
Health December 31, 2025
Thyroid Ultrasound: How Imaging Nodules Reveals Cancer Risk
When your doctor finds a lump in your neck, the first test you’ll likely get isn’t a biopsy, not a scan with radiation, and not even a blood test. It’s a thyroid ultrasound. This simple, painless procedure uses sound waves to paint a detailed picture of your thyroid gland-and it’s the single most important tool doctors have to figure out whether a nodule might be cancerous.
Why Ultrasound Is the First Step
You might think a biopsy is the obvious first move when a nodule is found. But that’s not how it works. Ultrasound comes first because it’s safe, fast, and tells doctors more than any other test can. Unlike CT or MRI, which can spot a nodule by accident, ultrasound shows exactly what the nodule looks like: its shape, texture, and blood flow. It’s like having a magnifying glass for your thyroid. Studies show that up to 68% of people have thyroid nodules when scanned with ultrasound-far more than the 2-21% found by just feeling the neck. And here’s the key: most of these nodules are harmless. But ultrasound helps separate the ones that need attention from the ones that don’t.What Ultrasound Looks For: The Five Warning Signs
Radiologists don’t just glance at the image. They check five specific features that raise red flags:- Composition: Is the nodule solid, filled with fluid, or a mix? Solid nodules are more concerning than cysts.
- Echogenicity: How bright or dark does it look? Markedly hypoechoic (very dark) nodules are more likely to be cancerous.
- Shape: A nodule that’s taller than it is wide is a major warning sign. Normal nodules are wider than they are tall.
- Margin: Smooth edges? Probably fine. Jagged or spreading beyond the thyroid? That’s trouble.
- Punctate echogenic foci: Tiny white dots inside the nodule-these are microcalcifications. They’re one of the strongest predictors of cancer.
These features aren’t just opinions. They’re part of a standardized scoring system called TI-RADS, developed by the American College of Radiology in 2017. Each feature gets 0 to 3 points. Add them up, and you get a risk category.
Understanding TI-RADS Risk Levels
TI-RADS turns those five features into clear risk levels:- TR1 (0 points): 0.3% chance of cancer. No follow-up needed.
- TR2 (2 points): 1.5% risk. Still very low. Usually just monitor.
- TR3 (3 points): 4.8% risk. Mildly suspicious. Usually biopsy if over 2.5 cm.
- TR4 (4-6 points): 9.1% risk. Moderately suspicious. Biopsy recommended at 1 cm or larger.
- TR5 (7+ points): 35% risk. Highly suspicious. Biopsy almost always needed.
These numbers aren’t guesses. They’re based on data from tens of thousands of patients. For example, a nodule with microcalcifications, solid composition, and central blood flow has a 3 to 5 times higher chance of being cancer than one without them.
What Ultrasound Can’t Do
It’s important to understand what ultrasound can’t tell you. It can’t say for sure if a nodule is cancerous. Only a biopsy can do that. Ultrasound only estimates risk. That’s why even a TR5 nodule needs a needle biopsy before surgery. Also, ultrasound struggles with nodules that are deep in the chest (substernal goiters) or those with unclear features. In those cases, doctors may turn to other tools-but only after ultrasound has done its job.Why Not Just Use a CT or MRI?
