Health January 30, 2026
Opioids and Low Testosterone: Symptoms and Treatment Options
Opioid-Induced Low Testosterone Screening Tool
Opioid-Induced Androgen Deficiency Assessment
This tool is based on the ADAM questionnaire (Androgen Deficiency in Aging Males) used by healthcare professionals to screen for low testosterone. Answer the following questions to assess your risk of opioid-induced low testosterone.
If you answered "Yes" to 3 or more questions, talk to your doctor about getting a testosterone test.
Your Assessment Results
Total "Yes" Answers: 0
Next Steps
Why Long-Term Opioid Use Can Crash Your Testosterone Levels
Most people know opioids help with pain, but few realize they can quietly shut down your body’s natural testosterone production. This isn’t rare-it happens in 50 to 90% of people taking opioids for more than a few months. The condition is called Opioid-Induced Androgen Deficiency, or OPIAD. It doesn’t show up on a scan or blood test right away. Instead, it creeps in slowly: low energy, no sex drive, mood swings, and weight gain that won’t go away no matter how hard you try. If you’ve been on opioids for over 90 days and notice these changes, your body might be telling you something serious is happening.
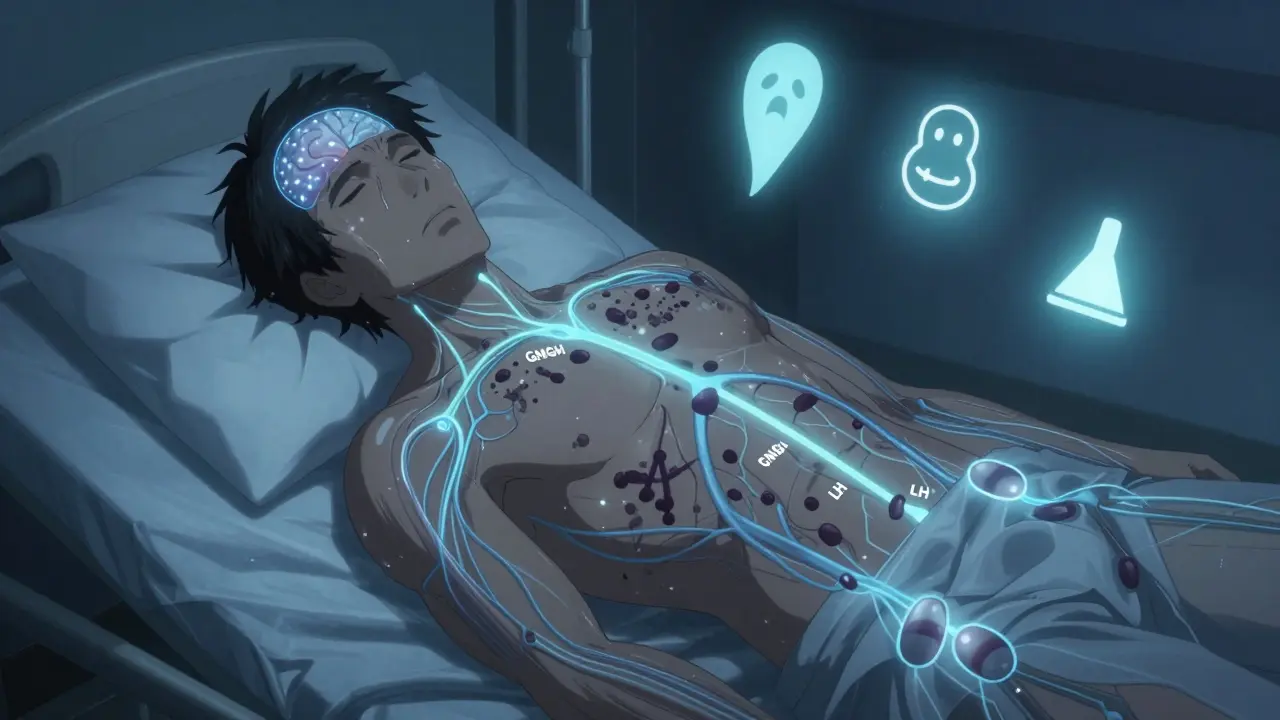
Opioids don’t just block pain signals-they mess with your brain’s hormone control center. When you take opioids regularly, they bind to receptors in your hypothalamus, the part of your brain that tells your body to make testosterone. This shuts down the signal chain: less GnRH → less LH → less testosterone. It’s like turning off a faucet at the source. Long-acting opioids like methadone and buprenorphine are especially bad at this. One study found men on methadone had testosterone levels averaging just 245 ng/dL, far below the normal range of 300-1000 ng/dL. Even buprenorphine, considered safer, still dropped levels to 387 ng/dL on average.
