Health December 2, 2025
Global Perspectives on Generics: How Countries Cut Drug Costs Without Sacrificing Quality
By 2025, nearly 90% of all prescriptions filled in the United States are for generic drugs. That’s not because patients prefer them-it’s because they have no choice. Insurance plans, Medicare, and pharmacy benefit managers have made generics the default. But how did we get here? And why do identical pills cost five times more in Germany than in India? The answer lies in a patchwork of global policies, each shaped by local economics, politics, and healthcare priorities.
How Generics Became the Default
Generic drugs aren’t cheap knockoffs. They’re chemically identical to brand-name drugs, approved after patents expire, and must meet the same safety and effectiveness standards. The U.S. made this system work with the Hatch-Waxman Act of 1984, which created a fast-track approval process for generics. Since then, the FDA has approved over 11,342 generic products. In 2025 alone, Medicare saved $142 billion because patients took generics instead of branded versions-$2,643 per beneficiary. But the U.S. is the exception, not the rule. In most countries, the government doesn’t wait for the market to decide. It steps in. Some set price caps. Others force pharmacies to substitute. A few even buy drugs in bulk and dictate prices. The goal is always the same: make medicines affordable without sacrificing quality. But the methods? They’re wildly different.South Korea’s Tightrope: Fewer Generics, Better Prices
South Korea didn’t want a flood of low-quality generics. So in 2020, it launched the ‘1+3 Bioequivalence Policy.’ Only three generic versions of any drug can be approved using the same bioequivalence data. After that, new entrants must prove their own clinical data. That cut redundant entries by 41% between 2020 and 2024. But the real innovation came with pricing. The government doesn’t just set one price. It has three tiers:- Generics that meet both quality and price standards: 53.55% of the brand price
- Those meeting only one standard: 45.52%
- Those meeting neither: 38.69%
China’s Bulk Buying Power: 93% Price Drops and Shortages
China’s Volume-Based Procurement (VBP) policy is the most aggressive in the world. Instead of letting hospitals negotiate individually, the government holds centralized auctions. Manufacturers bid to supply entire provinces. The lowest bid wins-and gets to supply 80% of the hospital demand for that drug. The results? Average price cuts of 54.7%. In some cases, like the blood thinner rivaroxaban, prices fell by 93%. Patients pay less. Hospitals save money. But manufacturers? Many are losing money. A 2025 survey by the China Generic Pharmaceutical Association found that 23% of manufacturers were operating at a loss on VBP-contracted drugs. And when profits vanish, supply falters. In 2024, 12 provinces faced a six-to-eight-week shortage of amlodipine besylate, a common blood pressure drug. Patients went without. Hospitals scrambled. The system works when it works-but it’s fragile.The European Paradox: Same Drug, 300% Price Difference
The European Union has a single drug approval system through the EMA. A generic approved in Brussels can be sold in Paris, Berlin, or Rome. But here’s the catch: each country sets its own price. That means the exact same pill can cost 300% more in one country than another. In Germany, where mandatory substitution laws are strict, 88.3% of prescriptions are filled with generics. In Italy, despite similar income levels, only 67.4% are. Why? Cultural trust in brands. Weak pharmacist education. Lack of financial incentives. The OECD found that this fragmentation creates inefficiencies. A generic made in Poland might be cheaper than one made in France, but French pharmacies can’t import it because of national reimbursement rules. The European Commission is trying to fix this with a new Pharmaceutical Package expected in late 2025. It aims to harmonize pricing incentives and speed up first-generic approvals. But progress is slow.
