
Health December 29, 2025
Fibromyalgia Pain: How Antidepressants Help Manage Widespread Chronic Pain
When you have fibromyalgia, pain isn’t just in one spot-it’s everywhere. It’s the kind of ache that wakes you up at 3 a.m., makes walking upstairs feel like climbing a mountain, and lingers no matter how much you rest. This isn’t muscle strain or arthritis. It’s fibromyalgia pain: a constant, dull, widespread ache that moves through your body, often without a clear cause. And for many people, the go-to medication isn’t a typical painkiller-it’s an antidepressant.
Why Antidepressants for a Pain Condition?
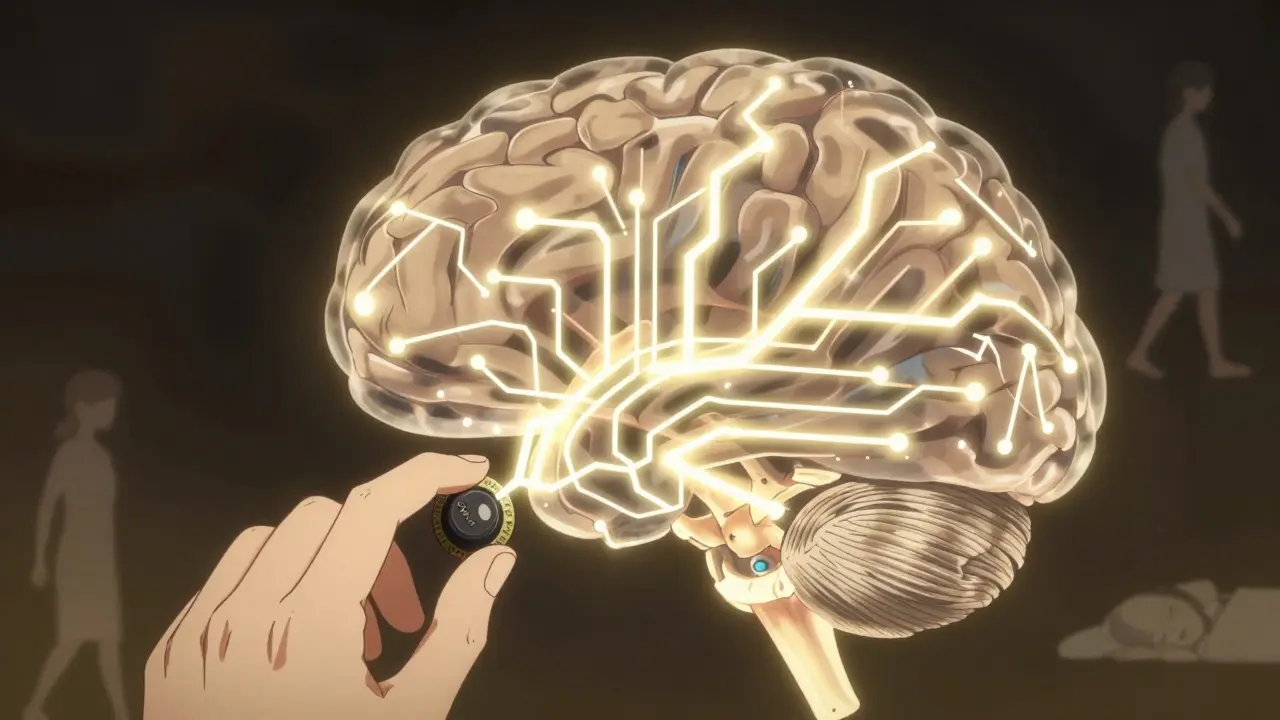
It sounds confusing at first. Why would you take a drug for depression to treat pain? The answer lies in how your brain processes pain. In fibromyalgia, the central nervous system gets stuck on high volume. Pain signals that should be quiet get amplified. It’s like your body’s alarm system is broken, and every little touch, sound, or movement sets it off. Antidepressants like amitriptyline, duloxetine, and milnacipran don’t work here because they make you happy. They work because they tweak the chemicals in your brain-serotonin and norepinephrine-that help control pain signals. At low doses, these drugs act like volume knobs, turning down the noise in your nerves. You don’t need to be depressed for them to help. In fact, many people with fibromyalgia aren’t clinically depressed at all.What Does Widespread Pain Actually Mean?