What Low Testosterone Feels Like When You’re on Opioids
If you’re on opioids and feel constantly tired, it’s easy to blame the pain or the medication. But fatigue isn’t the only symptom. In fact, it’s one of the least specific ones. The real red flags are sexual: 68-85% of men report low libido, and 60-75% struggle with erectile dysfunction. These aren’t just inconvenient-they’re signs your body isn’t producing enough testosterone.
Other symptoms are harder to connect to hormones. You might notice you’re losing muscle even if you’re still lifting weights. Your body fat, especially around your belly, might be creeping up. Your mood has changed-you’re irritable, down, or can’t focus. Studies show depression symptoms are 40% higher in opioid users with low testosterone. Even your bones are at risk: bone density in the spine can drop by 15-20%, raising your fracture risk. Your blood may be thinner too-hemoglobin levels often fall to 12.3 g/dL, well below the normal 14-18 g/dL, leading to anemia.
These symptoms don’t show up overnight. They usually develop over 3-6 months of continuous opioid use. That’s why many doctors miss it. Patients assume their fatigue is from pain, their low sex drive is from stress, and their weight gain is from inactivity. But when testosterone drops, all these problems pile up-and they get worse over time.
How Testosterone Replacement Helps-And What It Costs
If you’ve been on opioids long-term and your testosterone is low, replacement therapy can make a real difference. Testosterone replacement therapy (TRT) comes in several forms: injections every 1-2 weeks, gels applied daily, patches worn on the skin, or tablets stuck to your gum. The goal is to bring levels back into the healthy range: 350-750 ng/dL.
Research shows it works. In one trial, men on TRT saw their sexual function scores jump from 12.5 to 19.8 on a standard scale. Their muscle mass increased by 3.2 kg, while body fat dropped by 2.1 kg in just six months. Even more striking: those who got testosterone had a 49% lower risk of dying over time compared to those who didn’t. Their risk of heart attacks, strokes, hip fractures, and anemia also dropped significantly.
But TRT isn’t a magic pill. It requires monitoring. Blood tests are needed every 3-6 months after starting, then yearly. Prostate-specific antigen (PSA) levels must be checked every 6 months for men over 50 or those with a family history of prostate cancer. The FDA warns that testosterone therapy can increase the risk of blood clots, stroke, and heart problems-especially in older men or those with existing heart disease. It’s also strictly off-limits if you have prostate or breast cancer.
Side effects are common. About 15-20% of users develop polycythemia-too many red blood cells-which thickens the blood and raises stroke risk. Acne appears in 25% of those using gels or patches. HDL (good cholesterol) often drops by 10-15 mg/dL. These risks mean TRT should never be started without careful evaluation by a doctor familiar with endocrine disorders.

What to Do Before You Even Think About Testosterone
Before jumping to hormone therapy, there are natural ways to support your body. Many of these are already part of good health-but they’re especially important when you’re on opioids.
- Keep your weight in check. Men with a BMI under 25 have 20-30% higher testosterone than those who are overweight.
- Exercise regularly. Three strength-training sessions a week can boost testosterone by 15-25%. Even walking 30 minutes daily helps.
- Sleep 7-9 hours a night. Poor sleep cuts testosterone by 20%. If you’re on opioids, sleep disruption is common-addressing it can help.
- Avoid smoking. Smokers have 15-20% lower testosterone than non-smokers.
- Limit alcohol. More than 14 drinks a week reduces testosterone by 25%.
