
Health December 3, 2025
Telemedicine Prescriptions and Generics: What You Need to Know in 2025
When you need a refill for your generic sertraline or buprenorphine, you might not think twice about getting it through a telemedicine visit. But behind that simple click-and-send prescription is a tangled web of federal rules, state laws, and technical hurdles that change how-and if-you can get your meds online. In 2025, telemedicine prescriptions aren’t just convenient-they’re regulated in ways most patients and even some doctors don’t fully understand.
What’s Allowed and What’s Not
Not all medications are treated the same under telemedicine rules. Generic medications that aren’t controlled substances-like sertraline, metformin, or lisinopril-can be prescribed remotely with almost no restrictions. You can get a 90-day supply, renew it monthly, and have it sent to any pharmacy that accepts e-prescriptions. No in-person visit needed. That’s because the DEA doesn’t regulate these drugs the same way it does opioids, stimulants, or sedatives.
But if your prescription is for a Schedule III-V controlled substance-like generic buprenorphine for opioid use disorder, or Adderall (Schedule II)-you’re in a different world. The DEA’s new rules, finalized in early 2025, created three separate registration paths for providers. Only certain specialists can prescribe Schedule II drugs via telemedicine: board-certified psychiatrists, neurologists, pediatricians, hospice doctors, and those treating long-term care patients. General practitioners? Not unless they can prove a "compelling use case," and even then, it’s rare.
For Schedule III-V drugs like buprenorphine, the rules are slightly more flexible. You can get an initial six-month supply via telemedicine without ever stepping into a clinic. But after that? You must either have an in-person visit or continue under strict conditions. That six-month cap is a major pain point for rural patients who travel hours to see a specialist. Clinical guidelines say 12 months of medication-assisted treatment leads to the best outcomes. The rules don’t match the science.
The Hidden Rules: PDMP, EPCS, and Identity Checks
It’s not just about what you can prescribe-it’s how you prescribe it. Every telemedicine prescription for a controlled substance must be sent electronically through EPCS (Electronic Prescribing of Controlled Substances). That means your provider needs special software certified by the DEA. Over 90% of telehealth platforms now use EPCS, but that’s just the start.
Before writing any controlled substance prescription, providers must check your state’s Prescription Drug Monitoring Program (PDMP). This is a database that tracks who’s getting what, when. Sounds reasonable-until you realize there are 50 different PDMP systems, none of them talk to each other well. A doctor in Montana prescribing to a patient in Wyoming has to log into three separate state databases. Each check takes 5-10 minutes. Multiply that by 20 patients a day, and you’re adding hours to your schedule.
And you have to prove who you are. No more just saying your name and birthdate. You need to show a government-issued photo ID during the video call-driver’s license, passport, military ID. The provider must document the exact time and date they verified your identity. If they miss one of these steps, the pharmacy can-and will-refuse to fill the prescription.
Why Your Prescription Gets Rejected
It’s not always about the doctor. Often, the pharmacy is the bottleneck. Many community pharmacists haven’t been trained on the new DEA rules. A patient in Nevada gets a valid buprenorphine prescription from a California-based telehealth provider. The pharmacy in Nevada says no-"We don’t accept out-of-state telemedicine prescriptions for controlled substances." But under federal law, they should. The DEA says location doesn’t matter as long as the provider is licensed and compliant. But local pharmacies? They’re scared. They’ve been burned before. So they play it safe and deny.
Another big reason prescriptions get denied? Incomplete documentation. In Q1 2025, 42% of DEA registration applications were rejected because providers didn’t properly log their PDMP checks. That means even if the doctor meant to follow the rules, a missing timestamp or incorrect form can shut down the whole process.
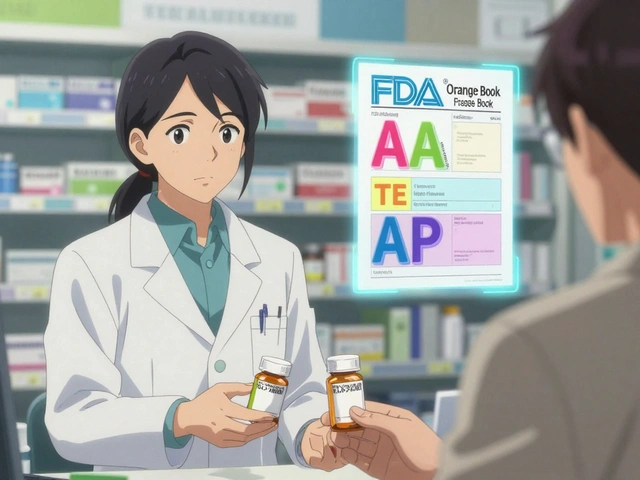
Generics vs. Controlled Substances: A Double Standard
Here’s the real kicker: you can get a generic version of your antidepressant or blood pressure med with zero restrictions. But if that same generic is a controlled substance-like buprenorphine-it’s treated like a high-risk drug. That’s not based on safety. Buprenorphine is safer than many non-controlled drugs. It’s about history. The DEA’s rules are still shaped by the opioid crisis, not current evidence.
