Health December 5, 2025
Warfarin and Vitamin K: How to Maintain Consistent Diet for Stable INR Levels
Vitamin K Intake Calculator
Daily Vitamin K Tracker
Track your vitamin K intake to stay within the recommended range of 60-120 µg/day for stable INR levels
Current Day
Weekly Pattern
Track consistency over multiple days
| Day | Total (µg) | Status |
|---|---|---|
| Today | 0 µg | Within target |
| Yesterday | -- | -- |
| 2 days ago | -- | -- |
| 3 days ago | -- | -- |
Key Guidelines
Your goal is consistent intake between 60-120 µg daily
- Aim for 60-120 µg/day of vitamin K
- Choose consistent sources: e.g., ½ cup broccoli daily
- Avoid large spikes: Don't eat 1 cup of kale one day and none the next
- Track for 4-6 weeks to establish your baseline
- Never restrict vitamin K - it's essential for bone health
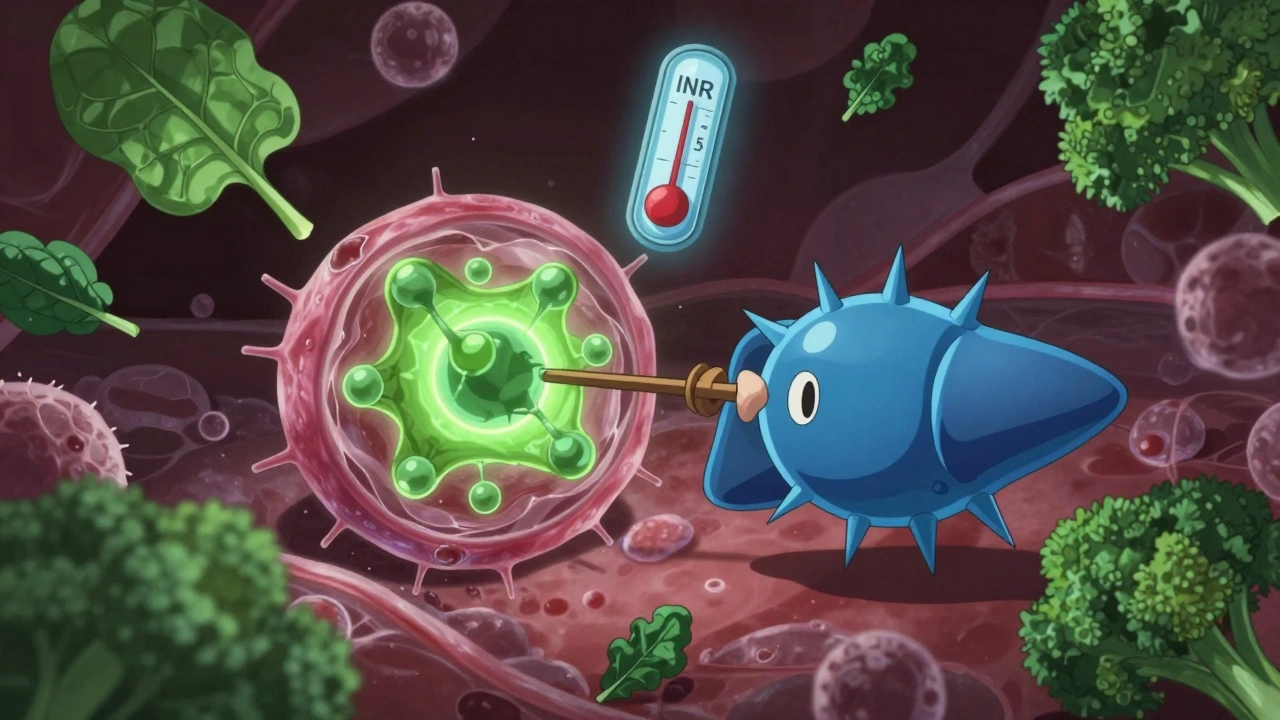
When you're on warfarin, your life doesn't stop-but the way you eat might need to change. Not because you have to give up your favorite greens, but because warfarin and vitamin K are locked in a quiet biochemical tug-of-war inside your body. Get the balance wrong, and your INR can swing wildly. Too high, and you risk bleeding. Too low, and you could clot. The good news? You don't need to avoid vitamin K. You just need to keep it steady.