- Manage blood sugar. Diabetes cuts testosterone by 25-35%. If you’re prediabetic, now’s the time to act.
These steps won’t fully reverse OPIAD if your testosterone is severely low-but they can improve how you feel and reduce your need for medication. They also lower your risk of other opioid-related problems like heart disease and obesity.
Who Should Be Tested-and How
Screening for low testosterone should be routine for anyone on opioids for more than 90 days. But most doctors don’t do it. The American Pain Society and the Endocrine Society both recommend testing, yet only a small fraction of patients ever get their levels checked.
Testing requires two morning blood draws (between 7-10 a.m.) because testosterone levels naturally dip later in the day. You need both total and free testosterone measured. A single low result isn’t enough-you need two low readings at least a week apart to confirm hypogonadism.
Use the ADAM questionnaire (Androgen Deficiency in Aging Males) as a quick screen. Answer yes to three or more of these:
- Do you have a decreased sex drive?
- Do you lack energy?
- Do you have decreased strength or endurance?
- Have you lost height?
- Have you noticed decreased enjoyment of life?
- Do you feel sad or irritable?
- Are your erections less strong?
- Have you noticed a recent decrease in sports performance?
- Do you feel more tired after a full day?
- Do you have decreased work performance?
If you answer yes to three or more, ask your doctor for a blood test. Don’t wait for symptoms to get worse.

The Big Debate: Is Testosterone Therapy Safe for Opioid Users?
Not everyone agrees on whether to treat OPIAD with testosterone. The VA Whole Health Library warns that testosterone therapy is being pushed by drug companies and says, “Once you start, your body stops making its own.” That’s true-TRT suppresses natural production. But the alternative is leaving a man with low energy, poor sex life, weak bones, and higher death risk.
Here’s the reality: OPIAD is real. The data is clear. Men on long-term opioids have half the testosterone of healthy men. Their quality of life suffers. Their mortality risk rises. And TRT, when carefully managed, reduces those risks.
Doctors who avoid TRT often cite lack of long-term safety data. That’s fair-but the same could be said for many medications we routinely prescribe. The key is not to avoid treatment, but to do it right: screen first, monitor closely, use the lowest effective dose, and combine it with lifestyle changes.
For women on opioids, the picture is less clear. Some studies suggest DHEA supplementation might help, but evidence is limited. More research is needed.
What’s Next? The Future of Opioid-Related Hormone Problems
As opioid use continues-whether for chronic pain or addiction treatment-OPIAD will remain a hidden epidemic. Globally, over 58 million people used opioids in 2022. Even if only half develop low testosterone, that’s millions of people living with unexplained fatigue, depression, and sexual dysfunction.
Future research needs to answer key questions: What’s the safest way to taper opioids while starting testosterone? Can we restore natural hormone production after stopping opioids? Are there alternatives to TRT that don’t suppress the body’s own production?
For now, the message is simple: If you’re on opioids long-term, don’t ignore your symptoms. Ask for a testosterone test. Talk to your doctor about TRT if your levels are low. And don’t underestimate the power of sleep, exercise, and weight control. Your body is trying to tell you something-and it’s not just about pain anymore.
Can opioids cause permanent low testosterone?
In most cases, no. Testosterone levels usually rebound after stopping opioids, but it can take months or even over a year. For some men with very long-term use (5+ years), recovery may be incomplete. That’s why early detection and treatment matter-waiting too long can damage the body’s ability to restart natural production.
Is testosterone therapy addictive?
Testosterone itself isn’t addictive like opioids. But people can become dependent on the feeling it gives-more energy, better mood, improved sex drive. Stopping abruptly can cause a crash in energy and mood. That’s why tapering under medical supervision is important. It’s not addiction-it’s physiological dependence, similar to stopping thyroid or steroid medication.
Can women on opioids also get low testosterone?
Yes, though it’s less studied. Women produce small amounts of testosterone in their ovaries and adrenal glands. Opioids can suppress this too, leading to low libido, fatigue, and mood changes. DHEA supplementation has been used experimentally, but evidence is limited. Women should have their hormone levels checked if symptoms persist.
How long does it take for testosterone therapy to work?