The American College of Rheumatology defines widespread pain in fibromyalgia as pain on both sides of your body and above and below your waist. That means if you feel pain in your left shoulder, you should also feel it in your right hip. If your neck hurts, your lower back should too. This isn’t random. It’s a pattern. For a diagnosis, this pain must last at least three months, with no other medical condition explaining it. Doctors used to press on 18 tender points to check for fibromyalgia. Now, they focus more on how long the pain has lasted and how many body areas are affected. The National Institutes of Health says pain needs to be present in at least four out of five regions: left upper, right upper, left lower, right lower, and axial (neck, chest, or spine). If you’ve had this kind of pain for months or years, and nothing shows up on X-rays or blood tests, fibromyalgia is likely the culprit.The Top Antidepressants Used Today
Three types of antidepressants are most commonly used for fibromyalgia: tricyclics (TCAs), SNRIs, and sometimes SSRIs. But not all are equal.- Amitriptyline (a TCA) is the oldest and cheapest. Most people start with just 5 mg at bedtime-less than a quarter of a standard antidepressant dose. It’s especially good for sleep. Studies show it reduces pain by 25-30% more than placebo, and nearly half of users report meaningful improvement.
- Duloxetine (Cymbalta) and milnacipran (Savella) are SNRIs. These are FDA-approved specifically for fibromyalgia. Duloxetine is usually taken at 60 mg daily. Milnacipran is dosed higher than for depression-100 to 200 mg a day. They help with pain and fatigue, but don’t improve sleep as much as amitriptyline.
- SSRIs like fluoxetine (Prozac) are less effective for pain alone. They’re sometimes added if someone has clear depression, but they’re not first-line for fibromyalgia pain.
What to Expect When You Start
Starting an antidepressant for fibromyalgia isn’t like popping a pill and feeling better the next day. It takes time. Most people don’t notice changes until 4 to 6 weeks. Full effects can take up to 12 weeks. That’s why many give up too soon. Side effects are common, especially at first. With amitriptyline, dry mouth (reported by 68% of users), drowsiness (57%), and weight gain are typical. Duloxetine often causes nausea (49%) and increased sweating (37%). Milnacipran can trigger headaches (53%) and constipation (31%). A 2023 review from Stanford Pain Medicine found that 78% of people experience side effects in the first few weeks. But many learn to manage them. Taking amitriptyline with a small snack helps with stomach upset. Drinking water constantly eases dry mouth. Most side effects fade after a few weeks if the dose is increased slowly.Who Benefits Most?
Antidepressants work best for people with two things: poor sleep and mood issues. About 30-50% of fibromyalgia patients also have anxiety or depression. For them, these drugs do double duty-calming the nervous system and lifting mood. They’re also most helpful if your pain is worse at night or if you wake up feeling exhausted. Amitriptyline, in particular, improves deep sleep, which is often disrupted in fibromyalgia. People who struggle with "fibro fog"-trouble concentrating or remembering things-don’t usually see big improvements from these drugs. That’s a sign the problem is more about brain processing than pain signaling. The European League Against Rheumatism gives amitriptyline a strong recommendation score of 8.7 out of 10 for pain relief. The Arthritis Foundation says it’s one of the most cost-effective options, costing just $4-$10 a month as a generic. Brand-name SNRIs like Savella can cost $300-$500 a month.Why So Many People Stop Taking Them
About 30% of people quit antidepressants within three months. Why? Side effects. But also because they expect quick results. One Reddit user, u/FibroWarrior87, said: "Amitriptyline at 10 mg finally let me sleep through the night after 8 years-but the dry mouth is brutal." Another, u/PainFreeFuture, said duloxetine cut their pain from 8/10 to 5/10 but made them feel "emotionally flat." In a review of 1,247 patient ratings on Drugs.com, 48% found amitriptyline moderately to highly effective-but 32% stopped because of side effects. For duloxetine, 52% saw benefit, but 28% quit due to nausea. Doctors now know it’s not about finding the "best" drug. It’s about finding the right one for you. If one doesn’t work or causes too many side effects, switching is normal. Many people try two or three before finding their fit.