This creates a bizarre situation. Two patients with the same condition-say, depression with anxiety-might both need sertraline. One gets it easily via telehealth. The other needs buprenorphine for opioid withdrawal. They’re both generics. They’re both effective. But one has a six-month clock ticking, and the other doesn’t. That’s not medicine. That’s bureaucracy.
Who’s Getting Left Behind
Primary care doctors-especially in rural areas-are being pushed out of the loop. The DEA’s new rules explicitly exclude most family physicians from prescribing Schedule II-V drugs via telemedicine. But here’s the truth: 80% of people with opioid use disorder first seek help from their regular doctor, not a specialist. Now those doctors can’t help. Patients are forced to travel to urban clinics, wait months for appointments, or go without.
Medicare adds another layer. Starting October 1, 2025, Medicare patients must have had an in-person mental health visit before they can get continued telehealth care. That’s a huge blow to people who rely on telemedicine because they can’t drive, don’t have childcare, or live in areas with no providers. It could cut reimbursement for telemedicine prescriptions by nearly half.
What You Can Do
If you’re using telemedicine for generics like antibiotics, thyroid meds, or birth control-you’re fine. Just make sure your provider uses a reputable platform that does EPCS and ID verification if you’re getting anything controlled.
If you’re on buprenorphine or another Schedule III-V drug:
- Ask your provider if they’re registered under the Telemedicine Prescribing Registration category.
- Confirm they check PDMPs for every state you’ve lived in over the past year.
- Have your photo ID ready during every visit-even if you’ve used the service before.
- Call your pharmacy ahead of time to ask if they accept telemedicine prescriptions for controlled substances.
- Keep a copy of your prescription and the provider’s DEA number. If it’s denied, you can file a complaint with the DEA’s Diversion Control Division.
And if you’re a provider? Get certified in EPCS. Learn your state’s PDMP system. Document everything. The paperwork is brutal, but the alternative is losing your ability to prescribe.
The Future: What’s Coming Next
The current emergency flexibilities expire December 31, 2025. After that, the new DEA rules are locked in. There’s talk of another extension, but industry analysts give it a 30% chance. The DEA is spending $127 million to build a national PDMP system-but experts say it won’t be fully functional until late 2027. Until then, providers are stuck with a patchwork of broken state systems.
Meanwhile, non-controlled generics are booming. The telemedicine market for these drugs is growing at 28% per year. They’re the future of digital health. Controlled substances? They’re stuck in regulatory limbo. The system isn’t broken because it’s flawed-it’s broken because it’s trying to solve a decade-old crisis with 1990s-era tools.
For now, if you need a refill on your generic meds, telemedicine works. But if you need something controlled, you’re navigating a minefield. The rules are changing. The tech is lagging. And the people who need help the most? They’re the ones paying the price.
Write a comment
Items marked with * are required.



13 Comments
Benjamin Sedler December 5, 2025 AT 05:35
Let me get this straight-you can get a 90-day supply of sertraline like it’s candy, but if you need buprenorphine to not die, you’ve got to jump through 17 hoops and beg a specialist who’s booked for six months? This isn’t healthcare. This is a bureaucratic snuff film where the DEA is the director and patients are the extras. And don’t even get me started on pharmacies refusing out-of-state scripts. You’d think we were smuggling heroin, not treating addiction. Someone please tell me why we treat mental health like it’s a felony.
Gareth Storer December 6, 2025 AT 01:50
Oh wow, a 12-page essay on why bureaucracy is bad. Groundbreaking. Next up: ‘Water is wet and gravity still exists.’ I’m just waiting for the 2026 update titled ‘Why Your Toaster Still Doesn’t Need a DEA License.’
Pavan Kankala December 7, 2025 AT 22:03
They don’t want you to know this, but the DEA’s rules were written by pharmaceutical lobbyists who own half the telehealth platforms. Buprenorphine is cheaper than opioids, so the pharma giants push for restrictions to keep people on brand-name drugs like Suboxone. Meanwhile, your grandma’s metformin? Free as air. Why? Because no one’s making billions off it. This isn’t regulation-it’s capitalism with a stethoscope.
And the PDMP systems? They don’t talk because they’re owned by different tech companies who charge states $50k/year to ‘interface.’ The whole system’s rigged. You think this is about safety? Nah. It’s about profit. Wake up.
Jessica Baydowicz December 8, 2025 AT 20:54
Ugh, I just got my sertraline refill via telehealth and I’m so grateful! 😊 But reading this made me cry for my cousin who’s on buprenorphine and has to drive 3 hours every 5 months just to get a checkup. It’s not fair. Why can’t we just treat people like humans? We’ve got the tech, we’ve got the data-why are we still stuck in the 90s? Let’s fix this! 💪❤️
Yasmine Hajar December 10, 2025 AT 02:54
I’m a nurse in rural Ohio, and I see this every single day. One guy got his buprenorphine script denied because the pharmacy thought ‘California telehealth’ meant ‘drug dealer.’ He cried in my office. I had to call the DEA hotline myself to get it cleared. And you know what? The DEA rep was nice, but said ‘We’re aware, but we’re understaffed.’ That’s not a solution. That’s a shrug. We need to train pharmacists. We need to fix the PDMP mess. We need to stop punishing people for needing help.
