Health October 19, 2025
How Hydrochlorothiazide Lowers Blood Pressure - The Science Explained
Blood Pressure Reduction Calculator
How Hydrochlorothiazide Lowers Blood Pressure
This calculator estimates your potential blood pressure reduction based on the article's research showing an average systolic reduction of 9 mmHg and diastolic reduction of 5 mmHg. The effect depends on sodium intake, potassium balance, and treatment duration.
When you take Hydrochlorothiazide a thiazide diuretic that lowers blood pressure by promoting sodium and water loss, you’re stepping into a cascade of kidney‑driven changes that ultimately calm an over‑active cardiovascular system. This article breaks down the chemistry, the kidney’s role, and the downstream effects on the heart, giving you a clear picture of why this old‑school pill remains a cornerstone of hypertension treatment.
What makes Hydrochlorothiazide a thiazide diuretic?
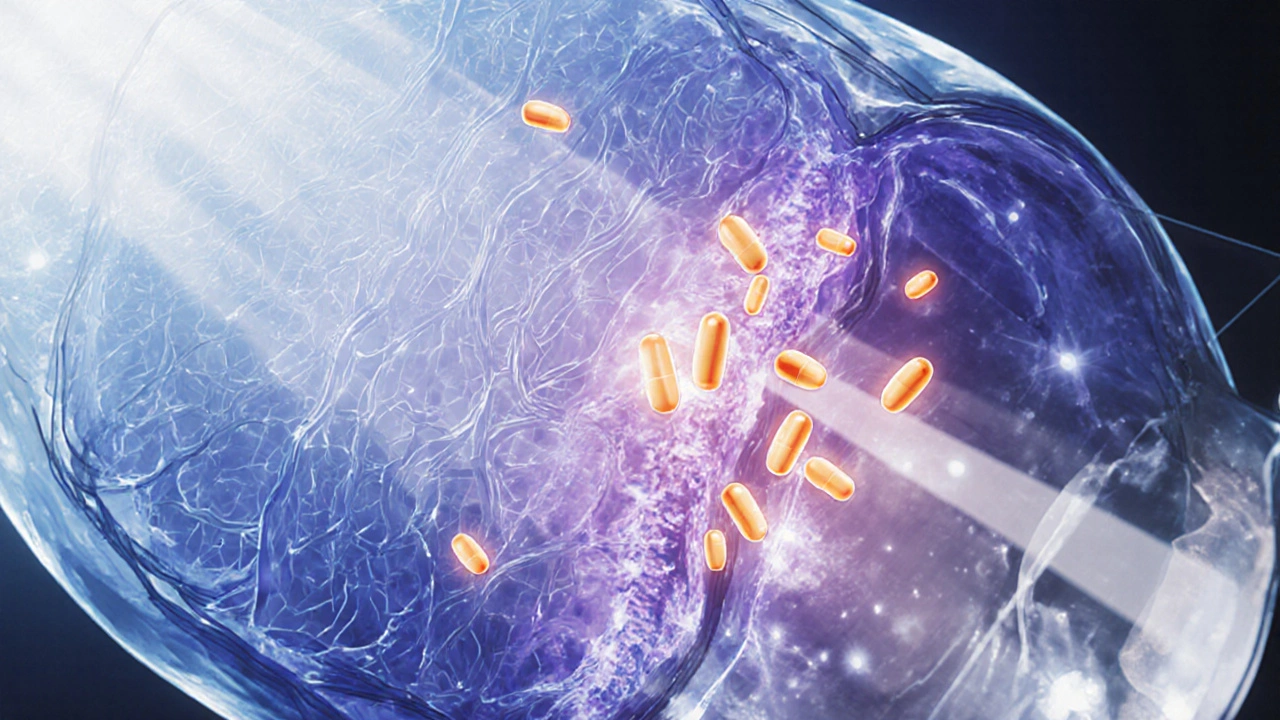
Thiazide diuretics belong to a family of drugs that act on the distal convoluted tubule (DCT) of the nephron. The DCT is the segment where the body fine‑tunes electrolyte balance before urine leaves the kidney. Thiazide diuretics inhibit the Na⁺/Cl⁻ co‑transporter (NCC) located on the apical membrane of DCT cells. By blocking NCC, Hydrochlorothiazide reduces the reabsorption of sodium (Na⁺) and chloride (Cl⁻), forcing the kidney to excrete more of both along with water.