CT and MRI scans can show thyroid nodules, but they’re like using a sledgehammer to crack a nut. They miss the fine details that matter: microcalcifications, shape, and internal blood flow. Plus, they expose you to radiation (CT) or are much more expensive (MRI). Nuclear scans (like radioactive iodine uptake tests) can tell you if a nodule is “hot” (overactive) or “cold” (underactive). Hot nodules are almost never cancerous. Cold ones have a 15% risk. But here’s the catch: nuclear scans can’t show you the nodule’s shape or calcifications. So even if you have a cold nodule, you still need an ultrasound to decide if you need a biopsy.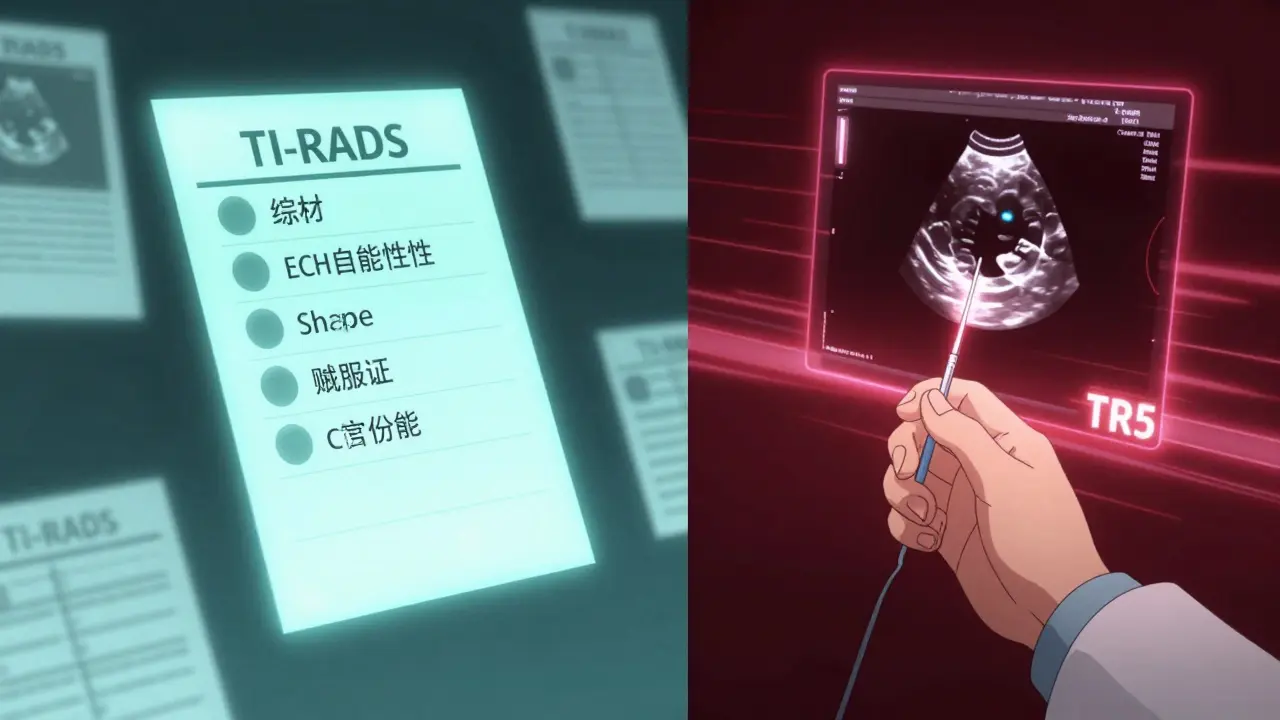
When Do You Need a Biopsy?
Not every nodule needs a biopsy. Size matters-but so does appearance.- Nodules under 5 mm: No biopsy, no follow-up. Even if they look suspicious, they’re too small to be dangerous.
- Nodules 1 cm or larger with TR4 or TR5 features: Biopsy recommended.
- Nodules 2.5 cm or larger with TR3 features: Biopsy recommended.
Why 2.5 cm? Because research shows thyroid cancers under that size rarely spread or cause harm. Many doctors now watch small, low-risk cancers with regular ultrasounds instead of rushing to surgery. Studies show 10-year survival rates are over 99% with active monitoring.
The Role of AI and New Technology
Ultrasound tech isn’t standing still. In 2023, a study in Nature Scientific Reports showed a new AI model could analyze ultrasound images with 94.2% accuracy-better than most human radiologists. The model learned to spot subtle patterns, like how the nodule’s shape relates to its internal structure. AI isn’t replacing doctors. It’s helping them. Some hospitals are already using AI tools to flag suspicious nodules during scans, reducing missed diagnoses. The American College of Radiology plans to update TI-RADS in 2024 to include AI-assisted features. Another emerging tool is elastography, which measures how stiff a nodule is. Cancerous tissue tends to be stiffer than healthy tissue. Contrast-enhanced ultrasound, which uses tiny bubbles to highlight blood flow, is also being tested-but neither is standard yet.What Happens After the Scan?
