Health February 1, 2026
Dual Antiplatelet Therapy: Managing Bleeding Side Effects
DAPT Bleeding Risk Calculator
PRECISE-DAPT Bleeding Risk Score Calculator
The PRECISE-DAPT score helps identify patients at high risk of bleeding during dual antiplatelet therapy after heart stent placement. A score of 25 or higher indicates high bleeding risk.
When you’ve had a heart stent placed, doctors prescribe dual antiplatelet therapy - usually aspirin plus another drug like clopidogrel, prasugrel, or ticagrelor - to keep your arteries open. It works. Studies show it cuts the chance of another heart attack or stent clotting by up to 30%. But here’s the catch: every time you take these drugs, you’re also making yourself more likely to bleed. Not just a little. Enough to matter.
Why DAPT Works - and Why It Bleeds
Your blood has tiny platelets that clump together when you get hurt. That’s good - it stops cuts from bleeding too long. But when plaque builds up in your arteries, those same platelets can stick where they shouldn’t, forming clots that cause heart attacks. DAPT blocks those platelets from sticking together. Aspirin does one thing. The P2Y12 inhibitor - clopidogrel, prasugrel, or ticagrelor - does another. Together, they’re stronger than either alone.
But your body doesn’t know the difference between a dangerous clot in your artery and a simple cut on your finger. So when you’re on DAPT, even minor injuries can lead to longer bleeding. Nosebleeds that won’t stop. Bruises that spread. Blood in your stool. These aren’t rare. In fact, about 1 in 50 people on DAPT will have a major bleed within a year. That’s not a small risk. It’s a real trade-off.
The Three Drugs - And Their Bleeding Trade-Offs
Not all DAPT combinations are the same. The choice of P2Y12 inhibitor changes everything.
- Clopidogrel is the oldest. It’s cheaper. It causes fewer bleeds - about 30-40% less than the newer drugs. But it’s also weaker. About 1 in 10 people don’t respond well to it, leaving them at higher risk for clots.
- Prasugrel works faster and stronger. Great for people who’ve just had a heart attack. But it increases major bleeding by 20% compared to clopidogrel. It’s not even recommended for patients over 75 or under 60 kg.
- Ticagrelor is the most potent. It reduces heart attacks better than clopidogrel. But it also causes more bleeding - 27% more, according to one trial. It can also cause shortness of breath and slower heart rate. And here’s the kicker: there’s no antidote. If you bleed badly, you can’t just reverse it like you can with some blood thinners.
That’s why doctors don’t just pick one at random. They look at your age, your history of bleeding, your kidney function, and whether you’re on other medicines. A 72-year-old with a past stomach bleed? Clopidogrel might be safer. A 58-year-old with a recent heart attack and no bleeding history? Ticagrelor could save their life.
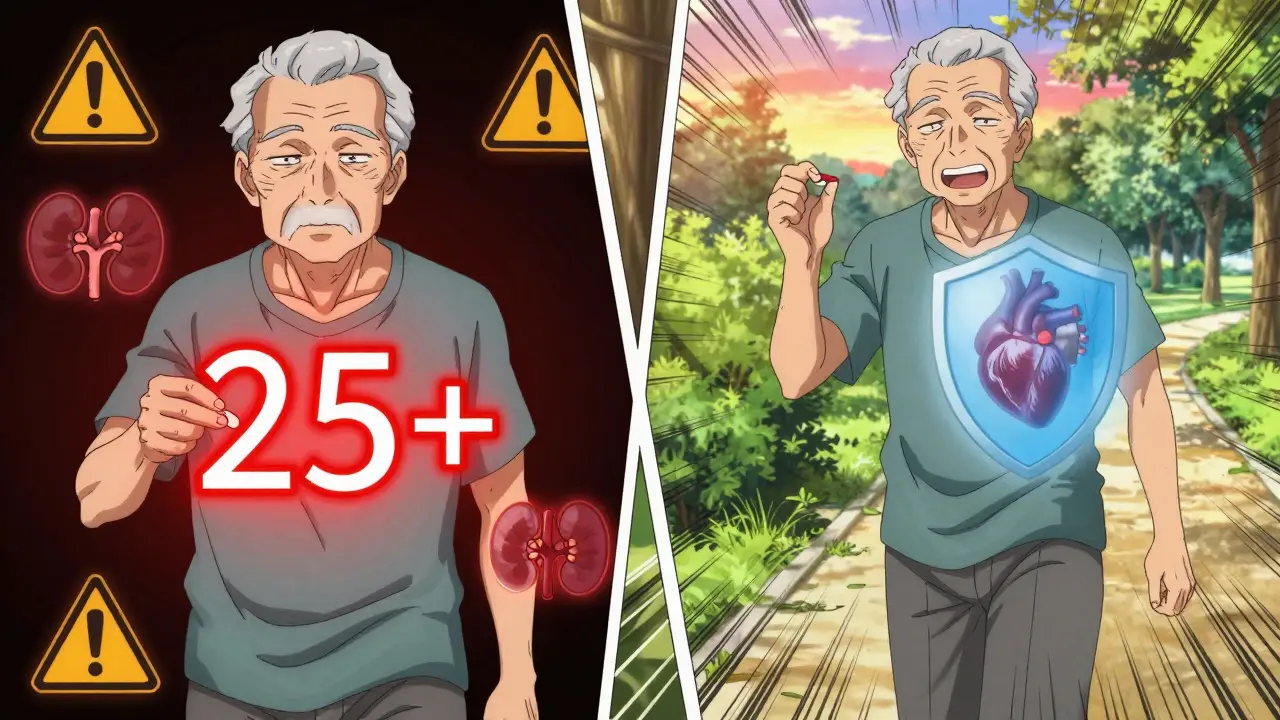
Who’s at Highest Risk for Bleeding?
