Health September 24, 2025
How Diabetes Increases the Risk of Pulmonary Tuberculosis - What You Need to Know
Diabetes mellitus is a chronic metabolic disorder characterised by elevated blood glucose levels due to insufficient insulin production or impaired insulin action. When blood sugar stays high, the body’s defence mechanisms start to wobble, creating a perfect storm for infections. diabetes and tuberculosis link is a phrase you’ll see more often in medical journals, and it isn’t just a coincidence.
What Is Pulmonary Tuberculosis?
Pulmonary tuberculosis is a contagious lung disease caused by the bacterium Mycobacterium tuberculosis. It spreads through airborne droplets when an infected person coughs or sneezes. While anyone can catch TB, people with weakened immunity-like those living with diabetes-are far more likely to develop active disease after exposure.
The Micro‑bug Behind the Illness
Mycobacterium tuberculosis is a slow‑growing, acid‑fast bacterium that can survive inside immune cells for years. Its knack for hiding inside macrophages makes it especially dangerous when the host’s immune surveillance is compromised.
Why Diabetes Changes the Immune Landscape
Two core metabolic problems drive the increased TB risk: insulin resistance is a condition where cells fail to respond properly to insulin, forcing the pancreas to produce more of the hormone and the resulting hyperglycemia is a state of persistently high blood glucose. Both conditions impair neutrophil chemotaxis, reduce cytokine production and blunt the oxidative burst that normally kills invading microbes.
Immune Dysfunction in Plain English
Immune dysfunction is a broad term covering any reduction in the body’s ability to mount an effective defence against pathogens. In diabetes, the dysfunction is two‑fold: the cellular immune response (T‑cells, macrophages) weakens, and the humoral response (antibodies) becomes less coordinated. The net effect is a slower, less decisive attack on Mycobacterium tuberculosis.
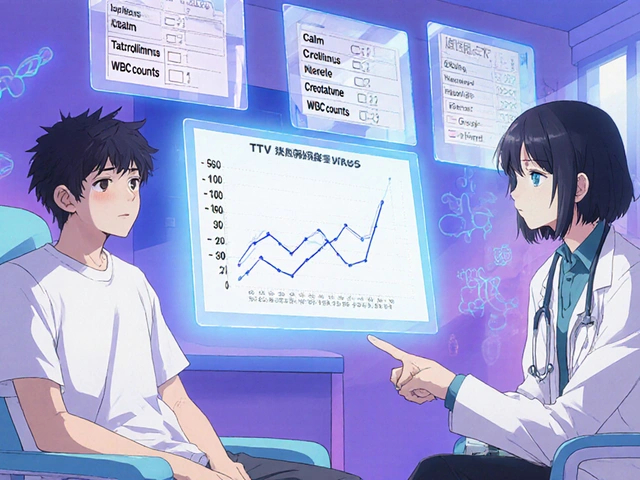
Numbers That Matter
According to the World Health Organization, there were roughly 10 million new TB cases worldwide in 2023, and people with diabetes accounted for about 15% of those infections. That translates to an estimated 1.5million cases where diabetes was a key co‑morbidity.
When HIV Joins the Party
The risk picture gets even grimmer when HIV co‑infection is present. HIV already devastates CD4‑positive T‑cells, and adding diabetes on top creates a triple hit: metabolic, immunological and viral. Studies from South Africa show a three‑fold increase in active TB among patients juggling both HIV and diabetes.
Prevention Tools Worth Mentioning
The BCG vaccine is a live‑attenuated vaccine derived from Mycobacterium bovis, administered early in life to protect against severe TB forms. While BCG’s efficacy wanes in adults, a recent trial in India suggested modest protection in diabetic adults when combined with good glycaemic control.

Clinical Red Flags in Diabetic Patients
Doctors say diabetic patients with TB often present with atypical symptoms: less pronounced fever, milder night sweats and a slower weight loss trajectory. Imaging may reveal cavitary lesions that look “quiet” on X‑ray because the immune response is muted. Awareness of these subtle cues can shave weeks off the diagnostic delay.
Diagnosis: Putting the Pieces Together
Standard TB work‑up still applies-sputum smear microscopy, GeneXpert PCR, and culture. However, labs now recommend an extra blood glucose check at the time of TB testing. If a patient’s HbA1c is above 6.5%, clinicians should suspect underlying diabetes and start appropriate management alongside anti‑TB therapy.
Managing Both Diseases Simultaneously
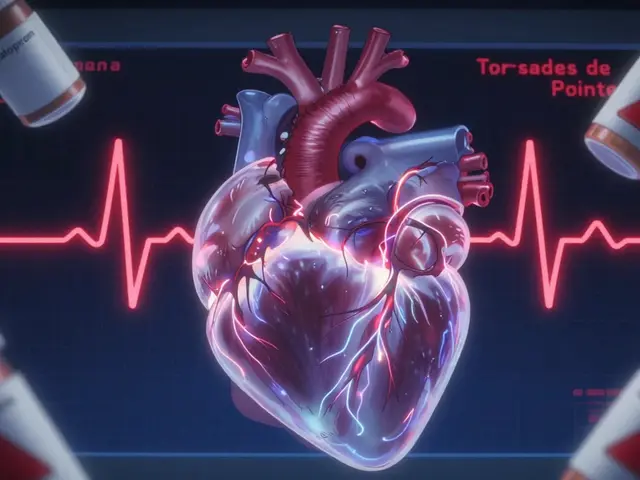
The cornerstone of TB treatment remains the six‑month regimen of isoniazid, rifampicin, pyrazinamide and ethambutol. Diabetes adds a layer of complexity: rifampicin speeds up the metabolism of many oral hypoglycaemic agents, including metformin which is a first‑line biguanide that lowers hepatic glucose production. Patients often need dose adjustments or a temporary switch to insulin during the intensive phase of TB therapy.
