Health January 10, 2026
How to Coordinate Medication Plans after Hospital Discharge
When you leave the hospital, your body is still healing - but the safety net you had in place starts to thin out. One of the biggest risks during this transition isn’t the illness you were treated for - it’s your medication plan. Studies show that 30 to 70% of patients leave the hospital with a medication list that doesn’t match what they were taking at home. That mismatch can lead to dangerous side effects, missed doses, or even another hospital stay. In fact, medication errors after discharge cause nearly one in five readmissions within 30 days. This isn’t just a patient problem - it’s a system problem. And fixing it starts with clear, coordinated action.
Why Medication Reconciliation Matters More Than You Think
Medication reconciliation isn’t just a paperwork chore. It’s a formal, evidence-based process required by Medicare and Medicaid to prevent harm. The National Quality Forum calls it NQF 0097, and it’s built into the rules hospitals and clinics must follow to get paid. The goal? Make sure every pill, patch, or injection you’re supposed to take after discharge matches what you were taking before you went in - and what the doctors actually ordered. Here’s the reality: during your hospital stay, your meds were likely changed. Maybe your blood thinner was paused. Maybe your diabetes drug was switched. Maybe you got new antibiotics. When you’re discharged, those changes should be clearly documented and communicated. But too often, they’re not. A 2022 study found that 68% of hospitals still struggle with fragmented electronic records between inpatient and outpatient systems. That means your GP might not even see the updated list - and you’re left guessing what to take. The stakes are high. The American Society of Health-System Pharmacists says medication reconciliation is one of the top three ways to prevent readmissions. And the data backs it up: when pharmacists lead the reconciliation process, medication errors drop by over 30%, and readmissions fall by nearly 28%.The Three Steps to Get Your Medication Plan Right
You don’t need to be a doctor to make sure your meds are safe after discharge. Here’s what you need to do - in order.- Get a complete, written list before you leave. Ask for a printed or digital copy of your discharge medication list. It must include every medication: prescriptions, over-the-counter drugs, vitamins, supplements, eye drops, creams, and herbal remedies. Don’t assume it’s all there. If you’re unsure, ask: “Is this different from what I was taking before I came in?”
- Compare it to your home list. Take your pre-hospital meds list (or a recent pharmacy receipt) and line it up with the discharge list. Circle anything new, changed, or removed. Write down why - “Warfarin stopped because of surgery,” or “Metformin dose increased from 500mg to 1000mg.”
- Call your primary doctor or pharmacist within 48 hours. Don’t wait for your next appointment. Call your GP or community pharmacist. Say: “I was just discharged. Here’s my discharge med list. Can you help me check if this matches what I should be taking?” If you can’t reach them, call your hospital’s discharge follow-up line. Many now have pharmacists on call specifically for this.
Who’s Responsible? The Role of Doctors, Pharmacists, and You
Many patients think their doctor will handle everything. But the truth is, coordination falls through the cracks. Here’s who does what - and where the gaps are. Your discharge team (doctors, nurses) is supposed to create the discharge med list and explain changes. But they’re often rushed. A 2021 study found that 82% of primary care physicians say they don’t have enough time during follow-up visits to properly review meds. Your primary care provider (PCP) is supposed to reconcile your meds within 30 days. But if they don’t have access to your hospital records - or if the discharge summary is incomplete - they can’t do it right. And here’s the catch: only one person can bill Medicare for this service. That means your PCP and your cardiologist can’t both bill for the same discharge. So who steps up? Often, no one. Enter the pharmacist. In top-performing hospitals, pharmacists are embedded in discharge teams. They don’t just check lists - they call patients at home. They ask: “Did you fill your new prescription? Are you having side effects? Are you still taking your old meds?” One study showed pharmacist-led reconciliation reduced errors by 32.7%. They’re the missing link. And then there’s you. You’re the only person who knows what you actually took at home. You’re the only one who can say if a new pill makes you dizzy, or if your old blood pressure med was stopped without explanation. Your voice matters.
What to Do If Your Meds Don’t Match
Let’s say you get home and realize your discharge list says you’re now taking Lisinopril 10mg daily - but before the hospital, you were on Losartan 50mg. And your doctor never told you why. Or worse - your discharge list says “Discontinue Metformin,” but your blood sugar has been climbing since you got home. Here’s your action plan:- Don’t stop or start anything on your own.
