
Health December 4, 2025
Antihistamines and Dementia Risk: What You Need to Know About Long-Term Use
Anticholinergic Burden Calculator
Calculate the cumulative anticholinergic burden of your medications to understand potential dementia risk. The Anticholinergic Cognitive Burden (ACB) scale rates medications from 0 (no anticholinergic effect) to 3 (strong anticholinergic effect).
Total ACB score indicates risk level:
0 = Low risk
1-2 = Moderate risk
3+ = High risk
Total Anticholinergic Burden
Current score: 0
Many older adults reach for diphenhydramine-better known as Benadryl-to help them sleep or manage allergies. It’s cheap, easy to find, and works fast. But what happens when you take it every night for months or years? A growing body of research suggests there may be a hidden cost: an increased risk of dementia. This isn’t about occasional use. It’s about long-term, daily exposure to certain antihistamines that block a key brain chemical called acetylcholine. And the warning isn’t just from one study-it’s backed by guidelines from the American Geriatrics Society, the FDA, and European regulators.
Why Some Antihistamines Are Riskier Than Others
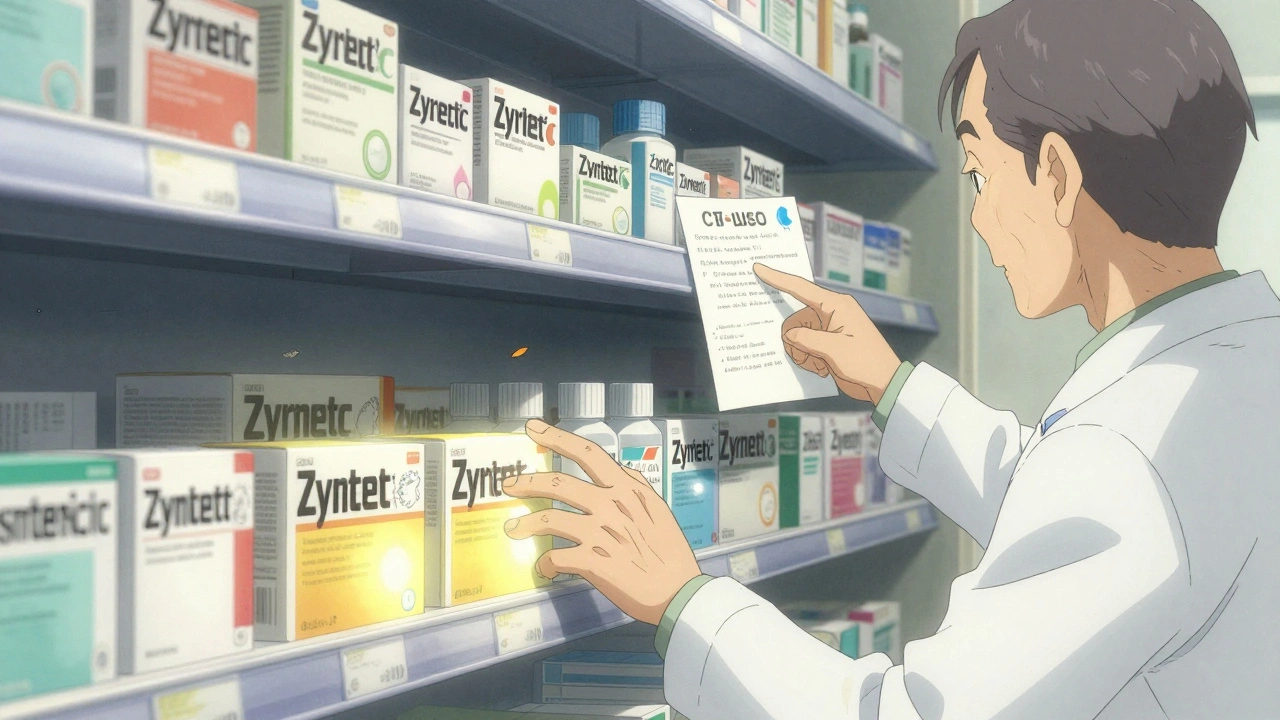
Not all antihistamines are the same. There are two main types: first-generation and second-generation. First-generation ones like diphenhydramine, doxylamine, and chlorpheniramine cross the blood-brain barrier easily. Once inside, they block acetylcholine receptors. That’s why they make you drowsy. But acetylcholine isn’t just about sleep-it’s essential for memory, focus, and learning. When you consistently block it over years, your brain may struggle to maintain normal function. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are designed differently. They don’t cross into the brain easily because of a natural defense system called P-glycoprotein. That means they relieve allergies without messing with your memory. Their anticholinergic effect is 100 to 1,000 times weaker than first-generation drugs. If you’re taking an antihistamine daily, switching to one of these is one of the simplest safety moves you can make.What the Research Actually Shows
The big 2015 JAMA Internal Medicine study that first raised alarms tracked over 3,400 people aged 65 and older for a decade. It found that people who took anticholinergic medications daily for three years or more had a higher risk of dementia. But here’s the twist: when researchers broke the data down by drug type, antihistamines didn’t show the same risk as antidepressants or bladder