Pharmacokinetics: How the drug gets to the kidney
After oral ingestion, Hydrochlorothiazide is absorbed quickly, reaching peak plasma concentrations in about 2 hours. It binds to plasma proteins at roughly 40 % and is largely excreted unchanged via the kidneys, with a half‑life of 6‑15 hours. This relatively long half‑life means a single daily dose maintains enough plasma level to keep the NCC blocked throughout the day.
Why sodium loss matters for blood pressure
Sodium is a key driver of extracellular fluid volume. When the body retains more Na⁺, water follows osmotically, expanding blood volume. More volume means the heart must pump a larger amount of fluid with each beat, raising arterial pressure. By flushing Na⁺ out, Hydrochlorothiazide shrinks plasma volume, which directly drops the pressure against which the heart works.
Influence on the Renin‑Angiotensin‑Aldosterone System (RAAS)
The RAAS acts like a thermostat for blood pressure. Low blood volume triggers the kidneys to release renin, starting a chain that creates angiotensin II, a powerful vasoconstrictor, and aldosterone, which forces the kidneys to retain sodium. Hydrochlorothiazide’s volume‑reducing effect initially nudges renin up, but chronic use leads to a new equilibrium: the body adapts, and the overall vasoconstrictive tone diminishes. This adaptation is why thiazides are especially effective when combined with ACE inhibitors or ARBs - the two mechanisms complement each other without over‑activating the RAAS.
Direct vascular effects beyond volume reduction
Research from 2023 shows that thiazides open potassium channels in vascular smooth muscle, causing mild relaxation of arterial walls independent of volume changes. This vasodilatory action adds a second layer of blood‑pressure lowering, especially valuable in patients whose blood pressure remains high despite adequate diuresis.
Clinical impact: What the numbers say
Large meta‑analyses covering more than 150,000 hypertensive patients report an average systolic reduction of 9 mm Hg and diastolic reduction of 5 mm Hg after 8‑weeks of Hydrochlorothiazide therapy. The effect is consistent across age groups, though older adults tend to see slightly larger drops, likely because their kidneys are more prone to sodium retention.

Common side effects and safety considerations
- Electrolyte shifts: Loss of Na⁺ often comes with potassium (K⁺) loss, risking hypokalemia. Routine labs every 3‑4 months help catch this early.
- Increased uric acid: Thiazides reduce uric acid excretion, which can provoke gout attacks in susceptible individuals.
- Elevated glucose: Small rises in blood sugar have been noted, especially in patients with pre‑diabetes.
- Photosensitivity: Some users develop skin reactions to sunlight; sunscreen and protective clothing are advised.
Most side effects are manageable with lifestyle tweaks or complementary meds (e.g., potassium‑sparing diuretics). Severe reactions are rare, but any sign of muscle weakness, irregular heartbeat, or severe dizziness warrants immediate medical attention.
Practical tips for patients on Hydrochlorothiazide
- Take the pill in the morning to avoid nighttime bathroom trips.
- Pair with a potassium‑rich diet (bananas, oranges, leafy greens) or a low‑dose potassium supplement if labs show low K⁺.
- Stay hydrated, but avoid excessive fluid intake that could blunt the drug’s effect.
- Monitor blood pressure at the same time each day; look for a steady downward trend over weeks, not day‑to‑day spikes.
- Schedule periodic blood tests for electrolytes, kidney function (creatinine, eGFR), and uric acid.
Frequently Asked Questions
How quickly does Hydrochlorothiazide start lowering blood pressure?
Most patients notice a modest drop within 2‑3 days, with the full effect appearing after about 2 weeks of consistent dosing.
Can I take Hydrochlorothiazide with other blood‑pressure medicines?
Yes. It’s commonly combined with ACE inhibitors, ARBs, or calcium‑channel blockers to target different pathways and achieve better control.
Why do I need to check my potassium levels?