Not everyone on DAPT needs the same plan. Some people are at high bleeding risk - and we now have a way to spot them before they start.
The PRECISE-DAPT score is used in hospitals across the UK and US. It adds up points for things like:
- Age over 75
- Low hemoglobin (anemia)
- Low kidney function
- History of bleeding
- Low platelet count
- Taking blood thinners like warfarin
If your score is 25 or higher, you’re in the high-risk group. That’s about 1 in 4 patients after stent placement. For these people, sticking to 12 months of DAPT might do more harm than good.
That’s why newer guidelines now say: for high-risk patients, shorten the time. One month of DAPT, then switch to just aspirin. The MASTER DAPT trial showed this cut major bleeding by nearly 7% over two years - with no rise in heart attacks or deaths.
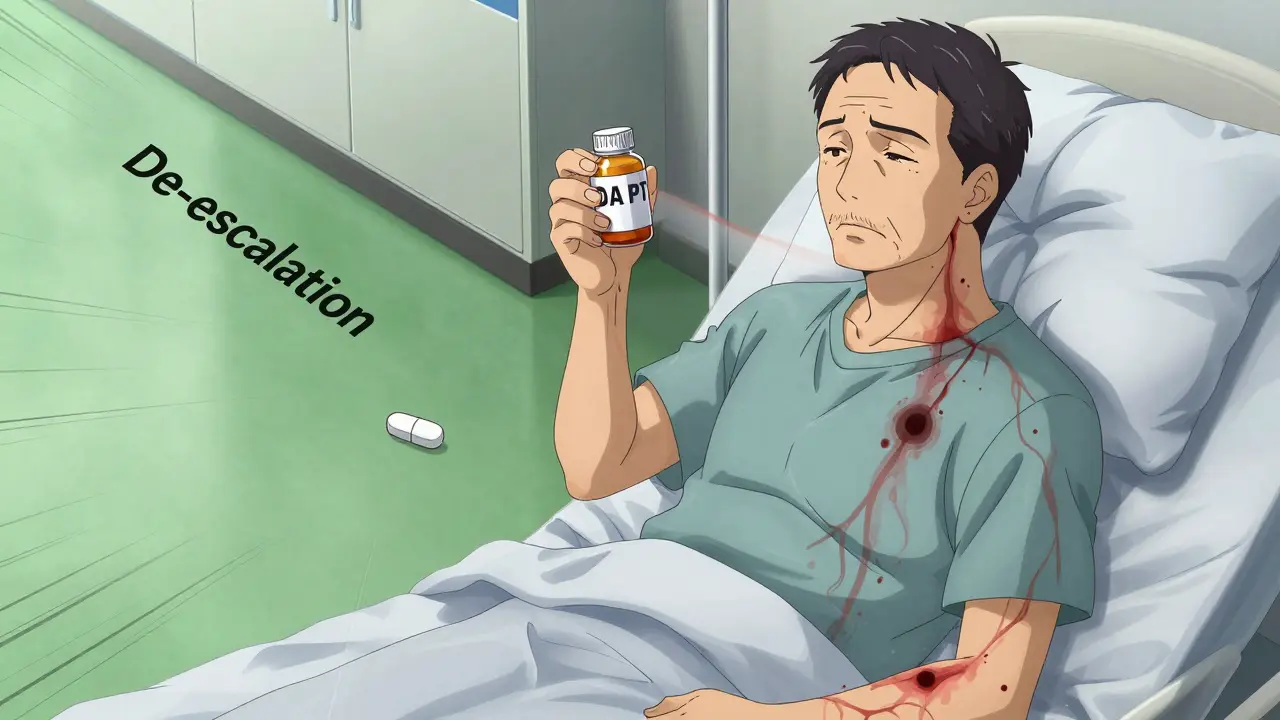
De-Escalation: The Smart Middle Ground
What if you’re on ticagrelor or prasugrel - the strong ones - but you’re starting to bleed? You don’t have to stop DAPT completely. You can switch.