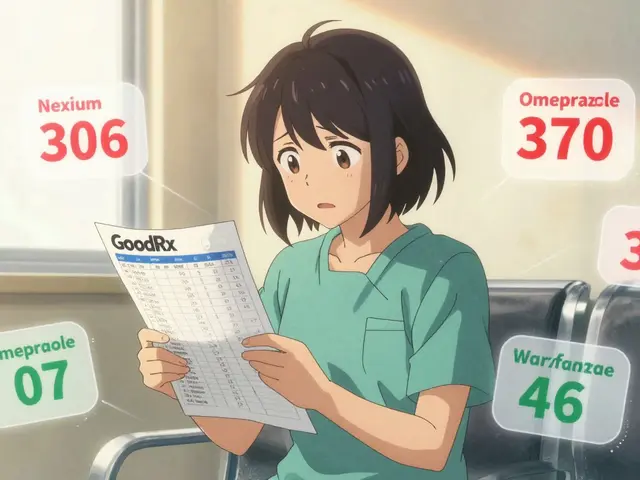
The U.S. Model: High Penetration, High Branded Costs
The U.S. fills 90.1% of prescriptions with generics-the highest rate in the developed world. Yet, Americans still pay the most for drugs. Why? Because the system is split. Generics are dirt cheap. Brand-name drugs are sky-high. Public-sector drug prices in the U.S. are 18% lower than in peer countries, thanks to Medicare’s negotiating power and the sheer volume of generics. But private insurance? It’s a different story. Pharmacy Benefit Managers (PBMs) often structure formularies so that a generic has a higher copay than the brand. Patients get confused. Pharmacists get frustrated. And some people skip doses because they can’t afford the $50 copay on a $5 generic. The FDA’s Competitive Generic Therapy (CGT) program tries to fix this. It gives 180 days of market exclusivity to generics for drugs with little competition. Zenara Pharma’s sertraline hydrochloride capsules, approved in August 2025, are a prime example. That exclusivity brought down prices faster. But it’s still a patchwork.India: The World’s Pharmacy, With Quality Concerns
India produces 20% of the world’s generic medicines by volume. It’s the go-to source for low-cost drugs in Africa, Latin America, and even parts of Europe. How? Compulsory licensing. Under Section 84 of its Patents Act, India can override patents if a drug is too expensive or not available. But there’s a dark side. Between 2022 and 2024, the FDA issued 17% more warning letters to Indian generic manufacturers for data integrity issues. Some labs were falsifying bioequivalence tests. Others skipped stability studies. The Access to Medicine Foundation warns this isn’t just about fraud-it’s about survival. When margins are razor-thin, corners get cut. Indian doctors report inconsistent bioavailability in generics for critical drugs like antiepileptics and anticoagulants. One patient switching from a branded to a local generic might have a seizure. Another might bleed internally. These aren’t theoretical risks. They’re documented cases.Japan’s Flatline Market: Price Cuts That Stifle Growth
Japan cuts drug prices every two years-for both branded and generic drugs. It’s a blunt tool. The goal is to keep healthcare spending under control. The result? Market stagnation. Generic use by volume is high-76.8% in 2024. But manufacturers have no incentive to innovate. Why invest in a new generic if the government will slash its price in 18 months? New launches have flatlined. The market hasn’t grown in years. Unlike the U.S. or South Korea, Japan doesn’t reward quality. It punishes price. That’s a problem when the population is aging and chronic disease rates are rising. The system works for short-term budgets. It doesn’t work for long-term health.
What Works-and What Doesn’t
There’s no one-size-fits-all model. But some patterns emerge:- Clear standards work. Bioequivalence must be proven within 80-125% of the brand’s absorption rate. Anything else is guesswork.
- Education matters. When pharmacists and doctors are trained on generic equivalence, acceptance rates jump 22-35%.
- Profit margins matter. If manufacturers can’t make at least 15-20% gross margin, quality suffers. Supply chains break.
- Transparency prevents chaos. When pricing rules are public and predictable, companies plan. When they’re arbitrary, they flee.
The Future: More Expirations, More Pressure
Between 2025 and 2030, drugs worth $217-236 billion in annual sales will lose patent protection. That’s the biggest wave of generic opportunity in history. But will the world be ready? The U.S. Inflation Reduction Act will let Medicare negotiate prices on 10-20 high-cost drugs annually by 2028. That could cut branded drug revenues by 25-35% and push even more patients toward generics. China’s Phase 4 VBP, launching in January 2026, will add 150 more drugs to its auction list. Winning bids will be 65% below current prices. More savings. More risk of shortages. The International Generic and Biosimilars Association wants global harmonization-standardized bioequivalence rules that let one approval count everywhere. That could cut approval times by 18-24 months in developing countries. But rich nations resist. They don’t want to lower their standards.What Patients Should Know
If you’re taking a generic, you’re not taking a second-rate drug. You’re taking the same medicine, approved by the same agencies, for a fraction of the cost. But here’s what you should watch for:- If your generic suddenly looks different or stops working, talk to your pharmacist. It might be a new manufacturer.