Hydrochlorothiazide promotes potassium loss alongside sodium. Low potassium can cause muscle cramps, irregular heartbeats, and fatigue.
Is Hydrochlorothiazide safe for people with kidney disease?
It can be used in mild to moderate chronic kidney disease, but dosage may need adjustment and kidney function must be monitored regularly.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s near the time of your next dose. In that case, skip the missed pill and continue with your regular schedule. Don’t double up.
Understanding the science behind Hydrochlorothiazide helps demystify why a simple pill can make a big difference in managing hypertension. By targeting sodium reabsorption, tweaking the RAAS, and gently relaxing blood vessels, the drug delivers a multi‑pronged attack on high blood pressure while keeping side effects manageable for most patients.
Write a comment
Items marked with * are required.




15 Comments
Penny Reeves October 19, 2025 AT 20:53
Hydrochlorothiazide reduces sodium reabsorption in the distal tubule, prompting a modest diuretic effect.
Monika Bozkurt October 20, 2025 AT 10:46
The inhibition of the Na⁺/Cl⁻ cotransporter in the distal convoluted tubule creates a cascade of physiologic adjustments.
By decreasing sodium reabsorption, the extracellular fluid volume contracts, which directly lowers cardiac output.
The resulting decline in renal perfusion stimulates renin release, yet chronic thiazide therapy leads to a new steady state where vasoconstrictive drive is attenuated.
Moreover, thiazides have been shown to modestly open potassium channels in vascular smooth muscle, adding a vasodilatory component independent of volume depletion.
These mechanisms together explain the consistent modest reductions in systolic and diastolic pressures observed across large trials.
Clinicians therefore consider hydrochlorothiazide a cornerstone of step‑wise hypertension management.
sravya rudraraju October 21, 2025 AT 00:40
The pharmacologic profile of hydrochlorothiazide extends far beyond a simplistic diuretic label.
When the drug binds to the apical membrane of distal tubule cells, it sterically hinders the Na⁺/Cl⁻ symporter, forcing the nephron to excrete excess sodium alongside water.
This primary natriuretic effect initiates a reduction in plasma volume, which in turn decreases preload and peripheral resistance.
A lower preload translates into less stretch of the ventricular walls, thereby diminishing the stimulus for maladaptive hypertrophy.
Concurrently, the diminished intravascular volume prompts a compensatory rise in renin secretion, but chronic exposure to thiazides blunts the downstream angiotensin II surge through receptor down‑regulation.
The net effect is a recalibrated renin‑angiotensin‑aldosterone axis that favors vasodilation rather than vasoconstriction.
Recent mechanistic studies have identified that thiazide molecules can directly activate endothelial potassium channels, leading to hyperpolarization of smooth muscle cells and gentle arterial relaxation.
This vasodilatory pathway operates independently of volume status, providing an additive blood‑pressure‑lowering benefit in patients who maintain euvolemia.
From a clinical perspective, the synergistic action of volume depletion and direct vascular relaxation accounts for the average 9 mm Hg systolic drop reported in meta‑analyses.
Older patients often experience a slightly larger effect because age‑related renal sodium handling becomes less efficient, magnifying the diuretic impact.
Nevertheless, clinicians must vigilantly monitor electrolyte balance, as the concomitant loss of potassium can precipitate arrhythmogenic risks.
Routine laboratory assessment every three to four months is a pragmatic strategy to catch hypokalemia before symptomatic manifestations arise.
In patients with a predisposition to hyperuricemia, the drug’s effect on uric acid excretion warrants consideration of prophylactic allopurinol or dietary modification.
Lifestyle measures, such as dietary potassium enrichment through fruits and vegetables, complement pharmacotherapy and may reduce the need for supplemental potassium salts.
Adherence to a morning dosing schedule mitigates nocturnal diuresis and enhances patient tolerance of the regimen.
Overall, hydrochlorothiazide exemplifies a multifaceted therapeutic agent that leverages renal physiology, hormonal modulation, and direct vascular effects to achieve durable blood‑pressure control.
Future research may uncover additional molecular targets that could further refine its risk‑benefit profile.