medications. A follow-up study in 2019 confirmed this-antihistamines had a hazard ratio of 1.00, meaning no increased risk. Other studies, like one published in Frontiers in Aging Neuroscience in 2022, found higher dementia rates among first-gen users, but the difference wasn’t statistically significant. So why the confusion? Because many earlier studies grouped all anticholinergics together. If you lump together a powerful bladder drug with a mild allergy pill, the overall risk looks bigger than it is. The real danger lies in drugs with high anticholinergic burden-like oxybutynin for overactive bladder or amitriptyline for depression. Antihistamines, even the first-gen ones, sit lower on that scale.The American Geriatrics Society Says: Avoid Them
Despite the mixed research, the 2023 American Geriatrics Society Beers Criteria gives a clear, strong recommendation: avoid first-generation antihistamines in adults 65 and older. They’re rated Level A-meaning there’s strong evidence and consensus behind the warning. The reason? Even if the dementia link isn’t proven beyond doubt, the potential harm is real enough to justify caution. These drugs can cause confusion, falls, urinary retention, and dry mouth. For older adults already at risk for cognitive decline, adding a daily anticholinergic is like stacking the odds. The European Medicines Agency is more cautious in its wording, calling the evidence "inconsistent" and calling for more long-term studies. But they still require updated patient leaflets to mention potential long-term cognitive effects. That’s a big deal. Regulatory agencies don’t add warnings lightly.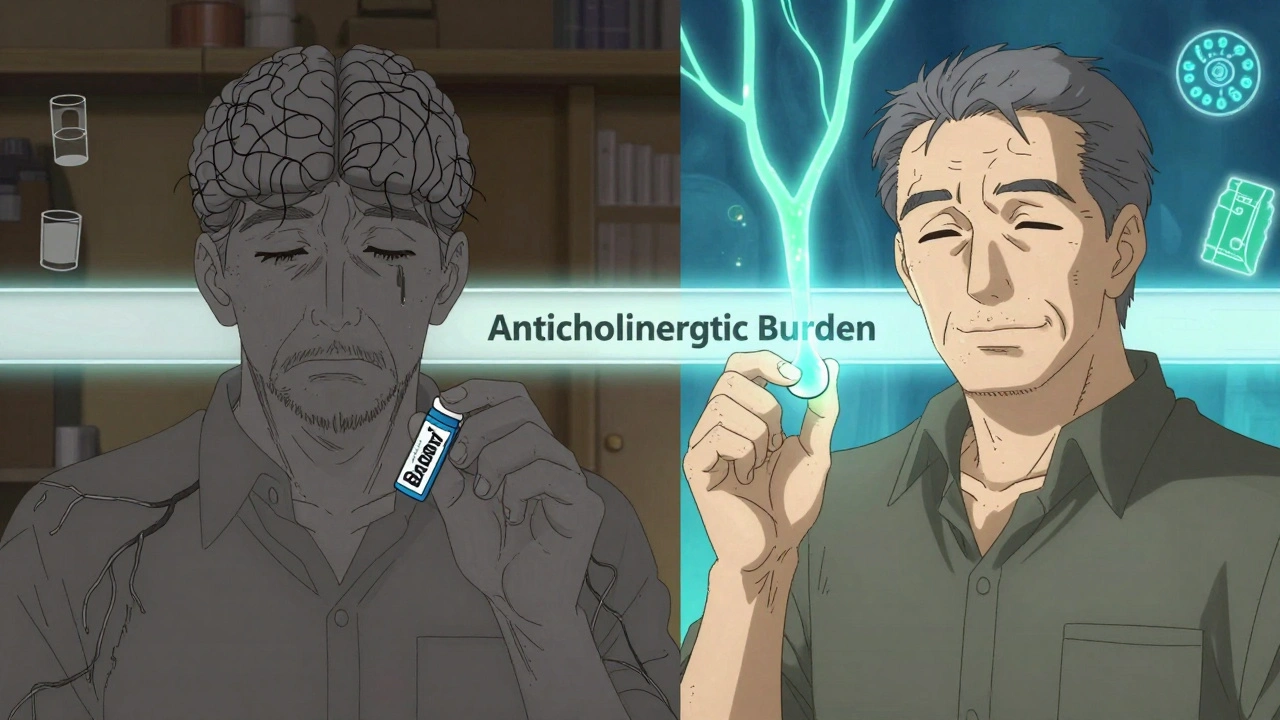
Why People Keep Taking Them
If the risks are known, why are so many still using diphenhydramine? The answer is simple: they don’t know better. A 2022 survey by the National Council on Aging found that 42% of adults over 65 use over-the-counter antihistamines for sleep. Of those, 78% had no idea these drugs have anticholinergic properties. Many were prescribed them years ago by doctors who didn’t realize the long-term risks. Others bought them on their own because they thought, "It’s just an OTC sleep aid." Reddit threads and forums are full of stories like this: "My mom took Benadryl every night for 10 years. Now she has Alzheimer’s. Was it the medicine?" There’s no definitive answer, but the pattern is worrying enough that experts urge people to question it.What to Do Instead
If you’re using diphenhydramine for sleep or allergies, here’s what to do next:- For allergies: Switch to loratadine, cetirizine, or fexofenadine. They work just as well without the brain effects.