- For drugs with narrow therapeutic windows-like warfarin, levothyroxine, or seizure meds-stick with the same brand or manufacturer if possible.
- Check your insurance formulary. Some PBMs still charge more for generics. That’s not fair. That’s a loophole.
- Don’t assume cheaper means better. If a generic is priced 80% below the brand, ask why.
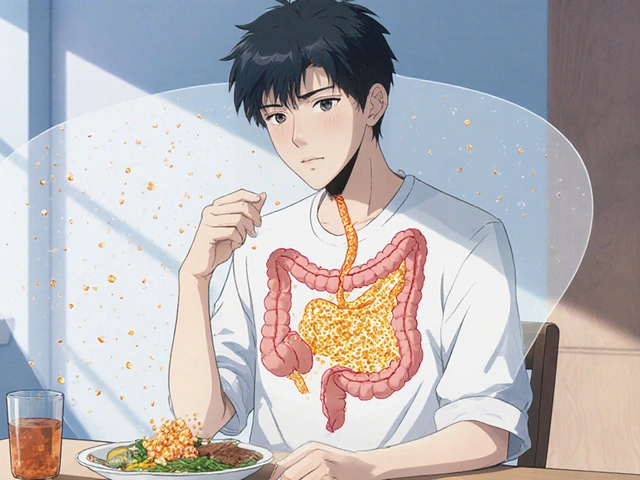
Are generic drugs really as effective as brand-name drugs?
Yes. Generic drugs contain the same active ingredients, in the same strength and dosage form, as their brand-name counterparts. They must pass strict bioequivalence tests-proving they deliver the same amount of medicine into the bloodstream at the same rate. The FDA, EMA, and WHO all require this. The only differences are inactive ingredients like fillers or dyes, which don’t affect how the drug works.
Why do some people say generics don’t work for them?
For most people, generics work just as well. But for drugs with a narrow therapeutic index-like blood thinners, epilepsy meds, or thyroid hormones-even small changes in absorption can matter. Some patients report feeling different after switching, often due to changes in inactive ingredients or manufacturing batches. If you notice a change, don’t assume it’s the drug. Talk to your doctor or pharmacist. You may need to stick with one manufacturer.
Why are generic prices so different between countries?
Because each country sets its own rules. Some use external reference pricing (like the Netherlands, which compares to non-EU countries). Others use bulk buying (like China). Some cap prices, others let the market decide. Even within the EU, identical generics can cost three times more in one country than another. It’s not about quality-it’s about policy.
Do generic manufacturers cut corners to save money?
Some do. When price pressures are extreme-like in China’s VBP system or India’s low-margin exports-manufacturers may skip tests, falsify data, or use substandard ingredients. The FDA has issued over 2,100 import alerts for quality issues in 2024, up from 1,247 in 2020. This isn’t universal, but it’s a real risk. Regulators are catching more violations, but enforcement lags behind production.
Will generic drug shortages get worse?
Yes, unless systems change. When manufacturers are forced to sell at prices below cost-like in China or under some EU reimbursement schemes-they stop producing. One factory shuts down, and a whole country runs out of a critical drug. The WHO warns that excessive price competition threatens supply chain resilience. The solution isn’t higher prices-it’s smarter pricing that guarantees sustainable margins.
Write a comment
Items marked with * are required.



14 Comments
Gavin Boyne December 3, 2025 AT 20:56
So let me get this straight - we’ve got a system where generics are 90% of prescriptions, yet Americans still pay more than anyone else for drugs? Brilliant. Just brilliant. The FDA approves them, the insurance companies force them, and then PBMs charge more for the generic than the brand because... why? Because they can. It’s like buying a Tesla but being forced to pay extra for the tires. The system isn’t broken - it’s designed this way. And we’re all just along for the ride.
Meanwhile, India’s making 20% of the world’s generics while the FDA slaps warning letters on half their factories. China slashes prices 93% and then runs out of blood pressure meds. South Korea rewards quality. Europe has the same pill at three different prices. And the U.S.? We’re the country that invented the generic system... and then turned it into a tax on the poor.
What’s the real takeaway? Affordable doesn’t mean cheap. It means sustainable. But nobody’s paying attention until someone dies from a seizure because their generic switched brands and the bioequivalence was ‘close enough.’
