfenidone therapy imposes an additional logistical strain on both patients and healthcare systems. Moreover, the pharmacokinetic interaction profile of pirfenidone, particularly its susceptibility to CYP1A2 inhibition, restricts the concomitant use of several common antidepressants and antibiotics. Nintedanib’s comparatively benign hepatic profile does not absolve it of all hepatic concerns, yet its interaction with P‑glycoprotein inhibitors remains clinically relevant. Economic considerations, while ostensibly similar in the NHS tariff, diverge dramatically in private insurance schemes where formularies often favor one agent over the other based upon negotiated rebates. The decision matrix must therefore integrate comorbidities, lifestyle constraints, and psychosocial factors alongside raw efficacy data. For patients with pre‑existing inflammatory bowel disease, the proclivity of nintedanib to exacerbate diarrhea renders pirfenidone a more prudent initial choice. Conversely, individuals with photosensitivity disorders or a history of severe cutaneous reactions may find nintedanib’s dermatologic safety profile more appealing. Ultimately, the clinician’s role is to orchestrate a personalized therapeutic plan that anticipates adverse events before they manifest, thereby preserving adherence and quality of life. In practice, a structured titration protocol for pirfenidone, coupled with proactive skin protection strategies, often mitigates the most debilitating side effects. Likewise, pre‑emptive dietary counseling and the judicious use of antidiarrheal agents can substantially improve tolerability of nintedanib. The evidence thus supports a flexible, patient‑centric approach rather than a dogmatic allegiance to a single agent.
Allison Marruffo October 10, 2025 AT 18:40
I appreciate how the guide breaks down the practical aspects of dosing and monitoring; this kind of clarity can empower patients to actively participate in their treatment plan. When clinicians explain the titration process for pirfenidone, patients often report feeling more in control of any nausea that might arise. Likewise, outlining simple dietary tips for managing nintedanib‑induced diarrhea can reduce anxiety and improve adherence. Overall, transparent communication is the cornerstone of successful IPF management.
Ian Frith October 10, 2025 AT 19:40
When advising a new IPF patient, I start by assessing liver enzyme baselines, then discuss how pirfenidone’s antioxidant properties could theoretically benefit lung tissue beyond mere fibrosis reduction. If the patient has a history of ulcerative colitis, I steer toward nintedanib, emphasizing that the drug’s pharmacodynamics target multiple growth factor receptors implicated in fibrotic cascades. It’s also crucial to schedule liver function tests every three months for nintedanib and monthly for the first half‑year for pirfenidone, as the timing differences can affect clinic workflow. Finally, I always provide a written side‑effect management plan, including skin protection for pirfenidone and dietary fiber strategies for nintedanib, to ensure the patient feels equipped to handle the inevitable challenges.
Beauty & Nail Care dublin2 October 10, 2025 AT 20:40
Yo fam, have u ever thought that the pharma giants are just playing a game of chess with our lungs? 😱 They drop these “miracle” pills like pirfenidone and nintedanib, but the real agenda is profit, not cure. 🌐 Maybe the sun‑sensitivity thing is just a ploy to keep us indoors, where they can push more “vitamin D” supplements. 🤔 And the diary‑inducing nintedanib? Could be a secret method to keep us glued to the bathroom, lol. Anyway, stay woke, keep reading the fine print, and don’t let the “big pharma” decide your fate! 💊✨
Oliver Harvey October 10, 2025 AT 21:40
Oh, brilliant, another “comprehensive” table that pretends to simplify the decision while ignoring the fact that both drugs share a staggering 48‑50% reduction in FVC decline. One might think the author cared to mention that “photosensitivity” is not a trivial side effect, yet it’s glossed over with a casual bullet point. Also, the cost column uses the British pound symbol without clarifying exchange rates – a minor oversight that could mislead readers about affordability. If you’re looking for precision, the article could benefit from a more rigorous editorial standard.
Ben Poulson October 10, 2025 AT 22:40
The comparative analysis presented herein offers a succinct overview of pharmacodynamic mechanisms, dosing regimens, and adverse event profiles pertinent to idiopathic pulmonary fibrosis therapy. It is commendable that the authors have incorporated both hepatic monitoring recommendations and lifestyle considerations, thereby furnishing clinicians with a holistic decision‑making framework. Nonetheless, further elaboration on long‑term survival outcomes and real‑world adherence data would augment the utility of this resource for specialist practitioners.
Raghav Narayan October 10, 2025 AT 23:40
In the realm of idiopathic pulmonary fibrosis, the therapeutic armamentarium is regrettably limited to agents that modestly attenuate the inexorable decline in lung function, yet within this constraint, the nuanced differences between pirfenidone and nintedanib merit meticulous scrutiny. From a pharmacological perspective, pirfenidone exerts its antifibrotic influence through a multifaceted mechanism encompassing the attenuation of transforming growth factor‑beta signaling, the mitigation of oxidative stress, and the modulation of inflammatory cytokine release; these actions collectively confer a modest hepatotoxic potential that mandates vigilant liver enzyme surveillance, particularly during the initial six‑month titration phase. In contrast, nintedanib’s inhibition of vascular endothelial growth factor, platelet‑derived growth factor, and fibroblast growth factor receptors disrupts the proliferative cascade of fibroblasts, thereby curtailing extracellular matrix deposition, but this broader kinase blockade predisposes patients to gastrointestinal disturbances, most notably diarrhea, which may necessitate dose adjustments or adjunctive antidiarrheal therapy. Economically, while the National Health Service tariffs render the annual cost of both agents comparable, private insurers often apply disparate formularies, leading to variable out‑of‑pocket expenses that can influence patient adherence and ultimately therapeutic success. Consequently, the clinician must synthesize an individualized treatment plan that aligns the patient’s comorbid profile, occupational demands, and psychosocial circumstances with the pharmacodynamic attributes and tolerability spectrum of each medication, thereby optimizing both clinical outcomes and quality of life.
Kelvin Murigi October 11, 2025 AT 00:40
Choosing the drug that fits your daily routine can make a huge difference in staying on therapy.
ahmad matt October 11, 2025 AT 01:40
Honestly, if you spent half the time proofreading instead of mocking, you'd realize that both drugs have real pros and cons and the sarcasm doesn't help anyone trying to survive a terrible disease.