Health January 26, 2026
How to Manage Medication Storage in Shared Living Spaces
Why Medication Storage in Shared Spaces Is a Silent Risk
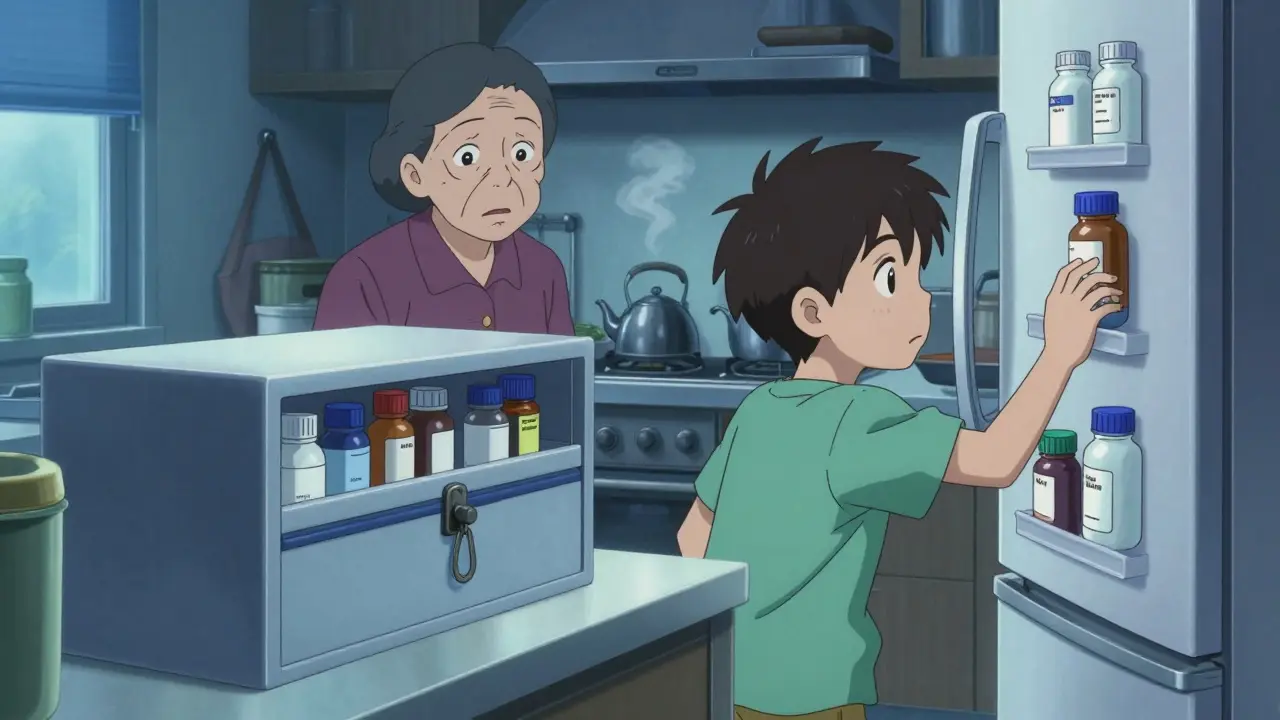
Imagine this: your teenager grabs what they think is cough syrup from the bathroom cabinet. It’s actually your dad’s painkiller. Or your elderly aunt’s insulin sits on the fridge door, where the temperature swings all day. By the time anyone notices, it’s too late. Medication storage in shared living spaces isn’t just about tidiness-it’s about preventing real harm. In multi-generational homes, assisted living facilities, or group households, one misplaced pill can lead to overdose, reduced effectiveness, or even death.
According to the Joint Commission, between 2020 and 2021, 13% of hospitals received citations for improper medication storage. That’s not just a hospital problem. The same risks exist in homes where multiple people share space. A 2025 survey by SeniorHelpers found that 67% of multi-generational households had at least one medication-related incident in the past year. Nearly half of those involved children accessing medicines stored in easy-to-reach places like bathrooms or kitchen counters.
What You Must Store Where: Temperature, Security, and Labels
Not all medications are created equal. Some need cold storage. Others must be locked away. And all of them need clear labels.
Refrigerated meds like insulin, certain antibiotics, and biologics must stay between 36°F and 46°F. That’s the center of the fridge-not the door. Door shelves can swing up to 10°F during normal use. One caregiver in Bristol reported her father’s blood sugar went wild after insulin sat on the fridge door for three weeks. The solution? A small, dedicated mini-fridge just for meds-or at least a clearly marked, sealed container on the middle shelf. Never store meds next to raw meat or dairy.
Controlled substances-opioids, benzodiazepines, stimulants-require locked storage. In care facilities, this means a locked cabinet with audit logs. At home, a simple lockbox with a combination or key works. The key is access control: only the person who needs the medication, or their designated caregiver, should be able to open it. A 2024 study showed that 78% of accidental overdoses in shared homes happened because controlled meds were left in unlocked drawers.