Antidepressants Aren’t the Whole Story
No expert recommends antidepressants as the only treatment. The American Pain Society and CDC both say medication should be part of a bigger plan. The most effective intervention for fibromyalgia? Regular movement. Walking, swimming, yoga, or even stretching for 20-30 minutes a day reduces pain more than any pill. Stress management, good sleep habits, and cognitive behavioral therapy (CBT) also help retrain how your brain responds to pain. A 2023 report from the Fibromyalgia Research Alliance found that 85% of rheumatologists now combine antidepressants with non-drug therapies. That’s the new standard. Medication helps you get to the point where you can move, breathe, and live again. But it doesn’t fix the root problem-your nervous system’s sensitivity.What’s Next for Treatment?
There’s no cure for fibromyalgia, but research is moving forward. Doctors are starting to use genetic tests to see how your body breaks down drugs. Some people metabolize amitriptyline too slowly, which means even low doses cause side effects. Testing for CYP450 enzymes can help avoid trial-and-error. New drugs are in the works. A compound called capivasertib is in Phase III trials as of late 2023. Early studies on NMDA receptor blockers show promise, with 35-40% pain reduction in early trials. But for now, the tools we have are limited. Antidepressants aren’t perfect. They don’t work for everyone. But for many, they’re the difference between being stuck in bed and being able to pick up your kid, cook dinner, or take a walk without crying from pain.Key Takeaways
- Fibromyalgia pain is widespread, constant, and not caused by tissue damage-it’s a brain signaling issue.
- Antidepressants like amitriptyline and duloxetine reduce pain by calming overactive nerves, not by treating depression.
- Low doses are used for pain; higher doses are for depression. Starting low and going slow cuts side effects.
- It takes 4-12 weeks to feel the full effect. Don’t quit too soon.
- Side effects are common but often improve. Dry mouth, drowsiness, and nausea are the top reasons people stop.
- Antidepressants work best with movement, sleep hygiene, and stress reduction-not alone.
- Amitriptyline is the most cost-effective option. SNRIs are more expensive but better tolerated.
- 30-50% of patients get meaningful pain relief. Only 10-20% reach 50% reduction.
Do antidepressants cure fibromyalgia?
No. Antidepressants don’t cure fibromyalgia. They help manage symptoms-mainly pain, sleep, and fatigue-by adjusting how your brain processes signals. Fibromyalgia is a chronic condition with no known cure. Treatment focuses on improving daily function, not eliminating the disease.
Can I take antidepressants if I’m not depressed?
Yes. Many people with fibromyalgia take antidepressants for pain, not mood. The doses used for pain are much lower than those for depression. Amitriptyline at 10 mg, for example, helps with sleep and pain but won’t change your mood. These drugs work on nerve pathways, not just brain chemistry related to depression.
Why is amitriptyline preferred over other antidepressants?
Amitriptyline is often the first choice because it’s cheap, effective for sleep, and has strong evidence for pain relief. It’s especially helpful for people who wake up tired or have trouble staying asleep. Studies show it reduces pain more than placebo and improves sleep quality better than SNRIs. It’s also been used for decades, so doctors know how to manage its side effects.
How long should I try an antidepressant before deciding it doesn’t work?
Give it at least 6 to 8 weeks. Most people don’t feel benefits until after 4 weeks, and maximum effects often take 12 weeks. If you’ve reached the highest recommended dose and still have less than 20% pain reduction after 8 weeks, your doctor may suggest switching or adding another treatment. Don’t stop early just because you don’t feel better in the first week.
Are there alternatives to antidepressants for fibromyalgia pain?