- For sleep: Talk to your doctor about cognitive behavioral therapy for insomnia (CBT-I). It’s more effective long-term than any pill, with 70-80% success rates in older adults. The catch? It’s hard to find a therapist. Wait times average over two months, and Medicare only pays $85-$120 per session.
- For mild sleep issues: Try melatonin (3 mg max), magnesium glycinate, or a consistent bedtime routine. Avoid screens an hour before bed. Keep your room cool and dark.
- For chronic insomnia: Low-dose doxepin (Silenor) is an FDA-approved option with minimal anticholinergic activity (ACB score of 1). It’s not cheap, but it’s safer than Benadryl.
Also, review all your meds every six months. Many older adults take five or more medications. Some are for pain, some for anxiety, some for sleep. Together, they can add up to a high anticholinergic burden-even if no single drug seems dangerous. Use the Anticholinergic Cognitive Burden Scale (ACB) to check your meds. Diphenhydramine is a 3 (highest risk). Fexofenadine is a 0 (no risk).
What’s Changing Right Now
The landscape is shifting. First-gen antihistamine sales dropped 24% between 2015 and 2022. Second-gen sales rose by 18%. More pharmacies now place first-gen drugs behind the counter. The FDA is reviewing all anticholinergics for dementia risk, with results expected in early 2024. The American Geriatrics Society’s 2024 update to the Beers Criteria will likely tighten recommendations even further. The biggest change? Awareness. Ten years ago, most doctors didn’t think twice about prescribing Benadryl for sleep. Now, they’re trained to ask: "Is this necessary? Is there a safer alternative?" The Choosing Wisely campaign, started by the American Board of Internal Medicine, lists avoiding diphenhydramine for chronic insomnia as one of its top five recommendations for older adults.Bottom Line: Don’t Panic, But Do Act
There’s no smoking gun proving that Benadryl causes dementia. But there’s enough evidence to say this: long-term use of first-generation antihistamines is not worth the risk. Especially when safer, equally effective options exist. If you or a loved one is taking diphenhydramine daily, talk to a doctor. Don’t stop cold turkey-sudden withdrawal can cause rebound insomnia or worse. But do start planning a switch. Replace it with a second-gen antihistamine for allergies. For sleep, explore non-drug options first. Your brain will thank you.Write a comment
Items marked with * are required.