Comparison of Diabetes and Pulmonary Tuberculosis
| Attribute | Diabetes mellitus | Pulmonary tuberculosis |
|---|---|---|
| Primary Cause | Metabolic dysregulation (insulin deficiency or resistance) | Infection by Mycobacterium tuberculosis |
| Transmission | Non‑communicable (lifestyle, genetics) | Airborne droplets; highly contagious |
| Typical Treatment Duration | Lifelong management | 6‑9 months of multidrug therapy |
| Impact on Immune System | Impaired neutrophil and T‑cell function | Exploits weakened immunity to proliferate |
| Key Risk Factor for the Other | Elevated HbA1c ↑ TB activation risk | Active TB can worsen glycaemic control |
Public Health Angle
Health ministries in high‑burden countries are now screening all TB patients for diabetes and vice‑versa. The strategy aims to catch hyperglycaemia early, offering lifestyle advice and medication before TB progresses. Integrated care reduces mortality: a cohort from Brazil showed a 20% drop in TB‑related deaths when diabetic patients received coordinated treatment.
Related Concepts Worth Exploring
If you found this link fascinating, you might also want to read about social determinants of health which shape both diabetes prevalence and TB exposure, the role of nutritional status in immune resilience, and the emerging field of host‑directed therapies that aim to boost the body’s own defence mechanisms while fighting TB.
Frequently Asked Questions
Does having diabetes guarantee I’ll get tuberculosis?
No. Diabetes raises the risk-studies suggest a two‑ to three‑fold increase-but most diabetic people never develop TB. Good blood‑sugar control and safe living conditions keep the odds low.
Can TB make my diabetes worse?
Absolutely. The infection triggers stress hormones that raise glucose levels, and some anti‑TB drugs speed up the breakdown of oral diabetes meds. You’ll likely need tighter monitoring and possibly insulin for a few months.
Should I be screened for TB if I have diabetes?
Screening is recommended if you live in a high‑TB‑incidence area, have a history of close contact with TB patients, or notice persistent cough and weight loss. A simple chest X‑ray and sputum test can rule it out early.
Does the BCG vaccine protect diabetic adults?
Evidence is mixed. BCG may lower the risk of severe TB forms, but its overall protective effect in adults-especially those with compromised immunity-remains modest. It should be combined with good glycaemic control for best results.
How does rifampicin affect my diabetes medication?
Rifampicin induces liver enzymes that speed up the breakdown of drugs like metformin, sulfonylureas and thiazolidinediones. Your doctor may raise the dose or switch you to insulin while you finish the TB regimen.
Write a comment
Items marked with * are required.



10 Comments
Nicole Carpentier September 26, 2025 AT 00:26
This is actually the most clear breakdown of diabetes and TB I’ve ever read. I work in public health and even I learned something new. Good job on explaining the immune mechanics without drowning in jargon.
Also, the part about atypical symptoms in diabetics? So important. So many cases get missed because doctors expect the textbook fever and night sweats.
Eric Pelletier September 26, 2025 AT 18:38
The rifampicin-metformin interaction is way more dangerous than most clinicians realize. I’ve seen patients crash into DKA because their endo didn’t adjust doses. The enzyme induction is massive-rifampicin can cut metformin half-life by 40%. Insulin is safer during active TB. Always. No exceptions.
Hadrian D'Souza September 26, 2025 AT 23:59
Oh wow. Another ‘diabetes makes you weak’ article. Let me guess-next you’ll tell us obese people are just lazy and diabetics don’t wash their hands? This is medical colonialism dressed up as science. The real issue? Poverty, food deserts, and underfunded clinics. But sure, blame the patient’s pancreas.
Abhay Chitnis September 27, 2025 AT 21:56
LOL at the WHO stats. 15%? Bro, in India it’s more like 30-40% of TB cases have diabetes. We’ve known this since 2015. Why is this even news in the US? Also, BCG doesn’t work for adults. Period. Stop selling hope with outdated vaccines. 😒
Nonie Rebollido September 28, 2025 AT 23:45
I have type 2 and got TB last year. Took 8 months to get diagnosed because my cough was ‘just a cold’. They didn’t check my sugar. I’m alive because my cousin is a nurse. This needs to be standard. Like, everywhere.
Howard Lee September 29, 2025 AT 06:49
The table comparing diabetes and TB is excellent. Clear, concise, and accurate. The fact that TB can worsen glycemic control is often overlooked. It’s a two-way street, not just diabetes increasing TB risk. This should be shared with every primary care clinic.
Robert Spiece September 30, 2025 AT 03:16
So let me get this straight-we’re treating a bacterial infection with antibiotics while simultaneously letting a metabolic disorder run wild because ‘it’s chronic’? We’re basically giving someone a grenade and telling them to hold it while we hand them a bandaid. The system isn’t broken. It’s designed this way.
Vivian Quinones October 1, 2025 AT 10:57
Why are we even talking about this? TB is a third world problem. We should be fixing our own healthcare, not worrying about some bacteria that only hits poor people. Diabetes is the real crisis here-obesity, soda, junk food. Blame the culture, not the bug.
Marshall Pope October 2, 2025 AT 12:10
i had no idea rifampicin messed with metformin. my doc just said ‘take your pills’ and i believed her. now i’m scared. thanks for the heads up. i’ll call tomorrow.
Brandon Benzi October 2, 2025 AT 15:01
This article is pure woke medicine. Diabetes isn’t a weakness-it’s a choice. If you can’t control your sugar, why should we waste resources on you? TB is airborne, not diabetic. Fix your life before asking for a cure.