Why Warfarin and Vitamin K Are a Team of Opposites
Warfarin works by blocking a key enzyme called VKORC1. This enzyme normally recycles vitamin K so your body can use it to activate clotting factors-proteins that help your blood form clots when needed. Without enough active vitamin K, those clotting factors stay inactive. That’s the whole point: to thin your blood and prevent dangerous clots from forming in your heart, lungs, or legs. But here’s the catch: vitamin K doesn’t just disappear when you take warfarin. It’s still in your food. Spinach, kale, broccoli, Brussels sprouts, even some oils and meats contain it. Every time you eat vitamin K, it fights back against warfarin’s effect. One big serving of kale can temporarily overpower your dose. That’s why your INR (International Normalized Ratio) jumps up and down. Your INR is the number your doctor checks every few weeks. For most people, the target is between 2.0 and 3.0. If you have a mechanical heart valve, it might be higher-2.5 to 3.5. When your INR stays in that range, you’re protected. When it drifts outside, you’re at risk.What Happens When You Eat Too Much-or Too Little-Vitamin K
A 2019 study in Thrombosis and Haemostasis found that people with inconsistent vitamin K intake were 2.3 times more likely to have INR levels outside the safe range. That’s not a small risk. It means more blood tests, more doctor visits, and potentially emergency trips to the hospital. Here’s the twist: it’s not about cutting out vitamin K. It’s about consistency. The National Academies say women need 90 micrograms (µg) of vitamin K per day and men need 120 µg. But most Americans already hit that mark-without even trying. The problem isn’t deficiency. It’s fluctuation. Some people think, “If vitamin K makes warfarin less effective, I’ll just stop eating greens.” But that backfires. A 2020 American Heart Association statement warns that vitamin K restriction actually increases INR instability. Why? Because your body starts to crave it. When you suddenly eat it again-even a small amount-it hits hard. Your INR crashes. You’re more likely to clot. Worse, long-term low vitamin K intake can weaken your bones. Vitamin K isn’t just about blood. It helps keep calcium where it belongs-in your bones, not your arteries. Restricting it for months or years can lead to osteoporosis. That’s why experts now say: don’t restrict. Just stabilize.The Magic Number: 60-120 µg Per Day
The Anticoagulation Forum recommends aiming for 60 to 120 micrograms of vitamin K daily. That’s not a strict limit. It’s a target range. You can eat more than that-just make sure you eat about the same amount every day. Here’s what that looks like in real meals:- 1 cup cooked spinach: 889 µg (way too much for one day)
- 1 cup raw kale: 547 µg
- ½ cup cooked broccoli: 102 µg
- 1 scrambled egg: 20 µg
- 3 oz chicken breast: 2 µg
- 1 tablespoon olive oil: 10 µg
Real People, Real Results
Reddit user u/WarfarinWarrior shared how their life changed after their pharmacist gave them a simple tracking sheet. They started eating exactly one cup of mixed greens every Tuesday and Thursday. No more guessing. No more panic when their INR spiked. Within weeks, their TTR jumped from 45% to 78%. That’s not magic. That’s math. Another survey of nearly 2,000 patients by the National Blood Clot Alliance found that 57% of emergency visits tied to INR instability were linked to inconsistent diet. People thought they were being careful by avoiding spinach. But then they ate a salad at a restaurant, or a friend brought over a kale smoothie, and their INR dropped. They didn’t know why. They just knew they felt dizzy or had bruising. At the Mayo Clinic, patients who got personalized counseling from anticoagulation pharmacists reached 82% TTR. Those who didn’t? Only 63%. The difference? Education. Structure. A plan.How to Build Your Own Vitamin K Routine
You don’t need to become a nutritionist. But you do need a system.- Track for 4-6 weeks. Use a food diary or an app like Warframate. Log everything you eat, especially leafy greens, cruciferous veggies, and oils. Don’t guess. Use measuring cups.
