
Health December 1, 2025
Understanding Controlled Substance Labels and Schedule Codes
When you pick up a prescription at the pharmacy, the label on the bottle might look like any other. But if it’s a controlled substance, that label carries legal weight-and the code on it tells the pharmacist, the DEA, and even you how strictly the drug is regulated. The difference between a Schedule II and a Schedule V drug isn’t just about strength. It’s about how it’s prescribed, how many times you can refill it, and whether the pharmacy needs to keep a special log. Understanding these labels isn’t just for doctors and pharmacists. If you’re taking painkillers, anxiety meds, or sleep aids, you need to know what those letters and numbers mean.
What Are Controlled Substances?
A controlled substance is any drug or chemical regulated by the federal government under the Controlled Substances Act (CSA) of 1970. This law doesn’t just ban drugs-it creates a tiered system to manage how they’re made, sold, prescribed, and tracked. The goal? To stop abuse while still letting patients get the medicines they need. The DEA, which stands for Drug Enforcement Administration, runs this system. Every controlled substance gets a unique code number, and it’s placed into one of five schedules based on its risk.
Not all drugs are controlled. Aspirin, antibiotics, and blood pressure pills aren’t on the list. But opioids like oxycodone, benzodiazepines like Xanax, and even some cough syrups with codeine are. The DEA decides which drugs go where based on three things: how likely they are to be abused, how addictive they are, and whether they have any medical use at all. A drug with no medical use and high abuse potential? That’s Schedule I. A drug with low abuse risk and proven medical use? That’s Schedule V.
The Five Schedules Explained
Each schedule has its own rules-and those rules show up on your prescription label.
- Schedule I: These drugs have no accepted medical use in the U.S. and a high potential for abuse. Examples include heroin, LSD, and (as of 2025) marijuana under federal law. You can’t get a prescription for these. They’re illegal everywhere, even in states where medical or recreational cannabis is legal.
- Schedule II: These drugs have high abuse potential but are used medically. They can lead to severe physical or psychological dependence. Common examples: oxycodone (OxyContin), fentanyl, morphine, Adderall, and methadone. These prescriptions can’t be refilled. If you run out, you need a brand-new prescription from your doctor. In most states, they must be written on special tamper-resistant paper or sent electronically through a secure system.
- Schedule III: These have moderate to low abuse potential. They’re less likely to cause dependence than Schedule II drugs. Examples include ketamine, anabolic steroids, and hydrocodone combined with acetaminophen (like Vicodin). You can get up to five refills within six months. Electronic prescriptions are allowed.
- Schedule IV: These have low abuse potential. They’re widely prescribed for anxiety and sleep disorders. Examples: Xanax (alprazolam), Valium (diazepam), Ambien (zolpidem), and tramadol. Like Schedule III, you can refill up to five times in six months. Most are prescribed electronically.
- Schedule V: These have the lowest abuse potential. Some can even be bought over the counter with pharmacist approval. Examples include cough syrups with less than 200 mg of codeine per 100 ml, and antidiarrheal meds with atropine/diphenoxylate. Refills are often allowed without strict limits.
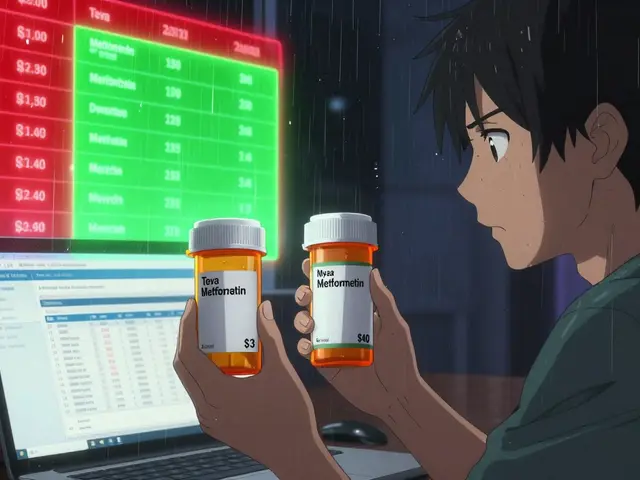
Here’s the catch: the same drug can be in different schedules depending on how it’s made. Codeine is a perfect example. Pure codeine? Schedule II. Codeine mixed with acetaminophen in a tablet? Schedule III. Codeine in a weak cough syrup? Schedule V. The label on your bottle will show the schedule code-usually listed as “CSA SCH II” or “CSA SCH IV.”
What You’ll See on the Label
Your prescription label doesn’t just say “Take one pill daily.” It also includes regulatory markings. Look for:
- CSA SCH II or CSA SCH IV - This tells you the schedule. Pharmacies use this to know how to handle the prescription.
- NARC - Stands for Narcotic. You’ll see this on opioids like oxycodone or hydrocodone.
- Controlled Substance - A clear warning that federal rules apply.