Labeling is non-negotiable. If a pill bottle says “Take once daily,” but no name or dosage is visible, someone else might take it. Always keep original packaging. If you transfer pills to a pill organizer, label each compartment with the full drug name, dose, and time. The Joint Commission found that 12% of hospitals failed on labeling compliance-and that’s in professional settings. In homes, it’s worse.
Storage Solutions: From Lockboxes to Dedicated Rooms
How you store meds depends on your living setup.
In assisted living or group homes, regulations require dedicated medication rooms or carts. Large facilities use automated dispensers with barcode scanning. Medium and small homes often use locked cabinets or drawers. But here’s the catch: 28% of small homes in one study had locked cabinets… but kept the key on a hook nearby. That’s not security. It’s theater.
In multi-generational homes, the best practice is bedroom-based storage. Each person gets a locked drawer or small safe near their bed. Why? Because it’s private, accessible only to them or their caregiver, and away from high-traffic areas like the kitchen or bathroom. A SeniorHelpers survey found that families using locked bedroom storage reported zero incidents-compared to 68% of those using bathroom cabinets who had at least one.
For households with kids or pets, a wall-mounted medicine safe (like those used for firearms) is ideal. They’re cheap, sturdy, and can be bolted down. Avoid glass-front cabinets or open shelves. Even if you think “no one would touch it,” curiosity and confusion make accidents inevitable.

What to Throw Out-and How
Expired, unused, or mismatched meds are a hazard. The FDA estimates that 70% of households have leftover pills from past prescriptions. These don’t just take up space-they’re temptation.
Start by collecting every pill bottle, patch, liquid, and inhaler in one place. Check expiration dates. Look for discoloration, strange smells, or crumbling tablets. If it’s been more than a year past its date, toss it. Some meds (like epinephrine auto-injectors) lose potency fast-even before the printed date.
Don’t flush them. Don’t throw them in the trash without mixing them with coffee grounds or cat litter first. The safest way? Use a drug take-back program. Many pharmacies in the UK now offer free drop-off bins. If none are nearby, mix meds with an unappealing substance (dirt, cat litter, used coffee grounds), seal in a plastic bag, and put it in the general waste. Remove personal info from bottles before recycling.
Documentation: The Invisible Shield
Professional care homes use Individualized Medication Administration Records (MARs). Every pill given, every time, is logged. In homes? Almost no one does this.
But you should. Even a simple notebook or digital note on your phone helps. Write down:
- Medication name and dose
- Time to take it
- Who gave it
- Any side effects observed
Why? Because memory fails. Especially when you’re tired, stressed, or juggling multiple people’s needs. One family in Bristol kept a handwritten log for their grandmother’s diabetes meds. When her blood sugar dropped suddenly, they checked the log and realized she’d been given double the dose the day before. They caught it before it became an emergency.
Training and Routine: Make It Stick
Storing meds safely isn’t a one-time setup. It’s a habit. And habits need reinforcement.
In care homes, staff get 8-12 hours of initial training, plus quarterly refreshers. At home? You need your own version. Hold a 15-minute family meeting every quarter. Walk through:
- Where each person’s meds are stored
- Who’s responsible for refills
- How to spot expired or damaged pills
- What to do if a pill is missing
Make it routine. Like checking smoke alarms. If you have a teenager or young adult living with you, explain why the locked box isn’t about distrust-it’s about safety. One 17-year-old told SeniorHelpers: “I thought my grandma’s meds were just old candy. Now I know they could kill me if I took one.”
What’s Changing: Smart Tech and New Rules
Medication storage is getting smarter. In 2024, companies like DosePacker launched smart cabinets that monitor temperature and humidity, log every access, and send alerts if something’s off. These are still pricey for homes-but they’re becoming more common in care facilities.
Regulations are tightening too. Since 2018, U.S. states have increased medication storage rules by 38%. The FDA updated its guidance in early 2024 for 47 common meds, clarifying exactly which ones need refrigeration. Even if you’re not in the U.S., these standards reflect global best practices.
For households, the biggest shift is awareness. SeniorHelpers launched a free medication safety certification for family caregivers in April 2025. Over 12,500 people signed up in the first month. It’s not about becoming a nurse-it’s about knowing the basics: lock it, label it, log it, and toss what’s expired.
What Happens When You Don’t Do This
Let’s be clear: skipping proper storage isn’t just risky-it’s common, and deadly.
A 2023 case in Bristol involved a 12-year-old who took her grandfather’s blood pressure pill, thinking it was candy. She ended up in the ER with dangerously low blood pressure. The pill bottle was on the nightstand-unlocked, unlabeled, and unattended.