- Find your average. After a month, add up your daily vitamin K intake and divide by 30. That’s your baseline. If it’s 80 µg/day, aim to stay within 60-100 µg.
- Choose one or two consistent sources. Pick one or two foods you like and eat them regularly. Maybe it’s broccoli every Tuesday and Thursday. Or a spinach smoothie on Mondays and Fridays. Stick to it.
- Avoid big spikes. Don’t eat a whole bag of kale on Sunday and nothing else all week. Spread it out. Even 1 cup of raw kale every other day is better than 2 cups once a week.
- Check labels on supplements. Many multivitamins contain vitamin K. If you take one, tell your doctor. If you don’t, don’t start.
What About Genetics? Does My DNA Matter?
Yes, it does. About 30% of people have genetic variations in VKORC1 or CYP2C9 that make them more sensitive to vitamin K. If you’re one of them, even small changes in your diet can throw off your INR. A 2023 study in the Pharmacogenomics Journal showed that people with these variants needed tighter control-±10% variation in vitamin K intake-compared to ±25% for others. But here’s the thing: you don’t need a DNA test to know if you’re sensitive. If your INR swings every time you eat something green, you’re probably one of them. Talk to your pharmacist. Ask if they can help you find your personal sweet spot.What You Should Never Do
- Don’t cut out green vegetables. They’re packed with fiber, antioxidants, and nutrients. You need them.
- Don’t start taking vitamin K supplements without talking to your provider. Even 150 µg/day can change your dose.
- Don’t skip blood tests. Your INR doesn’t lie. If you feel fine, that doesn’t mean your blood is safe.
- Don’t trust vague advice. “Just eat less spinach” isn’t enough. You need numbers, not guesses.
Tools That Actually Help
- Warframate (iOS/Android): A food database with vitamin K values for over 1,200 items. Scans barcodes, tracks weekly trends. - USDA FoodData Central: Free online database. Search any food, get exact vitamin K content. - Meal templates: Many anticoagulation clinics give you a sample week: Monday = broccoli, Wednesday = egg and olive oil, Friday = salad with 1 cup mixed greens. - Measuring cups: Visual estimates are wrong 45% of the time. A cup of chopped spinach isn’t what you think it is. Measure it.Final Thought: Predictability Over Perfection
You don’t have to eat the same exact meal every day. You don’t have to be perfect. You just have to be predictable. Think of it like driving a car. You don’t need to go exactly 60 mph every second. But if you’re going 30 one minute and 90 the next, you’re going to crash. Your body is the same. Warfarin works best when your vitamin K intake is steady. Not low. Not high. Just consistent. The goal isn’t to live on plain rice and chicken. It’s to enjoy your food-knowing it won’t send you to the hospital.Can I still eat spinach if I’m on warfarin?
Yes, you can-and you should. The key is consistency. Eat about the same amount of spinach or other vitamin K-rich foods every day. A cup of cooked spinach has nearly 900 µg of vitamin K, so eating it daily means you’re likely getting more than enough. But if you eat it one day and skip it for a week, your INR will swing. Stick to a routine.
Does alcohol affect warfarin and vitamin K?
Yes. Heavy drinking can increase your INR and raise bleeding risk. Even moderate drinking can interfere with how your liver processes warfarin. If you drink, keep it consistent-no bingeing. One glass of wine a few times a week is usually fine. But if you usually drink on weekends and suddenly stop, your INR can rise. Talk to your doctor about your habits.
How often should I get my INR checked?
When you first start warfarin, you’ll need checks every few days to a week. Once your dose and diet are stable, most people test every 2-4 weeks. But if you’ve had recent INR swings, changed your diet, started a new medication, or feel unwell, get tested sooner. Your pharmacist or anticoagulation clinic will tell you the right schedule.
Can I take a vitamin K supplement to stabilize my INR?