Some symptoms improve quickly: libido and mood often improve within 2-4 weeks. Muscle strength and energy take longer-usually 8-12 weeks. Bone density and fat loss may take 6 months or more to show measurable change. Patience is key, and tracking symptoms helps you see progress.
Should I stop opioids to fix my testosterone?
Not necessarily. If you’re on opioids for chronic pain, stopping abruptly can be dangerous. Many men benefit from staying on a stable dose while starting testosterone therapy. The goal isn’t always to quit opioids-it’s to treat both the pain and the hormone imbalance at the same time. Work with a pain specialist and endocrinologist to find the right balance.
Are there any natural supplements that help?
Zinc, vitamin D, and ashwagandha have shown modest benefits in general low testosterone cases, but none have been proven to reverse OPIAD. They might help a little, but they won’t fix the core problem: opioid suppression of the HPG axis. Don’t rely on supplements alone. Focus on lifestyle changes and medical treatment if your levels are low.
Next Steps: What to Do Today
If you’re on long-term opioids and feel off-tired, low in mood, or losing interest in sex-don’t wait. Schedule a blood test for total and free testosterone. Bring the ADAM questionnaire results with you. Ask your doctor if TRT is right for you. If they say no, ask why-and request a referral to an endocrinologist.
Start making small changes now: walk every day, sleep 8 hours, cut back on alcohol, and get your weight checked. These steps won’t fix everything-but they’ll give your body a fighting chance. Opioids don’t have to steal your vitality. With the right approach, you can take it back.
Write a comment
Items marked with * are required.





8 Comments
Nicki Aries February 1, 2026 AT 04:37
This is why so many guys on opioids just give up on life. No energy, no libido, no motivation. It's not 'just pain'-it's your body shutting down. And doctors act like it's normal. Bullshit.
Lisa Rodriguez February 1, 2026 AT 09:20
I'm a nurse and I've seen this over and over. Men come in saying they're 'just tired'-but their partner says they haven't had sex in a year, they're crying over nothing, and they've gained 40 pounds. They don't connect the dots. This post? It's a lifeline.
Naresh L February 1, 2026 AT 21:11
It's fascinating how the brain's reward and hormonal systems are so deeply intertwined. Opioids hijack the HPG axis not as a side effect, but as a direct neurological override. The body doesn't 'forget' how to make testosterone-it's forced into suspended animation. Recovery isn't guaranteed because the system gets conditioned to dependence. This isn't just medicine-it's neurobiology.
Sami Sahil February 2, 2026 AT 10:59
Dude i was on methadone for 3 years and my testo was at 210. Started TRT and my life changed. I could lift again. I wanted to go out. I stopped hating my wife. It wasnt magic-i still had to sleep and eat right. But without TRT? I was a ghost.
franklin hillary February 2, 2026 AT 20:34
Let me be blunt: if you're on opioids longer than 90 days and you're not getting your testosterone checked, you're being neglected. This isn't a niche issue-it's a public health crisis hiding in plain sight. We treat depression, we treat obesity, we treat anemia-but we ignore the root cause? That's not medicine. That's negligence. And the fact that the VA warns against TRT while ignoring the death stats? That's politics, not science.
Rachel Liew February 4, 2026 AT 10:11
i just found out my husband’s testo is low and he’s been on oxycodone for 2 years. i never knew this could happen. thank you for writing this. we’re going to the doctor next week. he’s been so down and i thought it was me. it’s not me. it’s the meds.
Ed Di Cristofaro February 4, 2026 AT 20:47
So now we're giving hormone shots to people who got addicted to painkillers? What's next? Free vitamins for people who eat 12 donuts a day? Take responsibility. Stop the opioids. Fix your life. Don't just swap one dependency for another.
Nicki Aries February 5, 2026 AT 22:37
You think it's that simple? Try telling that to someone with a crushed spine who can't walk without 80mg of oxycodone a day. You want them to quit cold turkey and just 'fix their life'? That's not tough love-that's cruelty. TRT isn't a crutch. It's restoring what the opioids stole. And if you don't get it, maybe you've never lived in real pain.