If your nodule is low-risk (TR1 or TR2), you’ll likely get a repeat ultrasound in 1-2 years. No biopsy. No treatment. Just watch. If it’s TR3 or higher, you’ll probably get a fine-needle aspiration (FNA). This is done right in the doctor’s office. The ultrasound guides the needle to the exact spot, making the sample more accurate. Without ultrasound guidance, up to 25% of biopsies give unclear results. With it, that drops below 5%. If the biopsy is indeterminate (about 1 in 5 cases), molecular testing can help. These tests look for specific gene mutations linked to cancer. They’ve cut unnecessary surgeries by half. But even if the test says “benign,” you still need follow-up ultrasounds. Cancer can grow slowly-and ultrasound catches it early.Who Should Get a Thyroid Ultrasound?
Guidelines are clear: anyone with a thyroid nodule-whether found by you, your doctor, or during another scan-should get an ultrasound. It’s not just for people with symptoms. Many nodules are found by accident during imaging for other reasons. The American Academy of Family Physicians and the American Thyroid Association both recommend ultrasound for all patients with nodules. Even if your thyroid hormone levels are normal. Even if you feel fine.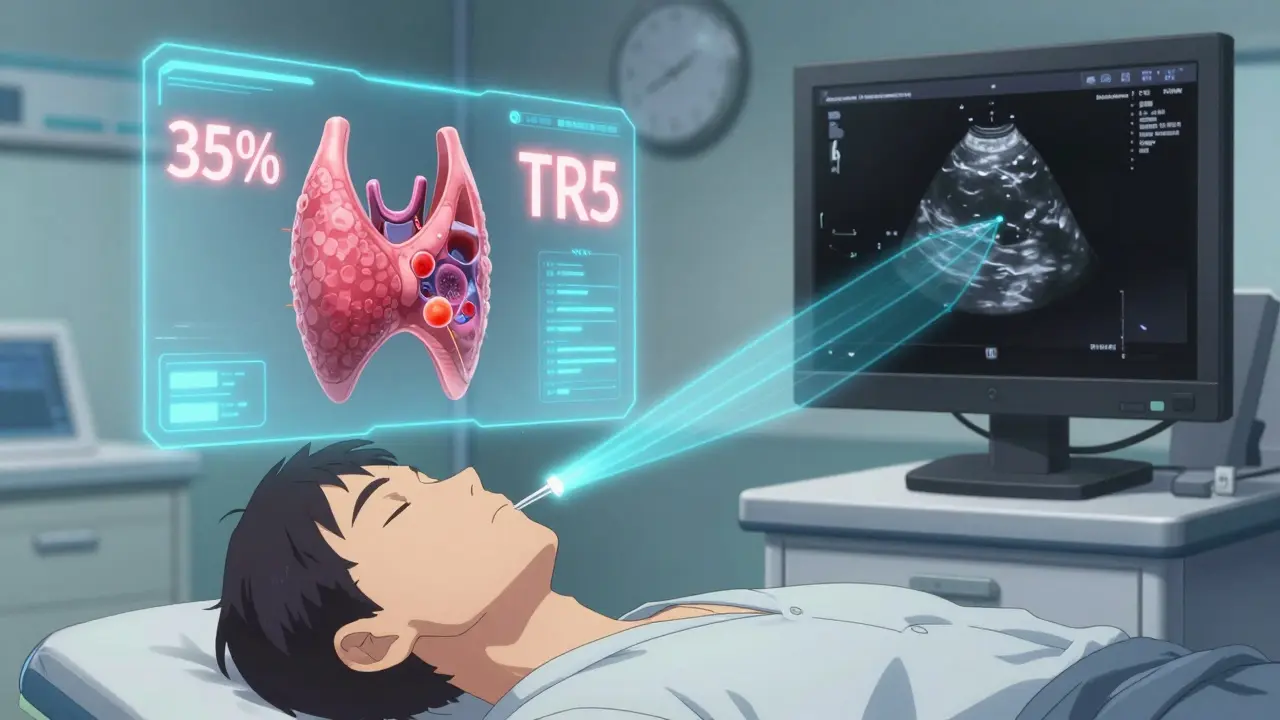
What to Expect During the Test
There’s no preparation. No fasting. No needles. You lie on your back with your neck exposed. A gel is applied, and a small handheld probe is moved gently over your skin. The whole thing takes 15-20 minutes. You might hear a whooshing sound-that’s the Doppler showing blood flow. The technician will take pictures of the nodule from different angles. They’ll also check your neck lymph nodes. That’s critical. Cancer can spread to lymph nodes, and missed lymph node evaluation happens in 35% of community clinics.How Accurate Is It?