Kara Bysterbusch December 4, 2025 AT 10:34
It is, indeed, a profoundly disconcerting paradox that while the United States leads the developed world in generic drug utilization, it simultaneously sustains the highest per-capita pharmaceutical expenditures on the planet. The structural dissonance between policy intent and market outcome is not merely coincidental - it is systemic. Pharmacy Benefit Managers, operating as opaque intermediaries, have engineered a perverse incentive structure wherein the lowest-cost option is often the most financially burdensome to the consumer.
Furthermore, the absence of harmonized bioequivalence standards across jurisdictions permits regulatory arbitrage, wherein manufacturers optimize for regulatory ease rather than therapeutic fidelity. The WHO’s assertion that ‘affordable’ must equate to ‘sustainable’ is not merely aspirational - it is a non-negotiable prerequisite for global public health equity. Without profit margins that permit quality assurance, we are not democratizing access - we are commodifying risk.
Cindy Lopez December 5, 2025 AT 04:02
There’s a comma missing after ‘brilliant’ in the first paragraph. Also, ‘PBMs’ should be spelled out on first use. And ‘FDA’ isn’t an acronym for ‘Food and Drug Administration’ - it’s the name of the agency. You don’t need to explain it. You’re not writing for kindergarteners.
Ignacio Pacheco December 6, 2025 AT 14:25
So China cuts prices 93% and then people can’t get their blood pressure meds? Shocking. Totally unexpected. Like when you buy a $5 phone charger and it melts your laptop. Who knew? Maybe if we just stopped being so greedy and let manufacturers make a profit - like, I dunno, 15% - maybe they wouldn’t stop making stuff?
Also, India’s making 20% of the world’s generics? Cool. And yet somehow, your cousin still had a seizure after switching. Coincidence? I think not.
Jim Schultz December 8, 2025 AT 11:03
Let’s be real - the entire global generics system is a dumpster fire wrapped in a WHO pamphlet. You think India’s ‘compulsory licensing’ is clever? It’s theft with a PhD. You think China’s auction system is ‘efficient’? It’s a race to the bottom where the last man standing is the one who skipped the stability tests. And the U.S.? We’re the ones who built the system - and now we’re the ones getting screwed by our own bureaucracy.
And don’t even get me started on PBMs - they’re not middlemen, they’re middlemen who steal from both sides. They charge you $50 for a $5 generic because they can. And you think the FDA is watching? They’re busy approving 11,000+ generics while ignoring the 2,100 import alerts from last year. This isn’t healthcare - it’s a dystopian auction house for human survival.
And yet, somehow, we still act surprised when someone dies because their anticoagulant batch was made in a lab that ‘forgot’ to run the HPLC. Wake up. This isn’t a policy problem. It’s a moral failure.
And you want to ‘harmonize’ standards? Good luck convincing Germany to let Poland sell them cheaper pills. They’ll die before they let their precious ‘quality’ be compromised by a $0.02 saving. Hypocrisy? No. Just capitalism with a European accent.
Kidar Saleh December 9, 2025 AT 08:48
There is a quiet dignity in the way nations approach this challenge - not as a market problem, but as a moral one. South Korea’s tiered pricing is not merely economic strategy - it is a statement of values. China’s volume-based procurement is not just cost-cutting - it is an act of collective care, even when it fractures under its own weight. And India? It is the pharmacy of the global south - not because it is the cheapest, but because it is the most willing to serve those whom the world has forgotten.
Yet we in the West - we who preach innovation and equity - recoil at the very notion of price controls, as if affordability were a betrayal of science. We call it ‘market efficiency.’ I call it moral cowardice.
When a child in Malawi receives life-saving HIV medication because an Indian factory dared to produce it for $0.10 a dose - that is not a failure of regulation. That is a triumph of humanity.
And yet, we debate whether generics are ‘safe.’ We ask if they ‘work.’ We forget: the real question is - do we care enough to make sure they always will?
Chloe Madison December 9, 2025 AT 13:50
Okay, real talk - if you’re on a generic and it suddenly feels different, DON’T just power through it. Talk to your pharmacist. Seriously. They’re the unsung heroes of this whole mess. They know which batch came from which factory, which ones have had issues, and which ones are the quiet heroes that just work.