Only under medical supervision. Some patients with unstable INR benefit from a daily 150 µg vitamin K supplement-but only if their doctor or pharmacist recommends it. Taking it without guidance can make your warfarin dose too low, increasing clot risk. Never start or stop supplements on your own.
Why do some people say to avoid vitamin K altogether?
That advice is outdated. Ten years ago, doctors often told patients to avoid vitamin K-rich foods. But research since 2015 has shown that restriction causes more harm than good. It leads to unstable INR, bone loss, and unnecessary fear around healthy foods. Major guidelines from the American College of Chest Physicians and the American Heart Association now say: avoid restriction. Focus on consistency.
What should I do if my INR is too high or too low?
Don’t change your warfarin dose yourself. Call your doctor or anticoagulation clinic immediately. They may ask you to skip a dose, adjust your next one, or come in for a blood test. If you’re bleeding or have chest pain, go to the ER. But for most INR changes, the fix is simple: stabilize your diet and retest in a few days.
Write a comment
Items marked with * are required.




8 Comments
Inna Borovik December 5, 2025 AT 22:33
Let’s be real - this post is just a glorified USDA pamphlet with extra steps. You’re telling people to measure spinach like it’s cocaine? Most folks don’t have time for this. My INR’s been stable for 7 years eating whatever I want. If your doctor can’t adjust your dose for a salad, they’re not doing their job.
Rashmi Gupta December 6, 2025 AT 22:28
Wow. Just… wow. So now we’re supposed to become vitamin K accountants? Next they’ll ask us to log our oxygen intake. This is medical gaslighting disguised as ‘empowerment.’ You want consistency? Then fix the drug. Don’t make the patient become a walking nutrition app.
Geraldine Trainer-Cooper December 8, 2025 AT 05:32
predictability over perfection
that’s the whole damn point
you don’t need to be perfect
just don’t be a chaos gremlin
Akash Takyar December 9, 2025 AT 10:15
This is one of the most thoughtful, evidence-based explanations I’ve seen on this topic. As someone who’s managed warfarin for over a decade, I can confirm that consistency - not restriction - is the true key. Many patients panic when they hear ‘vitamin K,’ but the real danger lies in unpredictability. I’ve seen friends crash their INR after avoiding greens for weeks, then eating a single large kale smoothie. It’s not the food. It’s the swing. Thank you for emphasizing the science, not the fear.
Mayur Panchamia December 9, 2025 AT 21:58
Bro, this is why India’s healthcare system is better than yours - we don’t need apps to tell us how much spinach to eat. My uncle’s been on warfarin since 2003, eats 3 cups of spinach daily, never checks his INR, and still runs marathons. You Americans overcomplicate everything. If your body can’t handle a little kale, maybe you shouldn’t be on warfarin in the first place. Stop micro-managing your diet and start trusting your body - and your doctor.
Karen Mitchell December 10, 2025 AT 16:51
It is deeply concerning that this post normalizes the commodification of patient health through algorithmic dietary compliance. The very notion that one’s biological stability should be contingent upon the rigid quantification of leafy greens reflects a systemic failure of medical ethics - one that prioritizes administrative convenience over holistic care. One cannot reduce human physiology to a spreadsheet. This is not medicine. This is surveillance dressed in nutritional jargon.
Nava Jothy December 10, 2025 AT 21:30
I’ve been on warfarin for 12 years… and I cried when I found out I could eat kale again 😭
My pharmacist gave me a little chart… I eat 1 cup of spinach every Tuesday and Thursday… no more panic… no more 3am INR anxiety…
It’s not about being perfect… it’s about being predictable…
and now I’m actually living… not just surviving…
thank you for this post… I’m not alone 💕
Andrew Frazier December 11, 2025 AT 05:25
lol at all these people acting like this is rocket science. you eat greens, you get your blood drawn. you eat less greens, you get your blood drawn. you eat more, same thing. stop overthinking it. if you’re too lazy to eat the same damn food every week, maybe you shouldn’t be on a blood thinner. also, who the hell uses warframate? that’s a 2018 app. my grandma uses pen and paper. she’s got better control than you.