Ultrasound is highly accurate-but only if done well. Training matters. A radiologist needs to do 200-300 supervised scans before they can reliably use TI-RADS. Inter-observer variability is still a problem: two doctors might disagree on whether a margin is smooth or jagged. That’s why accreditation matters. Facilities with AIUM or ACR accreditation have proven they meet strict standards for image quality and interpretation. Ask your provider if they’re accredited.What’s Next for Thyroid Ultrasound?
The future is integration. Doctors are starting to combine ultrasound risk scores with molecular test results to create personalized cancer risk profiles. One expert predicts that within five years, we’ll have a single number-like a “thyroid cancer risk score”-that tells you exactly what to do next. The goal? Reduce unnecessary biopsies without missing cancers. Right now, we biopsy too many benign nodules. But we also miss some cancers. Better tools will fix both.Final Thoughts
Thyroid ultrasound isn’t magic. But it’s the best tool we have. It’s safe, affordable, and gives more information than any other test. It doesn’t diagnose cancer-but it tells you whether you’re likely to need a biopsy. And that’s enough to save lives. If you’ve been told you have a nodule, don’t panic. Ask for an ultrasound. Ask about TI-RADS. Ask if your provider is accredited. Knowledge is power-and ultrasound gives you the clearest picture of what’s really going on.Is thyroid ultrasound painful?
No. It’s completely painless. You’ll feel slight pressure from the probe and cold gel on your neck, but no needles or discomfort. It’s similar to a prenatal ultrasound.
Can ultrasound diagnose thyroid cancer?
No. Ultrasound can only assess the risk of cancer based on nodule features. Only a biopsy can confirm whether a nodule is cancerous. Ultrasound helps decide if a biopsy is needed.
How often should I get a follow-up ultrasound?
For low-risk nodules (TR1-TR2), follow-up is usually every 1-2 years. For higher-risk nodules (TR3-TR5), follow-up depends on biopsy results. If you’ve had a biopsy and it was benign, you’ll typically get another ultrasound in 6-12 months to check for growth.
Are all thyroid nodules dangerous?
No. Over 90% of thyroid nodules are benign. Most people with nodules never need treatment. Ultrasound helps identify the small percentage that might be cancerous so they can be monitored or treated early.
Can I avoid a biopsy if my nodule looks suspicious?
Sometimes. If your nodule is small (under 1 cm) and has only mild suspicious features, your doctor may recommend observation instead of biopsy. If molecular testing is available and shows low-risk markers, surgery may be avoided. But if features are strongly suspicious, biopsy is still the standard.
What’s the cost of a thyroid ultrasound?
In the U.S., it typically costs between $200 and $500 without insurance. With insurance, your out-of-pocket cost may be $20-$100 depending on your plan. Costs vary by region and facility. Always ask for a price estimate beforehand.
Write a comment
Items marked with * are required.



12 Comments
Matthew Hekmatniaz December 31, 2025 AT 18:21
Really appreciate how clear this breakdown is. I had a nodule last year and was terrified until my radiologist walked me through TI-RADS. Turns out it was TR2-no biopsy, just a yearly check. Knowing the numbers helped me sleep at night.
Also, the part about lymph node checks? Huge. My first scan missed that entirely. Second clinic, accredited, caught it. Lesson learned: don’t skip the accreditation question.
Ultrasound isn’t perfect, but it’s the best tool we’ve got. Way better than guessing or jumping to radiation scans.
Liam George January 1, 2026 AT 05:29
Let me ask you something-how many of these 'standardized' TI-RADS scores were actually designed by radiology conglomerates with vested interests in biopsies and follow-up procedures?
They say 'evidence-based,' but the data comes from studies funded by ultrasound machine manufacturers. And don’t get me started on AI-trained on biased datasets, then sold back to hospitals as 'objective.'
Meanwhile, natural iodine protocols, selenium supplementation, and thyroid detox protocols have been shown in peer-reviewed studies to shrink nodules without surgery. But you won’t hear that from Big Med.