10 Comments
Rupa DasGupta December 5, 2025 AT 23:58
My grandma took Benadryl every night for 15 years... now she doesn’t recognize me. 😢 Coincidence? Maybe. But I’m not taking any chances.
Marvin Gordon December 7, 2025 AT 12:36
Switched from diphenhydramine to Zyrtec last year. Slept just as well, no brain fog, and my wife says I’m not yelling at the TV anymore. Easy win.
Also, CBT-I is legit. Took me 3 months to get in, but it changed my life. No pills needed.
Michael Dioso December 8, 2025 AT 08:28
Of course the FDA is "reviewing" it now. They waited until Big Pharma stopped pushing Benadryl as a sleep aid. Classic. They knew this for decades. You think they care about your brain? Nah. They care about lawsuits.
And don’t even get me started on "second-gen" - they’re just rebranded poison with a prettier label.
Krishan Patel December 8, 2025 AT 17:05
People still use this stuff? You’re literally poisoning your hippocampus for a few extra minutes of sleep. It’s not even a choice - it’s negligence. If your doctor prescribed this, they’re not a doctor. They’re a liability.
And yes, I’ve read the studies. The data is clear. Your brain doesn’t regenerate acetylcholine like it used to. Every pill is a brick in the wall between you and your memories.
sean whitfield December 10, 2025 AT 06:23
Wow. So the government finally noticed that sleeping pills make you forget your own name? Groundbreaking.
Next they’ll tell us breathing oxygen causes lung damage. Maybe we should all just stop existing.
ashlie perry December 11, 2025 AT 00:46
They’re hiding the truth. Benadryl was banned in Europe for years before they let it back in. The FDA is in bed with the drug companies. They don’t want you to know that your memory loss is from the medicine you bought at CVS. Look up the 2017 internal memo. It’s on archive.org. I’ve got screenshots.
Carole Nkosi December 11, 2025 AT 05:30
You think this is about health? No. It’s about control. They want you dependent on expensive alternatives. CBT-I? Try finding a therapist who takes Medicaid. Good luck. Meanwhile, Benadryl costs $3. That’s not a medical issue - it’s a class war.
Jimmy Jude December 13, 2025 AT 05:08
Let’s be real - if you’re taking Benadryl nightly, you’re not just risking dementia. You’re risking becoming a walking zombie who forgets where they put their dentures. I’ve seen it. I’ve smelled it. I’ve heard the snoring.
And now you want to talk about "evidence"? The evidence is in the nursing home. The evidence is in the empty stare. The evidence is in the fact that your mom used to recite Shakespeare and now she calls her cat "the president."
It’s not a theory. It’s a funeral waiting to happen.
Stephanie Bodde December 13, 2025 AT 10:55
Hey, if you’re reading this and you’re taking Benadryl - you’re not alone. I was too. But I switched to melatonin + a weighted blanket and I haven’t felt this clear-headed in 10 years. 💪 You got this. Talk to your doctor. Start small. One pill at a time. Your future self will high-five you.
And if you need someone to vent to? DM me. I’ve been there. I’m here for you. 🤗
Stephanie Fiero December 14, 2025 AT 08:34
My husband’s doctor told him Benadryl was fine for sleep - until he started forgetting his own birthday. Now he’s on doxepin and doing better than ever. But why did it take 3 years for someone to catch it? Because no one asks the right questions.
Everyone’s too busy Googling "why am I so tired" instead of checking the ACB scale. I printed one out and taped it to the medicine cabinet. It’s not rocket science. It’s just common sense.
Stop being lazy. Your brain matters more than $3.