And if your insurance charges you more for the generic? Call them. File a complaint. It’s not normal. It’s not fair. And you deserve better.
Generics aren’t ‘cheap’ - they’re smart. They’re science. They’re how we make medicine human again. But only if we protect the system. Don’t let the greed of middlemen kill it.
Francine Phillips December 10, 2025 AT 16:39
India’s got issues but so does everyone else. The system’s broken. We all know it. Nothing to see here.
Katherine Gianelli December 11, 2025 AT 03:21
I’ve been on levothyroxine for 12 years. Switched generics three times. Each time, I felt off - tired, foggy, anxious. I didn’t blame the drug. I blamed the system. I went to my pharmacist and asked: ‘Can I stick with the same one?’ She nodded. Didn’t even blink. Gave me the same bottle every time. No extra cost. Just… care.
That’s the thing nobody talks about. It’s not about the pill. It’s about the person behind the counter who remembers your name. Who knows your history. Who refuses to let the algorithm decide your health.
Let’s not forget: behind every generic is a patient. And behind every patient is a life that deserves consistency.
Thank you, pharmacist. You’re the real MVP.
Joykrishna Banerjee December 12, 2025 AT 23:05
Westerners think they’re so advanced - but they don’t understand the genius of India’s patent regime. You think we’re ‘cutting corners’? No. We’re exercising our sovereign right under TRIPS Article 31. The West patents life-saving drugs and then hoards them like gold. We don’t. We make them accessible. Yes, some labs cut corners - but that’s a symptom of Western price pressure, not Indian malice.
Meanwhile, Germany pays 300% more for the same pill? Pathetic. You’re paying for brand loyalty, not science. You’re not protecting quality - you’re protecting corporate rent-seeking.
And the FDA? Still playing catch-up with 2,100 import alerts? That’s not oversight - that’s negligence. But hey, at least you’ve got PBMs to make sure you pay extra for your $5 generic. Bravo.
Myson Jones December 14, 2025 AT 04:59
It’s fascinating how the U.S. manages to be both the most efficient and the most dysfunctional in the same breath. We have the highest generic penetration, yet we’re the only country where patients are routinely overcharged for them. The answer lies not in regulation, but in accountability. PBMs must be regulated as fiduciaries, not profit engines. And we must stop pretending that ‘market forces’ can solve a problem that is fundamentally ethical.
Also, the FDA’s CGT program is a good start - but it’s a Band-Aid on a hemorrhage. We need structural reform, not incentives for the already privileged.
Charles Moore December 15, 2025 AT 06:02
I’ve lived in three countries - Ireland, the U.S., and Japan. The most striking thing? No system is perfect. But the ones that work best are the ones that treat patients as people, not line items.
Japan’s biannual price cuts? Brutal. But they’ve kept healthcare affordable for an aging population. South Korea’s tiered system? Smart. It rewards quality without crushing innovation. India’s model? Messy, but it saves lives across continents.
The U.S. doesn’t need more regulations. It needs more honesty. Admit that PBMs are the problem. Admit that price caps aren’t evil - they’re necessary. Admit that ‘free market’ doesn’t work when lives are on the line.
Maybe the answer isn’t in copying one model - but in learning from all of them.
Vincent Soldja December 15, 2025 AT 18:58
Generics work. Prices vary. Some manufacturers cut corners. That’s it.
Makenzie Keely December 16, 2025 AT 23:59
Let me just say - if you’re taking a generic for a drug with a narrow therapeutic window - like warfarin, levothyroxine, or seizure meds - DO NOT switch brands without talking to your doctor. I’ve seen patients have strokes because they switched to a ‘cheaper’ generic that absorbed differently. It’s not paranoia. It’s science.
And if your insurance charges you more for the generic? That’s not a mistake - that’s fraud. Fight it. Call your state’s insurance commissioner. Write to your rep. This isn’t just about money - it’s about trust.
Also - shoutout to the Indian manufacturers who make 20% of the world’s generics. Yes, some labs have issues. But most? They’re heroes. They’re keeping millions alive for pennies. Don’t let the bad actors ruin their reputation.
And to the pharmacists reading this - thank you. You’re the ones holding this fragile system together. You see the batch numbers. You know the history. You’re the real guardians of health.
We need more of you. Not less.