- Call your pharmacy. Ask them to pull your pre-hospital fill history. They often have better records than your doctor.
- Take a photo of both lists - your old one and the discharge one - and send it to your GP’s office with a note: “Please review. These don’t match. What’s the plan?”
- If you’re unsure, ask for a medication therapy management (MTM) session. Many Medicare Advantage plans now cover this for free.
- If no one responds within 48 hours, call your hospital’s discharge coordinator. Ask: “Who is responsible for following up on this patient’s meds?”
Technology Can Help - But Only If You Use It
There are tools that can make this easier. But they’re only useful if you engage with them. Many hospitals now use apps where you can view your discharge meds on your phone. Ask if yours does. If not, use your own notes app. Create a simple list: Medication | Dose | Frequency | Reason for Change. Some pharmacies offer text reminders for new prescriptions. Sign up. Even better - use a pill organizer with alarms. Set it for the first 14 days after discharge, when mistakes are most common. New AI tools can scan your EHR and flag mismatches - but only if your hospital uses them. Ask your doctor: “Does your system check for drug interactions or missed meds after discharge?” If they say no, that’s a red flag. And don’t ignore the simple stuff: keep all your medication bottles in one place. Bring them to every appointment. Show them to your pharmacist. Seeing the actual pills helps catch errors no digital list can.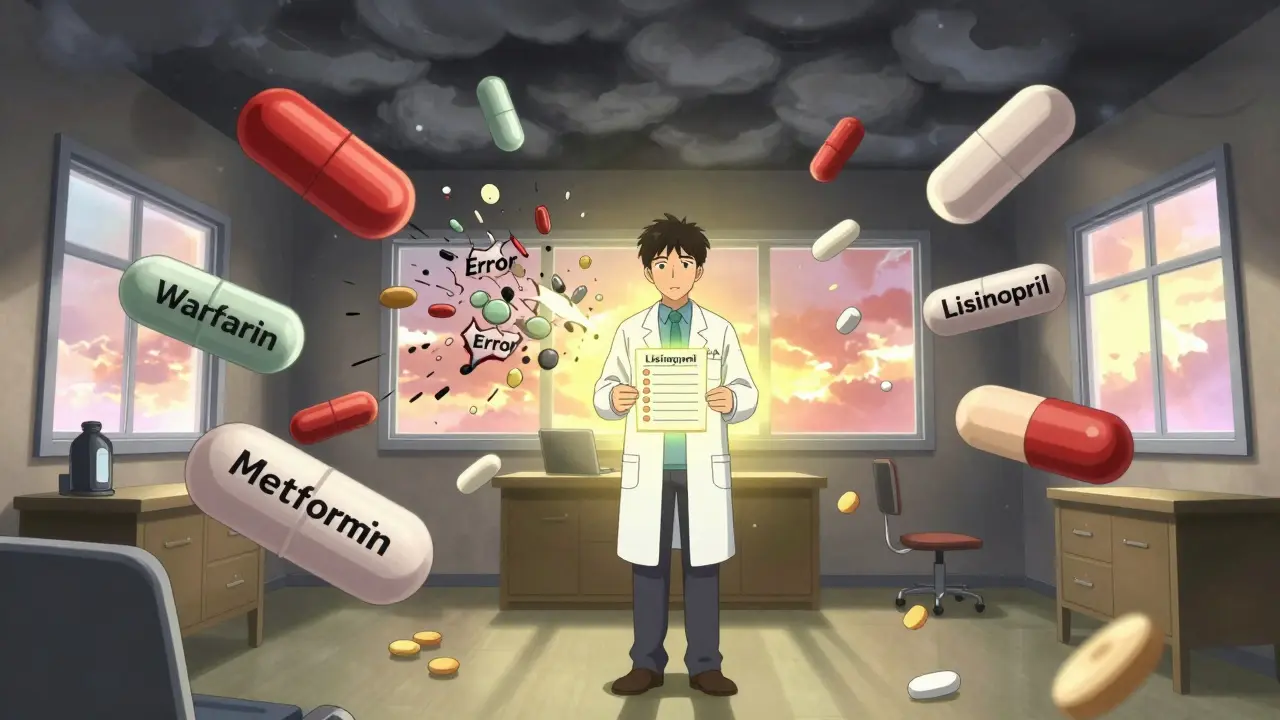
What Happens If You Don’t Do This?