Yes. Pregabalin (Lyrica) is an FDA-approved anticonvulsant that works similarly to antidepressants by calming overactive nerves. Other options include physical therapy, aerobic exercise, CBT, acupuncture, and mindfulness. Exercise is actually the most effective single treatment-studies show regular movement reduces pain more than any medication. Many people combine a low-dose antidepressant with walking or swimming for the best results.
If you’ve been struggling with widespread pain and feel like nothing helps, you’re not alone. Antidepressants aren’t magic, but for many, they’re the missing piece that lets them reclaim part of their life. The key is patience, persistence, and pairing them with movement, rest, and support. You’re not just treating pain-you’re retraining your nervous system.
Write a comment
Items marked with * are required.




9 Comments
Jasmine Yule December 30, 2025 AT 20:59
This post hit me right in the feels. I’ve been on amitriptyline for 3 years and honestly? It’s the only thing that lets me sleep past 4 a.m. Dry mouth? Yeah, I chew sugar-free gum like it’s my job. But waking up without crying from pain? Worth it. 🙌
Greg Quinn January 1, 2026 AT 10:40
It’s wild how a drug meant for depression ends up being a neural volume knob. The brain’s pain circuitry is just… miswired, not broken. Kinda makes you wonder how many other ‘chronic’ conditions are just nervous system glitches we’re medicating instead of rewiring.
Lisa Dore January 3, 2026 AT 02:39
To anyone reading this and thinking ‘I can’t handle side effects’ - you’re not weak. It’s a brutal balancing act. But I promise, the first time you cook a meal without crying, or hug your kid without wincing? That’s the win. Keep going. You’re not alone. 💪
Sharleen Luciano January 4, 2026 AT 17:41
Let’s be honest - amitriptyline is the 1980s of fibromyalgia treatment. It’s cheap, it’s crude, and it works. But calling it ‘first-line’ is like recommending a flip phone because it has a battery that lasts a week. SNRIs are objectively superior, and if your doctor still pushes TCAs without discussing alternatives, they’re not keeping up. Just sayin’.
Manan Pandya January 5, 2026 AT 09:33
Thank you for this detailed breakdown. I’ve been on duloxetine for 5 months. Nausea was brutal at first, but tapering from 30mg to 60mg over 6 weeks made all the difference. The key is slow titration. Also, hydration and avoiding caffeine helps with the sweating. This isn’t magic - it’s neuropharmacology.
Aliza Efraimov January 5, 2026 AT 14:35
My doctor told me to ‘just try it’ and I almost walked out. Then I found a rheumatologist who actually listened. I started at 10mg amitriptyline, added 15 minutes of walking daily, and did CBT for 3 months. Pain dropped from 9/10 to 4/10. It’s not one thing - it’s the whole damn ecosystem. Don’t let anyone sell you a silver bullet.
Nisha Marwaha January 7, 2026 AT 11:16
From a neurophysiological standpoint, the modulation of descending inhibitory pathways via serotonergic and noradrenergic reuptake inhibition is the mechanistic cornerstone of antidepressant efficacy in central sensitization syndromes like fibromyalgia. The clinical translation of this pharmacodynamic profile is why TCAs and SNRIs outperform NSAIDs and opioids in long-term management. Also, your sleep architecture improves due to REM suppression - critical for pain gate modulation.
Paige Shipe January 8, 2026 AT 04:43
I’ve read every study. Every trial. Every meta-analysis. And I’m telling you - antidepressants don’t work for fibromyalgia. They’re just a placebo with side effects. I’ve been on five of them. Nothing. My pain is real. My suffering is real. And doctors keep pushing pills like it’s 1998. I’m done.
Kevin Lopez January 9, 2026 AT 09:03
SNRIs > TCAs. End of story. Amitriptyline’s side effect profile is a dumpster fire. If your doc prescribes it without discussing Cymbalta or Savella first, they’re lazy. Also, exercise isn’t ‘alternative’ - it’s the only thing that changes neuroplasticity. Stop looking for pills. Start moving.