Ben Bathgate October 21, 2025 AT 14:33
Honestly, the hype around hydrochlorothiazide often overshadows its blunt side‑effects.
While the drug does drop pressure, the potassium loss can be a silent killer for unsuspecting patients.
The literature glosses over how many people end up on supplemental potassium, adding cost and compliance headaches.
Bottom line, the pill works, but it’s not the miracle you think it is.
Ankitpgujjar Poswal October 22, 2025 AT 04:26
Listen up, if you’re still battling stubborn numbers, crank up your adherence and pair the thiazide with a potassium‑rich diet.
The synergy between diet and drug can shave off those extra millimeters you’re fighting for.
Don’t let minor side‑effects derail your long‑term plan; manage them and stay the course.
Bobby Marie October 22, 2025 AT 18:20
Just keep an eye on your labs; it saves headaches later.
Thokchom Imosana October 23, 2025 AT 08:13
Big Pharma pushes hydrochlorothiazide as a cheap fix while quietly funneling research dollars into newer, pricier combos that line their pockets.
The subtle shift in prescribing trends isn’t accidental; it reflects a calculated move to keep the market captive.
Remember, the same companies that own the generic manufacturers also fund the guideline committees.
ashanti barrett October 23, 2025 AT 22:06
It’s easy to feel overwhelmed by the electrolyte dance, but consistent monitoring transforms uncertainty into confidence.
By checking potassium and uric acid regularly, you stay ahead of the curve and avoid nasty surprises.
This proactive stance empowers you to keep blood pressure low without sacrificing quality of life.
jagdish soni October 24, 2025 AT 12:00
One must appreciate the elegance of targeting a single transporter to orchestrate systemic hemodynamic changes.
The distal convoluted tubule, often overlooked, becomes the hero in this pharmacologic saga.
It’s a reminder that simplicity can yield profound therapeutic outcomes.
Latasha Becker October 25, 2025 AT 01:53
Contrary to popular belief, the magnitude of systolic reduction is not solely a function of volume depletion; intrinsic vascular remodeling plays a pivotal role.
Meta‑analytical sub‑group analyses reveal that patients with baseline arterial stiffness derive disproportionate benefit, underscoring the drug’s pleiotropic nature.
Therefore, dismissing hydrochlorothiazide as a mere diuretic neglects its nuanced mechanistic profile.
Maridel Frey October 25, 2025 AT 15:46
From a holistic perspective, integrating lifestyle modifications with hydrochlorothiazide enhances therapeutic durability.
Encouraging patients to adopt low‑salt meals, regular exercise, and stress‑reduction techniques complements the pharmacologic effects and fosters long‑term adherence.
This comprehensive approach aligns with best practice guidelines.
Madhav Dasari October 26, 2025 AT 04:40
Yo, the numbers don’t lie-when you slap that thiazide on a stubborn case, the pressure drops like a mic drop at a rap battle!
But don’t just ride the high; keep the potassium in check or you’ll end up with a shaky heart that’s no joke.
Stay vigilant, stay pumped, and let the meds do the heavy lifting while you bring the swagger.
DHARMENDER BHATHAVAR October 26, 2025 AT 18:33
Monitoring renal function alongside electrolyte panels ensures safe long‑term hydrochlorothiazide therapy.
Kevin Sheehan October 27, 2025 AT 08:26
The pursuit of optimal blood pressure mirrors the quest for equilibrium in life; combining agents that act on distinct pathways mirrors a balanced philosophy.
Aggressive titration, when guided by data, reflects disciplined ambition rather than reckless bravado.
Embrace the synergy, respect the limits, and you will find harmony in cardiovascular health.
Jameson The Owl October 27, 2025 AT 22:20
Consider the timeline of approvals and you see a pattern of regulatory capture that favors inexpensive diuretics over innovative solutions the public truly needs the same pill gets repackaged across continents while newer agents are buried under bureaucratic red tape the narrative of safety is curated by committees whose members owe allegiance to industry insiders this orchestrated silence on long term metabolic consequences is not an accident it is a strategic move to keep healthcare costs predictable for insurers and profitable for manufacturers the truth is buried beneath layers of jargon and selective data release and only a vigilant few dare to question the status quo.