Skipping medication reconciliation isn’t just risky - it’s common. And the consequences are real. - A patient stops taking their blood thinner after heart surgery because it wasn’t restarted. They have a stroke two weeks later. - Someone gets a new painkiller but keeps taking their old NSAID. They end up in the ER with a bleeding ulcer. - An elderly patient is discharged with six new meds and told to “take them as directed.” They don’t know what “as directed” means. They take them all at once. They’re hospitalized again. These aren’t hypotheticals. They happen every day. And they’re preventable. The cost? Over $21 billion a year in avoidable hospital readmissions. The human cost? Lost time, pain, fear - and sometimes, life.How to Make Sure This Doesn’t Happen to You
Here’s your checklist - print it or save it on your phone. Use it every time you’re discharged.- ☐ Get a written discharge medication list before leaving the hospital.
- ☐ Compare it to your home list - every single item.
- ☐ Note changes and reasons (e.g., “Stopped aspirin - surgery risk”)
- ☐ Call your GP or pharmacist within 48 hours - don’t wait.
- ☐ Bring all your pills to your next appointment.
- ☐ Ask: “Is this different from before? Why?”
- ☐ If you’re confused, ask for a pharmacist consult.
- ☐ If no one responds, call the hospital’s discharge follow-up line.
Final Thought: You’re Not Alone in This
The system isn’t perfect. But you don’t have to wait for it to fix itself. Every time you ask, “Why was this changed?” or “Can you check this list again?” you’re pushing the system to do better. And you’re protecting your health. Medication reconciliation isn’t just a hospital policy. It’s your right. And it’s your responsibility - to know your meds, to ask questions, and to make sure no one lets you fall through the cracks.What is medication reconciliation after hospital discharge?
Medication reconciliation is the process of comparing your current home medications with the list you were given when you left the hospital. The goal is to catch any changes, omissions, or errors that could cause harm - like taking a drug you shouldn’t, missing one you need, or getting the wrong dose. It’s a formal safety step required by Medicare and Medicaid to prevent dangerous mistakes after you leave the hospital.
Who is responsible for coordinating my meds after discharge?
Your hospital discharge team should create the initial list, but your primary care provider (PCP) or pharmacist is responsible for reviewing it within 30 days. However, many PCPs don’t have access to your hospital records or enough time to review everything. That’s why pharmacist-led reconciliation is becoming the gold standard - they’re trained to spot mismatches and follow up directly with patients. You can’t wait for someone else to fix it - you need to take the first step by calling your pharmacy or GP.
Can I use my pharmacy to help with medication reconciliation?
Yes - your pharmacy is one of your best resources. Pharmacists can pull your full prescription history, even before your hospital stay. They can tell you if a new prescription contradicts your old ones. Many pharmacies now offer free medication therapy management (MTM) sessions, especially if you’re on Medicare Advantage. Bring your discharge list and all your pill bottles - they’ll check for duplicates, interactions, and missed meds.
What if my doctor didn’t explain why a medication was changed?
That’s a red flag. Don’t assume it was intentional. Call your doctor’s office and say: “I noticed my medication changed from [old drug] to [new drug]. Can you explain why? Is this permanent?” If they can’t give you a clear reason, ask for a referral to a pharmacist or request a medication review. Some conditions - like kidney function or liver health - require dose changes, but you deserve to know why.
How soon after discharge should I get my meds reviewed?
Within 48 hours. The first week after discharge is when most errors happen - especially if you’re confused about new pills or side effects. Waiting until your next scheduled appointment (which might be weeks away) puts you at risk. Call your GP or pharmacist as soon as you get home. If you can’t reach them, call the hospital’s discharge follow-up line. Many hospitals now have pharmacists available for exactly this reason.
Is medication reconciliation covered by insurance?
Yes. Medicare and many private insurers cover post-discharge medication reconciliation under CPT codes 99495 and 99496 (for in-person visits) or through CPT II code 1111F (for documentation without a visit). Many Medicare Advantage plans also cover free medication therapy management (MTM) sessions. If your provider says it’s not covered, ask them to check again - it’s a federally mandated safety service.