Another case: a man’s antibiotics were stored in the fridge door. After two weeks, the drug degraded by 30%, according to Johns Hopkins. He got sicker. His infection didn’t clear. He needed a second round of treatment-and a hospital stay.
These aren’t rare. They’re predictable. And they’re preventable.
Start Today: Your 3-Step Action Plan
You don’t need a perfect system. You just need to start.
- Clear out the clutter. Gather every medication in your home. Toss expired, unused, or damaged ones safely. Don’t wait.
- Assign storage zones. Give each person a locked, labeled, temperature-appropriate spot. Bedroom drawers. Small lockbox. Dedicated mini-fridge. No exceptions.
- Set a reminder. Put a monthly calendar alert: “Medication Check.” Review labels, check expiration dates, confirm locks are working, and update your log.
It takes 20 minutes. And it could save a life.
Write a comment
Items marked with * are required.






13 Comments
TONY ADAMS January 27, 2026 AT 11:32
Bro, I saw my cousin's kid grab a bottle labeled 'sleep aid' and thought it was gummy vitamins. Next thing you know, she's napping on the floor for 3 hours. Lock it. Label it. Don't be lazy.
Ashley Porter January 28, 2026 AT 18:15
The fridge door temperature variance is a legit issue. I worked in pharma logistics-36–46°F is non-negotiable for biologics. Even a 5°F swing over weeks degrades potency. This post nails it.
Dan Nichols January 30, 2026 AT 04:42
So we're now criminalizing unsecured pill bottles like they're firearms? Next they'll make us sign a waiver before storing ibuprofen. This is overreach dressed as safety.
Peter Sharplin January 31, 2026 AT 10:09
I've managed meds for my mom with dementia and my nephew with ADHD. The locked bedroom drawer was the only thing that stopped two near-overdoses. Labeling each compartment with the full name and time? Game changer. Also, never assume someone knows what 'as needed' means-write it down. People forget under stress.
Henry Jenkins February 1, 2026 AT 13:29
I get the urgency, but the real problem isn't storage-it's systemic neglect. We treat medication safety like a household chore instead of a public health priority. Why aren't pharmacies required to hand out labeled, childproof containers with every script? Why do we expect families to become pharmacists overnight? The system fails us first; then we get blamed for not fixing it with a lockbox.
Allie Lehto February 3, 2026 AT 10:40
I'm so tired of people acting like this is just about 'being responsible.' My aunt died because her insulin was left on the fridge door for weeks and no one knew it was degraded. It's not negligence-it's ignorance. And ignorance is the real killer here. 😔
Skye Kooyman February 4, 2026 AT 08:31
My mom uses a pill organizer with labels. She forgets to refill it. We started using a Google Sheet with alerts. Now her meds are tracked. No drama. Just logistics.
Shawn Raja February 4, 2026 AT 14:38
We live in a world where you can't leave a bottle of aspirin unattended without a federal mandate. Next they'll require fingerprint scans to take Tylenol. Meanwhile, people are dying from bad water and food deserts. Priorities, people.
Rakesh Kakkad February 5, 2026 AT 20:24
In India, we often store medications in kitchen cupboards due to lack of dedicated space. But I’ve seen elderly relatives take wrong doses because labels faded or were in Hindi. The solution isn’t just lockboxes-it’s multilingual labeling and community health outreach. This isn’t just a Western problem.
Uche Okoro February 7, 2026 AT 10:16
The pharmacokinetic instability induced by suboptimal thermal exposure-particularly for monoclonal antibodies and insulin analogs-is empirically validated. The 30% degradation threshold observed in Johns Hopkins' 2023 study is corroborated by ICH Q1A guidelines. Storage protocols must align with pharmacopeial standards, not convenience.
Renia Pyles February 7, 2026 AT 16:12
Oh please. My brother’s ADHD meds were in a locked box. He still found the key under the rug. You can’t lock up human curiosity. This whole thing is performative safety.
Curtis Younker February 8, 2026 AT 17:47
I used to think this was overkill until my neighbor’s 8-year-old took his grandpa’s blood pressure med. Kid ended up in the ICU. We’re talking about life-or-death stuff here. It’s not about being paranoid-it’s about being prepared. I bought a wall-mounted safe for $40. Best money I ever spent. Now my whole family knows: meds = locked, labeled, logged. No exceptions. If you’re not doing this, you’re gambling with someone’s life.
James Nicoll February 9, 2026 AT 10:04
You know what’s wild? In Nigeria, we don’t have lockboxes. We have family elders who guard the meds like treasure. And guess what? It works. Because it’s not about the container-it’s about culture. The real solution isn’t tech-it’s teaching respect. A pill isn’t candy because it’s in a bottle. It’s candy because someone forgot to teach you it’s not.