Wake up. The system doesn’t want you healthy. It wants you returning.
Bill Medley January 1, 2026 AT 22:51
Accurate, non-invasive, cost-effective. Ultrasound is the gold standard for initial thyroid nodule assessment. TI-RADS improves consistency. Biopsy remains diagnostic. AI enhances, does not replace, clinical judgment.
Richard Thomas January 2, 2026 AT 11:27
There’s something deeply human about this whole process, isn’t there? We’ve turned the body into a map of symbols-hypoechoic, microcalcifications, TI-RADS scores-as if the thyroid were a puzzle to be solved rather than a part of us that’s been whispering for attention.
People panic because they don’t understand the language. But the real fear isn’t the nodule. It’s the silence that follows a diagnosis. The waiting. The feeling that your body has betrayed you.
Ultrasound doesn’t just show tissue. It gives voice to the invisible. It says: ‘We see you. We’re not ignoring you.’ That’s why it matters more than the numbers.
And yet, we reduce it to risk percentages. We forget that behind every TR4 is someone who just wants to know if they’ll live to see their kid graduate.
Maybe the real breakthrough isn’t AI or better imaging. It’s learning how to sit with someone while they hold that uncertainty.
I’ve sat with people after scans. The silence after ‘It’s suspicious’ is louder than any Doppler signal.
Heather Josey January 3, 2026 AT 20:07
This is such an important and well-explained post. I’m a nurse who’s seen too many patients delay care because they thought ‘it’s probably nothing.’ But thyroid cancer is one of the few cancers where early detection literally changes survival outcomes.
And yes-ultrasound is painless. I’ve had one myself. The gel is cold, but that’s it. No needles, no anxiety, no downtime. Why would anyone skip it?
Also, the 99% 10-year survival rate with monitoring? That’s hope. And we need more of that in medicine.
Lee M January 4, 2026 AT 16:40
TI-RADS is just a fancy way of saying ‘trust the radiologist’-but half of them can’t even agree on what ‘irregular margin’ means. You think you’re getting precision? You’re getting guesswork dressed up in jargon.
And AI? It’s trained on data from elite hospitals. What about the rural clinic with a $10k machine and a tech who’s never seen a thyroid before?
We’re outsourcing diagnosis to algorithms built by people who’ve never held a patient’s hand.
Kristen Russell January 6, 2026 AT 00:35
Just had my first ultrasound last week-TR3, 1.8cm. Doctor said ‘let’s wait and watch.’ Felt so much better knowing I didn’t need to rush into a biopsy. Thanks for the clarity!
Bryan Anderson January 6, 2026 AT 15:02
Great summary. One thing I’d add: the emotional toll of waiting for follow-up scans is often underestimated. Many patients report anxiety spikes right before their ultrasound appointments-even if they’re low risk.
Having a clear timeline (e.g., ‘we’ll recheck in 12 months’) helps reduce that stress. Also, asking for a copy of the report and images can empower patients to track changes themselves over time.
Knowledge really is power here.
sharad vyas January 7, 2026 AT 02:47
in india we dont have much access to this kind of scan. many people only find out when the lump is huge. i had a friend who waited 3 years because he thought it was just a swollen gland. now he needs surgery. ultrasound should be available to everyone, not just rich people.
Dusty Weeks January 8, 2026 AT 01:27
bro i got a nodule last year and i was like ‘is this cancer??’ then i did a google search and found a guy on youtube who said it’s all from 5g and fluoride… i started drinking lemon water and taking iodine drops and now it’s gone 😎✌️
Sally Denham-Vaughan January 8, 2026 AT 03:35
My mom had a TR5 nodule last year. Biopsy came back benign. She’s still getting scans every 6 months. I was terrified-but this post made me realize how much we’ve improved. No one’s rushing to cut out thyroids anymore. That’s progress.
Also, the Doppler sound? So weird. Like a spaceship in a movie. My mom said it made her laugh. Who knew a medical scan could be kinda cool?
Paul Ong January 8, 2026 AT 16:31
Ultrasound is the gatekeeper. Biopsy is the verdict. AI is the assistant. Don't overcomplicate it. If your doc says watch it then watch it. If they say biopsy then get it done. Trust the process. Your thyroid isn't your enemy. It's just doing its job. You just gotta listen.