- DEA Number - Your doctor’s registration number, printed on the prescription. It starts with two letters (like “AB” or “MC”) followed by seven digits. This proves the prescriber is authorized to write controlled substance prescriptions.
Pharmacists check these details every time. If the DEA number is missing, the schedule code is wrong, or the prescription looks altered, they can’t fill it. For Schedule II drugs, the original paper prescription is required in most states. No emails, no texts, no phone calls from the doctor will do.

Why the System Matters
This isn’t bureaucracy for bureaucracy’s sake. The system tracks who gets what, how much, and when. In 2022, pharmacists reported that Schedule III-V drugs made up over 92% of all controlled substance prescriptions. Hydrocodone combinations (Schedule III) were the most commonly dispensed. But Schedule II drugs-like opioids-trigger the most scrutiny. One oncology nurse said processing a single Schedule II prescription takes 15 minutes longer than a regular one, just because of the extra paperwork and verification steps.
The system helps prevent “doctor shopping”-where someone visits multiple doctors to get multiple prescriptions. Pharmacies share data through state prescription monitoring programs (PMPs). If you’re getting oxycodone from three different doctors in a month, the system flags it. That’s why you can’t refill Schedule II meds: it forces you to go back to your doctor, who can check if you’re still needing it or if something’s wrong.
Where the System Falls Short
But the system isn’t perfect. Cannabis is the biggest example. It’s still federally classified as Schedule I-meaning no medical use and high abuse potential. Yet 38 states allow medical marijuana. That creates confusion. A patient can legally get a cannabis card in California but still face federal penalties if they cross state lines. Experts agree: the current system doesn’t reflect modern science. The American Medical Association and the Rand Corporation both say it’s outdated.
Even more troubling: some Schedule IV drugs like Xanax have a higher abuse rate than certain Schedule III drugs. Yet the rules are looser for Schedule III. Critics say the system is based more on history than data. In 2023, the Department of Health and Human Services recommended moving cannabis to Schedule III. If that happens, it could be the first major change since 1970. Analysts predict more reschedulings in the next few years.

What You Should Do
If you’re prescribed a controlled substance:
- Check the label. Look for “CSA SCH” and the number. Know what schedule you’re on.
- Know your refill rules. Schedule II? No refills. Schedule IV? Up to five refills in six months.
- Keep your prescriptions safe. Never share them. Don’t let others use your meds.
- Ask questions. If you don’t understand why your painkiller can’t be refilled, ask your pharmacist. They’re trained to explain this.
- Report lost or stolen prescriptions. If your Schedule II prescription is stolen, tell your doctor and pharmacist immediately. It’s not just about safety-it’s the law.
For prescribers, the learning curve is steep. Doctors spend an average of 12.5 hours learning controlled substance rules during residency. Many make mistakes in documentation. A 2022 DEA audit found 43% of violations were due to incomplete records for Schedule II prescriptions. That’s why electronic prescribing systems are now required in most cases-they reduce errors and speed up the process.
What’s Changing?
The DEA is under pressure to modernize. In 2021, they launched the Controlled Substance Ordering System (CSOS), which cut processing times for Schedule II orders from days to under 24 hours. They’re also trying to reduce the time it takes to schedule new drugs-from two years down to one. And with the potential rescheduling of cannabis, the entire framework could shift.
Experts believe we’ll see more nuanced categories in the future. Some suggest a six- or seven-schedule system to better reflect the differences between drugs. Right now, the system treats all Schedule IV drugs the same-even though, say, a sleeping pill and a sedative can have very different abuse patterns.
The bottom line? Controlled substance labels aren’t just paperwork. They’re a legal map. They tell you what you’re allowed to do, how often you can get your medicine, and why the system treats some drugs more strictly than others. Knowing what those labels mean helps you stay compliant, stay safe, and get the care you need without unnecessary barriers.
What does CSA SCH II mean on a prescription label?
CSA SCH II stands for Controlled Substances Act Schedule II. It means the drug has a high potential for abuse and can lead to severe physical or psychological dependence, but it has accepted medical uses. Examples include oxycodone, fentanyl, and Adderall. Prescriptions for Schedule II drugs cannot be refilled and must be written on special tamper-resistant paper or sent electronically. In most states, a paper prescription is required, and the original must be presented to the pharmacy.
Can you refill a Schedule II prescription?
No, you cannot refill a Schedule II prescription. Federal law prohibits refills for these drugs because of their high risk of dependence. If you need more medication, your doctor must write a new prescription. This rule is designed to prevent misuse and ensure ongoing medical oversight. Even if you’re taking the same dose for chronic pain, you still need a new prescription each time.
Why is codeine sometimes Schedule III and sometimes Schedule V?
Codeine’s schedule depends on its concentration and what it’s mixed with. Pure codeine is Schedule II because it’s potent and highly addictive. When combined with acetaminophen in tablets (like in Vicodin), it becomes Schedule III because the combination reduces abuse potential. In low-dose cough syrups (less than 200 mg of codeine per 100 ml), it’s Schedule V because the amount is so small that dependence risk is minimal. The label will show the exact schedule based on the formulation.