This is called de-escalation. After 1 to 3 months, you stop the potent drug and switch to clopidogrel. The TALOS-AMI trial tracked over 2,500 heart attack patients. Those who switched from ticagrelor to clopidogrel after one month had 2.1% fewer major bleeds - and the same number of heart attacks.
And here’s what patients said: they felt better. Less anxious. More willing to take their pills. When you stop worrying about every nosebleed or bruise, you stick with the treatment. That’s huge. In that same study, patients with minor bleeding were 32% more likely to quit their meds. De-escalation fixes that.
What to Do If You Start Bleeding
Not every bleed means you need to stop DAPT. But you need to know when to call your doctor.
- Nosebleeds that last more than 15 minutes? Call.
- Bleeding gums when brushing? Not urgent - but mention it at your next visit.
- Dark, tarry stools or bright red blood in stool? Go to the ER. That’s internal bleeding.
- Head injury while on DAPT? Get checked. Even a small bump can cause a bleed inside the skull.
- Heavy menstrual bleeding? Talk to your doctor. You might need a different approach.
And here’s something many don’t know: you don’t need to stop DAPT for minor procedures. Dental cleaning? Colonoscopy? Even a lumbar puncture? Most of the time, you can keep taking your pills. The risk of bleeding from these is low. Stopping DAPT for them can be riskier than the procedure itself.
The Human Side: Anxiety, Avoidance, and Adherence
Bleeding isn’t just a medical event. It’s a life event.
Patients on DAPT who had even minor bleeding - like a nosebleed that didn’t need treatment - reported being afraid to exercise, to travel, to hug their grandkids. One woman in a Reddit thread said she stopped hugging her grandchildren because she didn’t want to risk bruising them. Another said he avoided shaving because he didn’t want to nick himself.
That fear leads to stopping the meds. And stopping DAPT too early? That’s dangerous. If you stop before 6 months after a stent, your risk of a deadly clot jumps 2 to 3 times. That’s why doctors now focus on managing bleeding - not just avoiding it.
Patients who switched to clopidogrel after 1 month reported a 15-point improvement in quality-of-life scores. That’s not just a number. It’s sleeping through the night. Not checking the toilet every time you pee. Feeling like yourself again.
What’s Next? The Future of DAPT
Doctors aren’t waiting around. The NIH is funding a new registry tracking 15,000 patients to predict bleeding risk using AI. The European Society of Cardiology is pushing for specific antidotes - something to reverse ticagrelor’s effects fast. Right now, if you bleed badly, you’re stuck waiting for the drug to wear off. That can take days.
By 2028, experts believe most patients will get personalized DAPT plans. Not 6 months. Not 12. But exactly what your body needs. Some might get 1 month. Others, 3. A few, maybe 24. It won’t be one-size-fits-all anymore.
And that’s the goal: protect your heart - without making you afraid to live.
Can I stop dual antiplatelet therapy on my own if I’m bleeding?
No. Stopping DAPT without medical advice, especially within the first 6 months after a stent, can cause a life-threatening clot. If you’re bleeding, contact your doctor immediately. They’ll assess whether to pause, reduce, or switch your medication - never stop on your own.
Is clopidogrel less effective than ticagrelor?
Yes - but only for some people. Ticagrelor is more powerful at preventing heart attacks and stent clots. But for patients at high risk of bleeding, older drugs like clopidogrel offer a better balance. Many patients start with ticagrelor and switch to clopidogrel after 1-3 months to reduce bleeding without losing protection.
Do I need to stop DAPT before dental work?
Almost always, no. Routine dental cleanings, fillings, and even tooth extractions can be done safely while on DAPT. Stopping increases clot risk more than the bleeding risk from the procedure. Always tell your dentist you’re on dual therapy - they’ll take extra precautions.