And yes, I’ve had patients show me their ID with tears in their eyes because they’re scared they’ll be turned away again. This isn’t policy. This is trauma.
Karl Barrett December 11, 2025 AT 01:50
Structural hermeneutics of pharmaceutical governance reveals a deeper epistemic rupture: the ontological privileging of non-controlled substances as ‘safe’ and ‘routine,’ while controlled substances are ontologized as ‘risky’-a discursive construction rooted in moral panic rather than pharmacological evidence. The DEA’s regulatory architecture operates under a Foucauldian biopolitical framework, where the body is subjected to surveillance protocols (PDMP, EPCS, ID verification) that function as technologies of power, not care. The asymmetry between sertraline and buprenorphine is not accidental-it is the logical outcome of a regulatory system that conflates addiction with criminality, and recovery with compliance.
Thus, the real crisis isn’t logistical-it’s epistemological. We have the tools. We lack the will to deconstruct the myth of the ‘addict’ as deviant.
Jake Deeds December 11, 2025 AT 19:12
I’m sorry, but if you’re getting buprenorphine via Zoom, you’re basically asking for trouble. I’m not saying you’re a junkie-I’m saying the system is designed to prevent abuse. If you can’t even go to a clinic once every six months, maybe you’re not ready for recovery. This isn’t about ‘access,’ it’s about responsibility. You wouldn’t let someone order a gun online without a background check-why treat addiction differently? Just saying.
Elizabeth Crutchfield December 12, 2025 AT 07:59
so like… i just got my buprenorphine refill and the pharmacy said no? i was like ‘wait what’? i showed them the script, the DEA num, everything. they said ‘we dont do tele for that here’. i called my doc and he was like ‘yeah they do that all the time’. so now i have to drive 45 min to a different pharmacy. its 2025. we have drones. why cant my meds just… come?
Ben Choy December 13, 2025 AT 07:20
This is such a mess, but I’m glad someone finally spelled it out. I work in telehealth IT and we had to rework our whole system last year to handle PDMP checks across 5 states. It’s a nightmare. But I’ve seen patients get their meds because someone took the time to call the pharmacy and explain the rules. Small wins. Keep fighting. 🤝
Chad Handy December 13, 2025 AT 10:08
Let’s be real-this whole system is designed to fail. The DEA doesn’t care about patients. They care about headlines. They care about looking tough on drugs. Meanwhile, people are dying because they can’t get their meds. And the worst part? The people who designed this system will never be the ones waiting for a 90-minute Zoom call with a doctor who’s on a 12-hour shift. They’re sipping lattes in D.C. while someone in West Virginia sits in their car crying because they missed their refill window. This isn’t a policy issue. It’s a moral failure. And it’s going to keep happening until the people in charge feel the pain. And they won’t. Because they’re not the ones suffering.
Jenny Rogers December 14, 2025 AT 01:10
It is imperative to note that the current regulatory framework governing telemedicine prescriptions for controlled substances is not merely a procedural inconvenience-it is a necessary safeguard against the proliferation of substance misuse, which, as documented by the CDC, remains a leading cause of preventable mortality in the United States. The requirement for in-person verification and PDMP consultation is not arbitrary; it is empirically grounded in longitudinal studies demonstrating reduced diversion rates when multi-layered authentication protocols are enforced. To suggest that these measures are outdated is to conflate accessibility with accountability, a dangerous fallacy.
Furthermore, the notion that buprenorphine is ‘safer’ than non-controlled substances is a misrepresentation of risk profiles. While its overdose potential is lower than full agonists, its pharmacological profile still necessitates clinical oversight. The fact that sertraline is non-controlled does not imply equivalence in therapeutic risk. The distinction is not a double standard-it is a scientifically calibrated distinction.
One cannot advocate for expanded access without acknowledging the responsibility inherent in such access. To do so is to prioritize convenience over public health.
Scott van Haastrecht December 14, 2025 AT 22:21
Oh my god, I knew it. This is why I don’t trust telemedicine. They let anyone with a laptop prescribe meds. And now you’re telling me they’re giving out buprenorphine like it’s a coupon? What’s next? Online Xanax with free shipping? This is how the opioid crisis got worse. You think this is ‘access’? It’s a loophole for dealers and lazy doctors. And now Medicare’s making it worse by forcing in-person visits? Finally, someone with sense. Let’s not turn healthcare into Amazon Prime.
Chase Brittingham December 16, 2025 AT 12:10
I just want to say thank you to everyone who’s fighting to make this system better. I’ve been on buprenorphine for 3 years via telehealth. I’ve had my script denied three times because of pharmacy ignorance. But I’ve also had pharmacists call me personally to say ‘I’m sorry, I didn’t know’-and then fix it. We’re not broken. The system is. But people? People are still good. Keep speaking up. Keep calling. Keep showing up. You’re not alone.