Are all opioids Schedule II?
Most strong opioids like oxycodone, hydrocodone (in higher doses), morphine, and fentanyl are Schedule II. But not all opioids fall into that category. Codeine in low-dose cough syrups is Schedule V, and tramadol-a weaker opioid-is Schedule IV. The schedule depends on the drug’s potency, abuse potential, and how it’s formulated. Always check the label to know the exact schedule.
Why does the DEA control prescription labels?
The DEA controls prescription labels to track the flow of drugs that can be abused or lead to addiction. This creates a “closed system” where every step-from manufacturer to pharmacy-is documented. This helps prevent diversion (like selling pills illegally), doctor shopping, and overdose. The label includes the DEA number of the prescriber, the schedule code, and other details so pharmacies and regulators can verify the prescription is legal and legitimate.
If you’re unsure about your medication’s schedule, ask your pharmacist. They can explain the rules and help you avoid violations. Understanding these labels isn’t about memorizing laws-it’s about staying safe and getting the care you need without unintended consequences.
Write a comment
Items marked with * are required.



10 Comments
Rachel Stanton December 2, 2025 AT 08:55
CSA SCH II labels are a lifeline for patients who need strict oversight-like those with chronic pain or ADHD. But the system’s rigidity often ignores individual needs. I’ve seen patients go without meds for days because a doctor’s office was closed on a Friday. The DEA’s paperwork maze doesn’t protect people-it punishes them for being human. Electronic prescribing helps, but it’s still a band-aid on a broken system.
Edward Hyde December 3, 2025 AT 14:08
This whole schedule thing is a joke. Schedule II? More like Schedule ‘Why Are You Making Me Jump Through Hoops?’ I got a 30-day script for oxycodone after back surgery and had to beg my doc to reissue it because the pharmacy wouldn’t accept a digital copy. Meanwhile, my buddy buys Xanax off Instagram like it’s a TikTok trend. The system’s rigged. It targets the sick, not the addicts.
Kenny Leow December 3, 2025 AT 15:54
As someone who’s lived in 5 countries, I’ve seen how other nations handle this. In Germany, they use a tiered digital registry that auto-alerts doctors if someone’s getting multiple scripts. No paper. No panic. Just data. The U.S. still relies on fax machines and handwritten DEA numbers. It’s like trying to stream 4K on a dial-up connection. We’re not just behind-we’re stuck in 1997.
Erin Nemo December 4, 2025 AT 21:18
Just checked my last prescription-CSA SCH IV. Knew it was something like that but never looked. Thanks for the clarity! 😊
ariel nicholas December 6, 2025 AT 02:33
Let’s be real-this isn’t about public health, it’s about control. The DEA doesn’t care if you’re in pain-they care if you’re compliant. Schedule I for cannabis? That’s not science-it’s politics. And don’t get me started on how they classify fentanyl analogs versus heroin-total chaos. The system isn’t broken-it was designed this way. To keep the masses docile. And you? You’re just a number in their database.
Scotia Corley December 7, 2025 AT 08:09
It is profoundly irresponsible to suggest that Schedule IV medications are equivalent in risk to Schedule III. The pharmacological profiles, dependency potential, and clinical outcomes are empirically distinct. The assertion that the system is ‘based on history’ rather than data is not only inaccurate-it is dangerously misleading. The DEA’s classification is grounded in decades of peer-reviewed toxicology, epidemiological surveillance, and controlled substance abuse metrics. To dismiss it as archaic is to misunderstand the very foundations of clinical pharmacology.
Kelly Essenpreis December 8, 2025 AT 01:30
Why do we even have schedules? Why not just ban everything dangerous and let the rest be OTC? All this paperwork just makes pharmacies hate their jobs and patients hate the system. My cousin got denied her anxiety med because the script had a typo in the DEA number. She cried. No one should have to cry over a prescription.
Margaret Stearns December 9, 2025 AT 00:56
My grandma took tramadol for years. She never knew it was schedule IV. She just took it when it hurt. I showed her the label last week and she was like ‘oh so thats why they make me come in every month’. She’s 78. She doesn’t need a class system. She needs to not be in pain.
amit kuamr December 9, 2025 AT 19:57
India has no such system. People buy tramadol, codeine, even oxycodone over the counter. No DEA number. No forms. No delays. And yet, addiction rates are lower than in the US. Maybe the problem isn’t the drug. Maybe it’s the fear. The control. The bureaucracy. We treat patients like criminals. That’s the real disease.
Debbie Naquin December 10, 2025 AT 05:28
The schedule isn’t a classification-it’s a narrative. It tells us which substances are ‘worthy’ of medical care and which are ‘dangerous’ by design. The criteria are opaque, politically mediated, and inconsistently applied. Codeine’s schedule shifts not because of pharmacology but because of corporate formulation. The label isn’t a legal map-it’s a mirror of institutional power. We don’t regulate drugs-we regulate people through drugs.