How do I know if I’m at high bleeding risk?
Your doctor uses the PRECISE-DAPT score, which looks at your age, kidney function, hemoglobin levels, history of bleeding, and whether you’re on other blood thinners. A score of 25 or higher means you’re high risk. If you’re unsure, ask your cardiologist to calculate your score after your stent procedure.
Are there any natural remedies to reduce bleeding on DAPT?
No. Supplements like fish oil, garlic, ginger, or ginkgo can make bleeding worse. Avoid them while on DAPT. There’s no proven natural way to reduce bleeding risk. The only proven methods are medical: adjusting your drug, switching to clopidogrel, or shortening treatment duration - all under doctor supervision.
What happens if I miss a dose of my antiplatelet drug?
If you miss one dose, take it as soon as you remember - unless it’s almost time for your next one. Never double up. Missing doses increases your clot risk, especially in the first 3 months after a stent. If you miss more than two doses in a row, contact your doctor immediately.
Bottom Line: Balance, Not Fear
Dual antiplatelet therapy saves lives. But it doesn’t come without cost. The goal isn’t to avoid bleeding at all costs - it’s to manage it smartly. That means knowing your risk. Talking openly with your doctor. And not being afraid to ask: “Is there a safer way for me?”
There is. And more options are coming. For now, the best strategy is personalized, not prolonged. Shorter. Smarter. Safer. That’s the new standard - and it’s already working for thousands of people right now.
Write a comment
Items marked with * are required.



8 Comments
Vatsal Srivastava February 1, 2026 AT 16:25
Interesting how they frame this as a "trade-off" like it's some noble sacrifice. Meanwhile, in the real world, 1 in 50 bleeding events is just poor pharmacological design. Why not develop targeted platelet inhibitors instead of blunt-force trauma to the entire hemostatic system? We've had 20 years of this. Pathetic.
Dan Pearson February 3, 2026 AT 14:30
LMAO you guys are crying about nosebleeds? In my day, we didn't have fancy pills. We had aspirin and grit. If you bled, you held pressure. If you died, you died. This whole "personalized DAPT" nonsense is just Big Pharma selling you anxiety so you'll keep buying their $400/month drugs. America, wake up.
jay patel February 4, 2026 AT 07:24
bro i just had a stent last year and honestly the worst part wasnt the bleeding it was the fear. like i stopped hugging my niece because i thought i'd bruise her and then she started crying and i felt like a monster. then i switched to clopidogrel after 6 weeks and suddenly i could sleep again. no more checking the toilet every time i pee. i swear to god this isnt just medical data its human stuff. also typo sorry im typing on my phone at 3am
Ansley Mayson February 5, 2026 AT 17:39
They mention the PRECISE-DAPT score like it's gospel. Meanwhile, most primary care docs don't even know what it is. And the trials? All funded by pharma. Of course they found "de-escalation" works. It's cheaper than lifelong ticagrelor. This isn't medicine. It's cost containment dressed in white coats.
phara don February 6, 2026 AT 17:34
Anyone else notice ticagrelor makes you feel like you're breathing through a straw? 😅 I thought I was having a panic attack until my cardiologist said "that's the drug". Switched to clopidogrel. Breathing again. Also no more random bruising on my arms. 🤞
Hannah Gliane February 7, 2026 AT 06:38
So you're telling me people are too scared to hug their grandkids because of a drug? 🤦♀️ Next they'll ban exercise and sunlight. People need to stop being babies. If you're bleeding from a nosebleed, you're either on too much or you're just a hypochondriac. Also, why are you taking ginger? That's literally asking for trouble. 😒
Murarikar Satishwar February 8, 2026 AT 02:01
De-escalation is the real win here. Not because it's new, but because it's patient-centered. Switching from ticagrelor to clopidogrel after 30 days isn't a compromise-it's precision medicine in action. The TALOS-AMI trial data is solid: fewer bleeds, same cardiac protection, and patients actually feel like they can live again. This isn't just clinical-it's psychological liberation. And yes, dental work? Keep taking it. Your dentist can manage minor bleeding. Stopping DAPT for a cleaning is like turning off your car's airbag because you got a scratch.
Bob Hynes February 8, 2026 AT 08:06
As a Canadian who’s seen this play out in both public and private systems… the real story isn’t the drugs, it’s the fear. People are terrified to live because they’re told every bruise is a death sentence. We need more education, not just more algorithms. And hey-can we please stop calling it "DAPT"? Sounds like a secret government program. Just say "the two blood thinners". It’s less scary. 🇨🇦